Angiodysplasia of the colon and small intestine
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
haemodynamically unstable (severe haemorrhage)
CT angiography + mesenteric angiography with embolisation
In patients with unstable angiodysplastic bleeding, guidelines recommend CT angiography as the initial test to assess the arterial anatomy and localise the bleeding point.[18]Sengupta N, Kastenberg DM, Bruining DH, et al. The role of imaging for GI bleeding: ACG and SAR consensus recommendations. Radiology. 2024 Mar;310(3):e232298. http://www.ncbi.nlm.nih.gov/pubmed/38441091?tool=bestpractice.com [35]Sengupta N, Feuerstein JD, Jairath V, et al. Management of patients with acute lower gastrointestinal bleeding: an updated ACG guideline. Am J Gastroenterol. 2023 Feb 1;118(2):208-31. https://journals.lww.com/ajg/fulltext/2023/02000/management_of_patients_with_acute_lower.14.aspx http://www.ncbi.nlm.nih.gov/pubmed/36735555?tool=bestpractice.com [38]Triantafyllou K, Gkolfakis P, Gralnek IM, et al. Diagnosis and management of acute lower gastrointestinal bleeding: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2021 Aug;53(8):850-68. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-1496-8969 http://www.ncbi.nlm.nih.gov/pubmed/34062566?tool=bestpractice.com This should be followed by a mesenteric angiography with a view to embolisation to control the source of bleeding.
supportive care
Treatment recommended for ALL patients in selected patient group
Intravenous access should be attained, preparing for replacement of fluid and blood loss with intravenous fluids and blood transfusions. Blood typing and cross-match with serial full blood counts are recommended to assess fluid status.
interventional upper endoscopy
An upper gastrointestinal endoscopy may be performed to rule out a source proximal to the distal duodenum. During this procedure, electrocautery, photocoagulation, clips, or an epinephrine (adrenaline) injection may be indicated to treat the lesion.
supportive care
Treatment recommended for ALL patients in selected patient group
Intravenous access should be attained, preparing for replacement of fluid and blood loss with intravenous fluids and blood transfusions. Blood typing and cross-match with serial full blood counts are recommended to assess fluid status.
colonoscopy, device-assisted enteroscopy, and/or surgery
Colonoscopy or surgery may be appropriate in the absence of angiography. A colonoscopy is recommended to identify a lower gastrointestinal source of bleeding and to provide treatment. During this procedure, electrocautery, photocoagulation, clips, or an adrenaline (epinephrine) injection may be indicated to treat the lesion.
Careful treatment in the right colon is recommended, due to the thinner walls and higher risk for perforation.
Electrocautery uses heated probes to coagulate the bleeding lesions. Photocoagulation uses argon and Yag lasers and requires specific training.
[Figure caption and citation for the preceding image starts]: Endoscopic (device-assisted enteroscopy) image of small bowel angiodysplasia after treatment with argon plasma coagulationFrom the personal collection of Dr Elli, Milan, Italy; used with permission [Citation ends].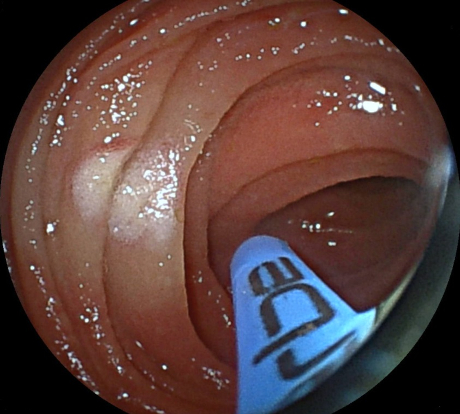 [Figure caption and citation for the preceding image starts]: Endoscopic image of argon plasma coagulation of colonic angiodysplasiaPermission obtained from patient; GNU Free Documentation License [Citation ends].
[Figure caption and citation for the preceding image starts]: Endoscopic image of argon plasma coagulation of colonic angiodysplasiaPermission obtained from patient; GNU Free Documentation License [Citation ends].
If the colonoscopy is negative and a small bowel source is suspected, device-assisted enteroscopy can be used to identify and treat the bleeding lesions. This can be done via the oral or retrograde route depending on the location of the suspected lesion in the small bowel.
Only patients with a large, life-threatening haemorrhage with little relief from interventional endoscopy or embolisation are appropriate for surgery.
At operation, if the patient is unstable, an on-table enteroscopy or blind sub-total colectomy may be appropriate.
Aortic valve replacement should be considered in patients with Heyde’s syndrome and ongoing bleeding.[8]Gerson LB, Fidler JL, Cave DR, et al. ACG clinical guideline: diagnosis and management of small bowel bleeding. Am J Gastroenterol. 2015 Sep;110(9):1265-87; quiz 1288. https://journals.lww.com/ajg/fulltext/2015/09000/acg_clinical_guideline__diagnosis_and_management.10.aspx http://www.ncbi.nlm.nih.gov/pubmed/26303132?tool=bestpractice.com
supportive care
Treatment recommended for ALL patients in selected patient group
Intravenous access should be attained, preparing for replacement of fluid and blood loss with intravenous fluids and blood transfusions. Blood typing and cross-match with serial full blood counts are recommended to assess fluid status.
haemodynamically stable
interventional endoscopy
During the endoscopy, electrocautery, photocoagulation, clips, or an adrenaline (epinephrine) injection may be indicated to treat the lesion.
Careful treatment in the right colon is recommended, due to the thinner walls and higher risk for perforation.
Electrocautery uses heated probes to coagulate the bleeding lesions. Photocoagulation uses argon and Yag lasers and requires specific training.[Figure caption and citation for the preceding image starts]: Endoscopic (device-assisted enteroscopy) image of small bowel angiodysplasia after treatment with argon plasma coagulationFrom the personal collection of Dr Elli, Milan, Italy; used with permission [Citation ends].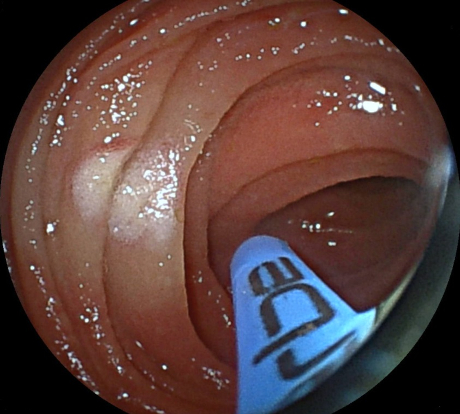 [Figure caption and citation for the preceding image starts]: Endoscopic image of argon plasma coagulation of colonic angiodysplasiaPermission obtained from patient; GNU Free Documentation License [Citation ends].
[Figure caption and citation for the preceding image starts]: Endoscopic image of argon plasma coagulation of colonic angiodysplasiaPermission obtained from patient; GNU Free Documentation License [Citation ends].
supportive care
Additional treatment recommended for SOME patients in selected patient group
Intravenous access should be attained, preparing for replacement of fluid and blood loss with intravenous fluids and blood transfusions. Blood typing and cross-match with serial full blood counts are recommended to assess fluid status.
The European Society of Gastrointestinal Endoscopy recommends red blood cell transfusion in haemodynamically stable patients with acute lower gastrointestinal bleeding and no history of cardiovascular disease, with a haemoglobin threshold of ≤ 70 g/L (≤ 7 g/dL) prompting red blood cell transfusion.[38]Triantafyllou K, Gkolfakis P, Gralnek IM, et al. Diagnosis and management of acute lower gastrointestinal bleeding: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2021 Aug;53(8):850-68. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-1496-8969 http://www.ncbi.nlm.nih.gov/pubmed/34062566?tool=bestpractice.com In those with a history of cardiovascular disease, a haemoglobin threshold of ≤ 80 g/dL (≤ 8 g/dL) should prompt red blood cell transfusion.[38]Triantafyllou K, Gkolfakis P, Gralnek IM, et al. Diagnosis and management of acute lower gastrointestinal bleeding: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2021 Aug;53(8):850-68. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-1496-8969 http://www.ncbi.nlm.nih.gov/pubmed/34062566?tool=bestpractice.com
wireless capsule enteroscopy or CT angiography + mesenteric angiography with embolisation or enteroscopy
If the endoscopy is negative and the bleeding continues, based on local expertise, capsule endoscopy or CT angiography should be performed which may guide further intervention. If CT angiography confirms active bleeding, it should be followed by a mesenteric angiography with a view to embolisation to treat the bleeding or endoscopic management using device-assisted enteroscopy if a small bowel source is seen.[40]Raju GS, Gerson L, Das A, et al. American Gastroenterological Association (AGA) Institute medical position statement on obscure gastrointestinal bleeding. Gastroenterology. 2007 Nov;133(5):1697-717.
http://www.gastrojournal.org/article/S0016-5085%2807%2901148-1/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/17983812?tool=bestpractice.com
[51]National Institute for Health and Care Excellence. Wireless capsule endoscopy for investigation of the small bowel. Dec 2004 [internet publication].
https://www.nice.org.uk/guidance/ipg101
[Figure caption and citation for the preceding image starts]: Small bowel angiodysplasia seen during small bowel capsule endoscopyFrom the personal collection of Dr Elli, Milan, Italy; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Small bowel angiodysplasia seen during small bowel capsule endoscopyFrom the personal collection of Dr Elli, Milan, Italy; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Small bowel angiodysplasia seen during small bowel capsule endoscopyFrom the personal collection of Dr Elli, Milan, Italy; used with permission [Citation ends].
supportive care
Additional treatment recommended for SOME patients in selected patient group
Intravenous access should be attained, preparing for replacement of fluid and blood loss with intravenous fluids and blood transfusions. Blood typing and cross-match with serial full blood counts are recommended to assess fluid status.
The European Society of Gastrointestinal Endoscopy recommends red blood cell transfusion in haemodynamically stable patients with acute lower gastrointestinal bleeding and no history of cardiovascular disease, with a haemoglobin threshold of ≤ 70 g/L (≤ 7 g/dL) prompting red blood cell transfusion.[38]Triantafyllou K, Gkolfakis P, Gralnek IM, et al. Diagnosis and management of acute lower gastrointestinal bleeding: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2021 Aug;53(8):850-68. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-1496-8969 http://www.ncbi.nlm.nih.gov/pubmed/34062566?tool=bestpractice.com In those with a history of cardiovascular disease, a haemoglobin threshold of ≤ 80 g/L (≤ 8 g/dL) should prompt red blood cell transfusion.[38]Triantafyllou K, Gkolfakis P, Gralnek IM, et al. Diagnosis and management of acute lower gastrointestinal bleeding: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2021 Aug;53(8):850-68. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-1496-8969 http://www.ncbi.nlm.nih.gov/pubmed/34062566?tool=bestpractice.com
surgery
If angiography is unsuccessful or unavailable and the patient is a surgical candidate, surgery can be considered. Surgery should not be used as a diagnostic tool to localise the site of bleeding in haemodynamically stable patients.[34]Karuppasamy K, Kapoor BS, Fidelman N, et al. Expert panel on interventional radiology, ACR appropriateness criteria® radiologic management of lower gastrointestinal tract bleeding: 2021 update. J. Am. Coll. Radiol. 2021 May 21;18(5):S139-52. https://www.jacr.org/article/S1546-1440(21)00153-8/fulltext http://www.ncbi.nlm.nih.gov/pubmed/33958109?tool=bestpractice.com The exact procedure used will depend on the likely site(s) of the bleeding based on preoperative and intraoperative investigations.
supportive care
Additional treatment recommended for SOME patients in selected patient group
Intravenous access should be attained, preparing for replacement of fluid and blood loss with intravenous fluids and blood transfusions. Blood typing and cross-match with serial full blood counts are recommended to assess fluid status.
The European Society of Gastrointestinal Endoscopy recommends red blood cell transfusion in haemodynamically stable patients with acute lower gastrointestinal bleeding and no history of cardiovascular disease, with a haemoglobin threshold of ≤ 70 g/L (≤ 7 g/dL) prompting red blood cell transfusion.[38]Triantafyllou K, Gkolfakis P, Gralnek IM, et al. Diagnosis and management of acute lower gastrointestinal bleeding: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2021 Aug;53(8):850-68. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-1496-8969 http://www.ncbi.nlm.nih.gov/pubmed/34062566?tool=bestpractice.com In those with a history of cardiovascular disease, a haemoglobin threshold of ≤ 80 g/L (≤ 8 g/dL) should prompt red blood cell transfusion.[38]Triantafyllou K, Gkolfakis P, Gralnek IM, et al. Diagnosis and management of acute lower gastrointestinal bleeding: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2021 Aug;53(8):850-68. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-1496-8969 http://www.ncbi.nlm.nih.gov/pubmed/34062566?tool=bestpractice.com
pharmacological therapy
If angiography is unsuccessful or unavailable and if the patient is not a surgical candidate, then pharmacological therapy may be considered. One systematic review and meta-analysis found that pharmacological treatment led to significantly reduced bleeding episodes and notable improvement in haemoglobin levels.[66]Gkolfakis P, Fostier R, Tziatzios G, et al. Efficacy of pharmacologic treatment for treating gastrointestinal angiodysplasias-related bleeding: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2022 Oct 1;34(10):1021-30. http://www.ncbi.nlm.nih.gov/pubmed/35913758?tool=bestpractice.com Somatostatin analogues (e.g., octreotide, lanreotide) and thalidomide have shown benefit in this setting. There is poor evidence for oestrogen derivatives. One multi-centre randomised controlled trial found that octreotide reduced transfusion requirements and the annual volume of endoscopic procedures in patients with angiodysplasia-related anaemia.[69]Goltstein LCMJ, Grooteman KV, Bernts LHP, et al. Standard of care versus octreotide in angiodysplasia-related bleeding (the OCEAN study): a multicenter randomized controlled trial. Gastroenterology. 2024 Apr;166(4):690-703. https://www.gastrojournal.org/article/S0016-5085(23)05685-8/fulltext http://www.ncbi.nlm.nih.gov/pubmed/38158089?tool=bestpractice.com Long-term lanreotide therapy has shown to significantly improve anaemia and reduce hospitalisations, blood transfusions, and endoscopies in patients with angiodysplasias.[70]Frago S, Alcedo J, Martín Pena-Galo E, et al. Long-term results with lanreotide in patients with recurrent gastrointestinal angiodysplasias bleeding or obscure gastrointestinal bleeding. Benefits in efficacy and procedures consumption. Scand J Gastroenterol. 2018 Dec;53(12):1496-502. http://www.ncbi.nlm.nih.gov/pubmed/30621520?tool=bestpractice.com [71]Hawks MK, Svarverud JE. Acute lower gastrointestinal bleeding: evaluation and management. Am Fam Physician. 2020 Feb 15;101(4):206-12. https://www.aafp.org/pubs/afp/issues/2020/0215/p206.html http://www.ncbi.nlm.nih.gov/pubmed/32053333?tool=bestpractice.com Systematic reviews suggest that somatostatin analogue therapy is safe and effective in patients with gastrointestinal angiodysplasia; octreotide therapy may be more effective than lanreotide therapy.[72]Jackson CS, Gerson LB. Management of gastrointestinal angiodysplastic lesions (GIADs): a systematic review and meta-analysis. Am J Gastroenterol. 2014 Apr;109(4):474-83. https://www.ncbi.nlm.nih.gov/books/NBK196085 http://www.ncbi.nlm.nih.gov/pubmed/24642577?tool=bestpractice.com [73]Goltstein LCMJ, Grooteman KV, Rocco A, et al. Effectiveness and predictors of response to somatostatin analogues in patients with gastrointestinal angiodysplasias: a systematic review and individual patient data meta-analysis. Lancet Gastroenterol Hepatol. 2021 Nov;6(11):922-32. https://www.doi.org/10.1016/S2468-1253(21)00262-4 http://www.ncbi.nlm.nih.gov/pubmed/34508668?tool=bestpractice.com One retrospective study reported that somatostatin analogue therapy plus endoscopic therapy reduced bleeding episodes in patients with recurrent anaemia and small bowel angioectasia.[47]Tai FWD, Chetcuti-Zammit S, Sidhu R. Small bowel angioectasia-the clinical and cost impact of different management strategies. Clin Res Hepatol Gastroenterol. 2023 Oct;47(8):102193. http://www.ncbi.nlm.nih.gov/pubmed/37553067?tool=bestpractice.com
Primary options
octreotide: consult specialist for guidance on dose
OR
lanreotide: consult specialist for guidance on dose
OR
thalidomide: consult specialist for guidance on dose
supportive care
Additional treatment recommended for SOME patients in selected patient group
Intravenous access should be attained, preparing for replacement of fluid and blood loss with intravenous fluids and blood transfusions. Blood typing and cross-match with serial full blood counts are recommended to assess fluid status.
The European Society of Gastrointestinal Endoscopy recommends red blood cell transfusion in haemodynamically stable patients with acute lower gastrointestinal bleeding and no history of cardiovascular disease, with a haemoglobin threshold of ≤ 70 g/L (≤ 7 g/dL) prompting red blood cell transfusion.[38]Triantafyllou K, Gkolfakis P, Gralnek IM, et al. Diagnosis and management of acute lower gastrointestinal bleeding: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2021 Aug;53(8):850-68. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-1496-8969 http://www.ncbi.nlm.nih.gov/pubmed/34062566?tool=bestpractice.com In those with a history of cardiovascular disease, a haemoglobin threshold of ≤ 80 g/L (≤ 8 g/dL) should prompt red blood cell transfusion.[38]Triantafyllou K, Gkolfakis P, Gralnek IM, et al. Diagnosis and management of acute lower gastrointestinal bleeding: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2021 Aug;53(8):850-68. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-1496-8969 http://www.ncbi.nlm.nih.gov/pubmed/34062566?tool=bestpractice.com
recurrent bleed
repeat interventional endoscopy
If bleeding continues, a repeat endoscopy is recommended with therapeutic intervention. During the procedure, electrocautery, photocoagulation, clips, or an adrenaline (epinephrine) injection may be indicated to treat the lesion.
For patients with colonic angiodysplasias, careful treatment in the right colon is recommended, due to the thinner walls and higher risk for perforation.
For patients with recurrent small bowel bleeding, endoscopic management with device-assisted enteroscopy can be considered depending on the patient’s clinical course and response to prior therapy.[8]Gerson LB, Fidler JL, Cave DR, et al. ACG clinical guideline: diagnosis and management of small bowel bleeding. Am J Gastroenterol. 2015 Sep;110(9):1265-87; quiz 1288. https://journals.lww.com/ajg/fulltext/2015/09000/acg_clinical_guideline__diagnosis_and_management.10.aspx http://www.ncbi.nlm.nih.gov/pubmed/26303132?tool=bestpractice.com
Electrocautery uses heated probes to coagulate the bleeding lesions. Photocoagulation uses argon and Yag lasers and requires specific training.[Figure caption and citation for the preceding image starts]: Endoscopic (device-assisted enteroscopy) image of small bowel angiodysplasia after treatment with argon plasma coagulationFrom the personal collection of Dr Elli, Milan, Italy; used with permission [Citation ends].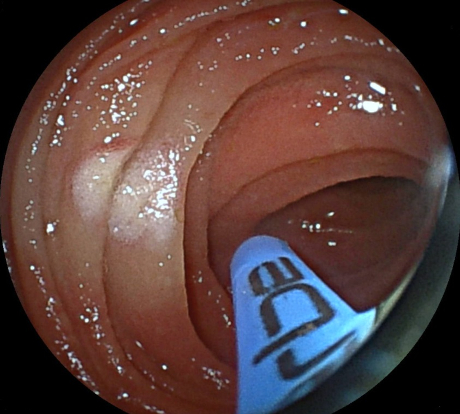 [Figure caption and citation for the preceding image starts]: Endoscopic image of argon plasma coagulation of colonic angiodysplasiaPermission obtained from patient; GNU Free Documentation License [Citation ends].
[Figure caption and citation for the preceding image starts]: Endoscopic image of argon plasma coagulation of colonic angiodysplasiaPermission obtained from patient; GNU Free Documentation License [Citation ends].

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer