Approach
The diagnosis of osteosarcoma should be considered in any patient that presents with bone pain, particularly if they are in the first or second decade of life. Rarely, patients older than this can be affected, although these cases tend to be secondary osteosarcomas related to previous radiotherapy or a history of Paget's disease.
Patients aged 40 years and under with an abnormal radiograph should be referred to an orthopaedic oncologist, whereas patients aged 40 years or older with an abnormal radiograph should be assessed for potential bone metastases.[23] People found to have primary bone cancer should be referred to an orthopaedic oncologist, for those who have secondary bone metastases, referral to an appropriate specialist for the primary site of cancer is recommended.[23]
Physical examination
The exact physical findings of osteosarcoma depend on the location of the tumour. Pain, swelling, limping, or limited range of motion are the most common symptoms and should raise suspicion for the possibility of a bone tumour.[2][14] Local swelling with associated skin warmth and occasionally ulceration can be seen in the affected area.
Rarely, patients may present with pathological fractures, which are common in purely lytic tumours such as telangiectatic osteosarcoma. Symptoms associated with metastatic disease (mainly pulmonary) may also form part of the clinical picture.
Initial test
Conventional radiography is the first-line diagnostic test for osteosarcoma.[23] These radiographs typically show a radiolucent lesion with areas of mottled radiodensity and ill-defined margins. The neoplasm is usually located in the metaphysis of a long bone. Reactive new bone formation under the periosteum can be seen as Codman's triangle or can give a characteristic sunburst appearance. Sometimes a soft tissue mass can be appreciated on conventional radiographs.[24]
If radiographs are reported as negative but symptoms persist or worsen, a computed tomography (CT) or magnetic resonance imaging (MRI) scan is indicated.[Figure caption and citation for the preceding image starts]: Conventional radiograph, anteroposterior view; poorly circumscribed, permeative lesion involving distal femoral metaphysis with mixed radiodense and radiolucent appearance; a large soft tissue mass with periosteal reaction is also presentPersonal collections of Dr Michael J. Klein and Dr Luminita Rezeanu [Citation ends].
Biopsy
Histological examination of tumour material is the definitive diagnostic test.[23] Biopsies should be taken as part of the initial workup for patients aged 40 years and under, or after local staging in patients aged 40 years and over.[23] Guidelines recommend consultation with an orthopaedic oncologist on appropriate pre-biopsy imaging.[23]
Core needle or open biopsy at a centre specialised in the management of osteosarcoma are recommended.[23] Fine-needle aspiration and excisional biopsies are not recommended. Tissue should be submitted for pathological assessment as quickly as possible. Tumour imprints (touch preps) can be taken, and tissue should be snap-frozen and/or sent for cytogenetic analysis.
Tumour banks are useful for diagnosis and translational research into the molecular pathology of cancer; therefore, informed consent for tumour banking should be sought that allows for later analysis and research according to local practice.[25] Preferably, the same clinician should perform both the biopsy and the subsequent resection.[26] To reduce the risk of tumour seeding by the biopsy process, the biopsy needle tract or scar is removed with the subsequent resection.
Staging
Recommended tests to establish the stage of osteosarcoma include:[23]
MRI and/or CT with contrast of the primary site
Chest CT (with or without contrast)
Whole-body fluorodeoxyglucose (FDG)-PET/CT and/or bone scan
MRI (with and without contrast) or CT (with contrast) of skeletal metastatic sites.
Local staging
MRI and CT are equally accurate for local staging. In a study of 387 patients with osteosarcoma or Ewing’s sarcoma, there was no statistically significant difference between the 2 modalities in determining local tumour extent.[27] MRI is usually favoured due to its sensitivity to soft tissue contrast, multi-planar capabilities, and lack of radiation exposure. MRI can also assess growth plate penetration, joint space invasion, whether the tumour encases and displaces the adjacent neurovascular bundle, and whether there is invasion of the adjacent muscles. Therefore, the region assessed by MRI should include the whole involved bone as well as the neighbouring joints.[25] CT is useful to reveal minimal matrix production and periosteal reaction in tumours with unusual locations and is clearly superior to conventional radiographs for detecting lung metastases.[27][Figure caption and citation for the preceding image starts]: Computed tomographic scan, axial view; osteosarcoma of proximal tibia; matrix production and bone destruction are best appreciated on conventional tomographsPersonal collections of Dr Michael J. Klein and Dr Luminita Rezeanu [Citation ends].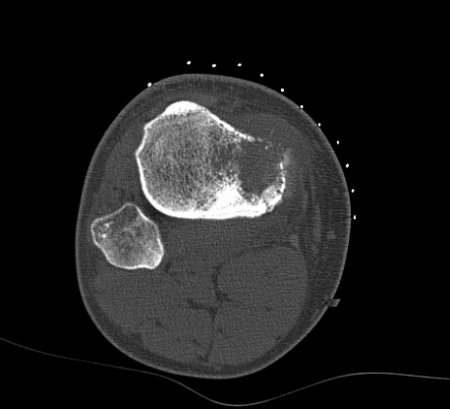 [Figure caption and citation for the preceding image starts]: Magnetic resonance imaging, coronal view; osteosarcoma of distal femur showing low-intensity signal; T1-weighted image; actual intra-osseous and extra-osseous tumour extent is also appreciatedPersonal collections of Dr Michael J. Klein and Dr Luminita Rezeanu [Citation ends].
[Figure caption and citation for the preceding image starts]: Magnetic resonance imaging, coronal view; osteosarcoma of distal femur showing low-intensity signal; T1-weighted image; actual intra-osseous and extra-osseous tumour extent is also appreciatedPersonal collections of Dr Michael J. Klein and Dr Luminita Rezeanu [Citation ends].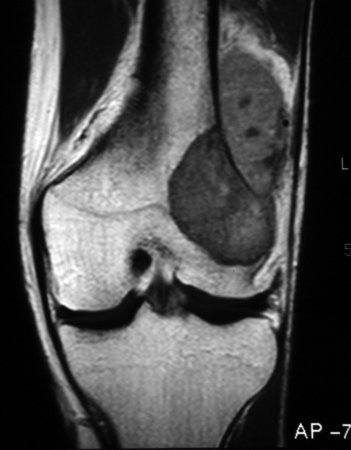 [Figure caption and citation for the preceding image starts]: Magnetic resonance imaging, axial view; osteosarcoma of distal femur showing high-intensity signal; T2-weighted imagePersonal collections of Dr Michael J. Klein and Dr Luminita Rezeanu [Citation ends].
[Figure caption and citation for the preceding image starts]: Magnetic resonance imaging, axial view; osteosarcoma of distal femur showing high-intensity signal; T2-weighted imagePersonal collections of Dr Michael J. Klein and Dr Luminita Rezeanu [Citation ends].
Systemic staging
Systemic staging after a confirmed diagnosis focuses on the main sites of metastasis, the lungs and the skeleton.
Investigations include CT scans of the lungs and thorax, whole-body FDG-positron emission tomography/CT (FDG-PET/CT), and/or bone scan to detect potential skip lesions or distant metastases identified by primary imaging.[23] MRI (with and without contrast) or CT (with contrast) are recommended of the skeletal metastatic sites.[23]
Appropriate imaging of the primary tumour or resectable metastases must be repeated before surgery.[23]
Laboratory investigations
Recommended laboratory investigations include:[23]
Full blood count
Alkaline phosphatase
Lactate dehydrogenase.
Elevated alkaline phosphatase and lactate dehydrogenase levels may correlate with adverse effects.[25] Measurement of alkaline phosphatase is useful to monitor for recurrences after treatment.[2][14][27][28]
Results of the tests may be relevant in the diagnosis, prognosis, and management of bone sarcoma patients and should be done prior to definitive treatment and periodically during treatment and surveillance.[23]
Additional investigations
Female patients should have a consultation with a fertility physician about potential ovarian sampling and cryopreservation; use of gonadotrophin-releasing hormone agonists and other means of ovarian suppression for fertility preservation should be considered, where available.[23][25]
Sperm storage is recommended for men of reproductive age.[25][Figure caption and citation for the preceding image starts]: Bone scan; high radionuclide uptake at tumour sitePersonal collections of Dr Michael J. Klein and Dr Luminita Rezeanu [Citation ends].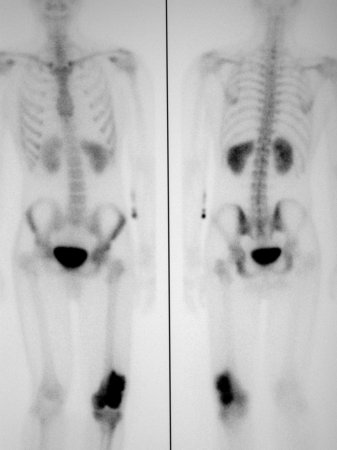
Chemotherapy treatment for osteosarcoma can result in cardiac and auditory dysfunction, a baseline assessment by echocardiogram or radionuclide ventriculography along with an audiogram is advisable.
Further tests before systemic therapy might include blood group typing, coagulation profile, serum electrolytes including magnesium and phosphate, renal and liver function tests, and hepatitis and HIV testing.
Individual patient and family history should be considered for genetic consultation and testing.[23]
Use of this content is subject to our disclaimer