Differentials
Common
Transposition of great arteries
History
incidence is higher in male infants and infants of diabetic mothers; cyanosis appears within the first 24 hours, sometimes with no respiratory distress; if transposition of great arteries is present with an intact ventricular septum, the infant will be very cyanotic, requiring immediate intervention
Exam
prominent right ventricular heave and a single second heart sound (a loud A2) are usually present; a systolic murmur due to increased pulmonary blood flow may be heard in a few cases
1st investigation
- echocardiogram:
definitive diagnostic test; reveals abnormal position of the aorta and pulmonary arteries, abnormal cardiac anatomy and function
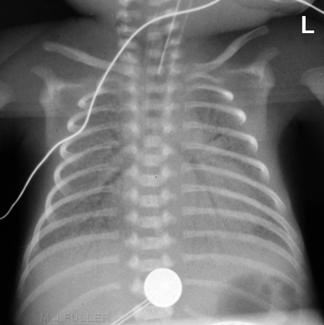
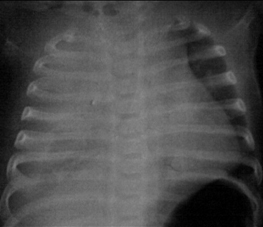
- chest x-ray:
'egg on a string' appearance; slight cardiomegaly and increased pulmonary vascular markings
Other investigations
- ABG:
low PaO₂ with normal PaCO₂ and pH
Tetralogy of Fallot
History
cyanosis depends on the degree of right ventricular outflow tract obstruction, which ranges from very mild to severe; the age of symptom onset is variable; VACTERL (vertebral anomalies, imperforate anus, cardiac lesions, tracheo-oesophageal fistula, renal and limb anomalies) are seen in approximately 15% of infants who have tetralogy of Fallot; infants may be referred for mild cyanosis or presence of a murmur at birth
Exam
prominent right ventricular heave and systolic ejection murmur at left sternal border are usually present
1st investigation
- chest x-ray:
boot-shaped heart
- echocardiogram:
diagnostic study revealing characteristic cardiac anatomy and function
Other investigations
- ECG:
right ventricular hypertrophy
Pulmonary atresia
History
variable presentation depends on the presence of ventricular septal defect and atrial septal defect for adequate mixing of blood at the atrial or ventricular level; mild to moderate cyanosis becomes worse when ductus arteriosus closes
Exam
murmur of patent ductus arteriosus is the only common finding
1st investigation
- chest x-ray:
may reveal decreased pulmonary vascular markings
- echocardiogram:
definitive diagnostic test that reveals pulmonary atresia, abnormal cardiac anatomy and function
Other investigations
- ECG:
peaked P waves in lead II due to right atrial enlargement and mild left axis deviation
Respiratory distress syndrome (RDS)
History
generally occurs in preterm infants due to surfactant deficiency; antenatal history may reveal immature lung profile in the amniotic fluid; higher incidence has been noted in infants of diabetic mothers; full-term infants with RDS have been reported to have surfactant protein B deficiency or adenosine triphosphate-binding cassette, sub-family A (ABCA3) mutations; majority of preterm infants with RDS are born to mothers who did not receive antenatal corticosteroids; delivery of previous sibling with RDS
Exam
tachypnoea, nasal flaring, grunting, and retractions with cyanosis; in severe cases, diminished air entry is present on chest auscultation
1st investigation
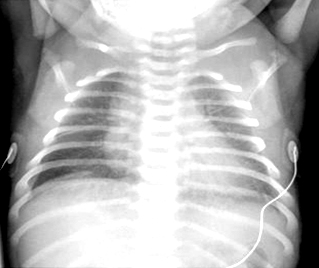
- chest x-ray:
reticular granularity, air bronchograms; in severe cases, decreased lung volume
More
Other investigations
- ABG:
low PaO₂ and a high PaCO₂ may be seen
Transient tachypnoea of the newborn
History
higher incidence among full-term newborns born by elective caesarean section; tachypnoea is the presenting symptom with increased FiO₂ requirement; self-limiting problem; generally resolves within the first 3 days; cyanosis may occur in severe cases
Exam
tachypnoeic infant with reasonable air entry bilaterally upon auscultation
1st investigation
- chest x-ray:
good lung volume with perihilar markings along with fissural fluid markings on the right horizontal fissure
More
Other investigations
- ABG:
mild hypoxia with normal or slightly elevated PaCO₂
Persistent pulmonary hypertension of the newborn (PPHN)
History
occurs in full-term, post-term, or preterm infants commonly; aetiology is variable; risk factors include history of asphyxia, meconium aspiration syndrome, sepsis, congenital diaphragmatic hernia (CDH), pulmonary hypoplasia
Exam
loud S2 and right ventricular heave
1st investigation
- chest x-ray:
depends on the precipitating factors, such as meconium aspiration syndrome, sepsis/pneumonia, CDH
- echocardiogram:
definitive diagnostic test; reveals elevated pulmonary artery pressure, tricuspid regurgitation, altered right ventricular size and function
Other investigations
Pneumothorax
History
can occur spontaneously at birth in full-term newborns or following resuscitation with positive pressure ventilation; occurs frequently in preterm infants with respiratory distress syndrome; assisted ventilation and continuous positive airway pressure contribute to the development of pneumothorax; higher incidence in meconium aspiration syndrome, pulmonary hypoplasia, and congenital diaphragmatic hernia
Exam
tachypnoea and cyanosis are usually present; depending on severity (proportionate to the amount of free air in the pleural space), breath sounds and heart sounds may be faint/distant; mediastinal shift to the contralateral side may occur; transillumination of the chest will be positive in most cases
1st investigation
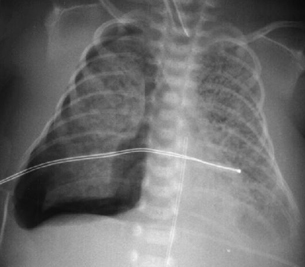
- chest x-ray:
mediastinal shift towards contralateral lung; linear shadow of visceral pleura with lack of lung markings
More
Other investigations
Aspiration pneumonia
History
may be due to meconium aspiration syndrome, blood, milk aspiration, or amniotic fluid; meconium aspiration is commonly seen in post-term infants and those who develop fetal distress; a history of thick meconium-stained amniotic fluid at the time of rupture of membranes is characteristic; most infants become symptomatic with respiratory distress at birth; in the case of blood aspiration, there may be a history of antepartum haemorrhage; in the case of milk aspiration, emesis following feeding and subsequent development of respiratory distress is usually present
Exam
tachypnoea, grunting, retractions, and cyanosis are present; on auscultation diminished air entry, rales, and rhonchi may be evident
1st investigation
- chest x-ray:
patchy and interstitial infiltrates; perihilar markings
More - ABG:
low PaO₂ and high PaCO₂ may be present
Other investigations
Pneumonia
History
risk factors include a history of prolonged rupture of membranes, chorioamnionitis, or positive maternal group B beta streptococcus (GBS) screen; congenital pneumonia due to viruses or bacteria is rare; early-onset GBS sepsis may present as GBS pneumonia with apnoea and circulatory collapse within the first week of life
Exam
respiratory distress with tachypnoea, retractions, and grunting may be present; auscultation often reveals rales, rhonchi, and diminished air entry in a few cases; apnoea may be the only presenting symptom in some cases
1st investigation
- chest x-ray:
diagnostic in most cases but early-onset GBS sepsis may have features of respiratory distress syndrome on x-ray
- FBC:
abnormal; leukopenia or neutropenia with thrombocytopenia may be present; increased amounts of immature neutrophils leading to abnormal I:T (immature to total neutrophil count) ratio (>0.2) is present in most cases
- blood culture:
may be positive
Other investigations
Pulmonary oedema
History
generally due to congestive cardiac failure; underlying cardiac disease, arteriovenous (AV) malformation, or severe anaemia may be present
Exam
tachypnoea, tachycardia, and hepatomegaly are usually present; severe pallor or signs of AV malformation present (bruit)
1st investigation
- chest x-ray:
fluffy infiltrates or hazy lung fields and associated cardiomegaly
Other investigations
- ABG:
hypoxia and mild hypercarbia
- echocardiogram:
diagnostic for congenital cardiac lesions
- FBC:
normal or severe anaemia
Congenital diaphragmatic hernia
History
most cases are diagnosed by antenatal ultrasound; more common on the left side; most cases are symptomatic at birth with severe cyanosis; some have minimal symptoms and are diagnosed later in the neonatal period or infancy; history of polyhydramnios
Exam
scaphoid abdomen at birth, diminished air entry on the left side of chest, with cyanosis at birth are typical features; heart sounds may not be heard on the left side of chest due to mediastinal shift
1st investigation
- chest x-ray:
diagnostic with intestinal gas pattern in the left hemithorax with mediastinal shift
More - ABG:
severe hypoxia and hypercarbia
Other investigations
- echocardiogram:
pulmonary hypertension; may also show eventration of the diaphragm
Congenital pulmonary airway malformation (CPAM; formerly known as congenital cystic adenomatoid malformation [CCAM])
History
most of these cases are diagnosed by antenatal ultrasound; the severe forms may lead to hydrops in the fetus; milder forms may have mild respiratory distress or no symptoms at birth; many infants are diagnosed in childhood when they present with recurrent infections
Exam
tachypnoea and mild cyanosis are present in many infants; diminished air entry on the affected side will be present
1st investigation
- chest x-ray:
multi-cystic air-filled lesion
More
Other investigations
- CT chest:
may be required to demarcate the extent of the cystic lesion
Upper airway obstruction
History
most become symptomatic shortly after birth with no significant cyanosis; symptoms worsen during feeding, with stridulous breathing; those with vocal cord paralysis will have a weak or non-existent cry; cyanosis may develop; risk of aspiration during feeding; infants with vocal cord paralysis may have central nervous system conditions
Exam
submandibular, suprasternal, and supraclavicular retractions are characteristic of upper airway obstruction; infants with choanal atresia or stenosis may have mild to moderate symptoms depending on whether unilateral or bilateral; inability to pass nasogastric tube is diagnostic
1st investigation
- chest x-ray and lateral view of neck:
sometimes the airway calibre can be demonstrated
Other investigations
- laryngoscopy:
in vocal cord paralysis, laryngoscopy will be diagnostic
- bronchoscopy:
bronchoscopy will be diagnostic for laryngomalacia, tracheal malacia, subglottic stenosis, or laryngeal web
- CT scan of the head and skull:
may demonstrate central nervous system malformations; diagnostic for choanal stenosis or atresia
- flexible nasendoscopy:
anatomical changes of choanal atresia
More
Polycythaemia
History
polycythaemia is common in insulin-dependent diabetes mellitus, small for gestational age infants, and twin-to-twin transfusion; maternal history of diabetes and hypertension during pregnancy are frequent; slightly higher incidence of transient tachypnoea of the newborn may be present
Exam
either large for gestational age or small for gestational age infants who may appear cyanotic but have normal ABGs; some infants may have transient tachypnoea of the newborn or mild persistent pulmonary hypertension of newborn; infants appear ruddy and plethoric, and have a higher incidence of acrocyanosis; clinical examination may be normal or findings of transient tachypnoea of the newborn may be present
1st investigation
- ABG:
normal PaO₂
- chest x-ray:
normal or suggestive of transient tachypnoea of the newborn
- FBC:
diagnostic with haematocrit >70%
Other investigations
Asphyxia
History
history of fetal distress with perinatal asphyxia and low Apgar scores requiring vigorous resuscitation; history of seizures or apnoea may be the presenting symptom; may lead to hypoxic ischaemic encephalopathy
Exam
neurologically depressed, hypotonia, subtle seizure activity, with good aeration to both lung fields; apnoea or hypoventilation (bradypnoea) is the cause for cyanosis
1st investigation
- chest x-ray:
normal
- serum creatinine:
elevated
- liver function tests:
raised alanine aminotransferase
Other investigations
- EEG:
may be abnormal; suggestive of seizure activity
- CT scan of brain:
may indicate cerebral oedema
- FBC:
normal; may have thrombocytopenia
Methaemoglobinaemia (met-Hb)
History
usually well in spite of characteristic skin discoloration, termed pseudocyanosis; condition may worsen with shortness of breath and central nervous system features including seizures; may be congenital or acquired; acquired form may result from exposure to drugs/toxins known to cause met-Hb
Exam
characteristic blue colour, dyspnoea, mental state changes; arterial blood with elevated methaemoglobin levels has a characteristic chocolate-brown colour; pulse oximetry is unreliable
1st investigation
- ABG:
normal PaO₂
More
Other investigations
- chest x-ray:
normal
- multiple wavelength co-oximeter:
direct measurement of met-Hb definite diagnostic test
Hypoglycaemia
History
either a small for gestational age or large for gestational age infant born to a diabetic or hypertensive woman
Exam
may be jittery or may have seizures; clinical examination may be normal or may reveal hypo- or hypertonia; cyanosis is usually due to apnoea or transient persistent pulmonary hypertension of newborn
1st investigation
- blood glucose:
severely hypoglycaemic <1.4 mmol/L (<25 mg/dL)
More
Other investigations
- chest x-ray:
normal
Neonatal sepsis
History
history of premature rupture of membranes, chorioamnionitis, or intrapartum maternal fever may be present; may present with non-specific, non-localised symptoms; fever, low body temperature or temperature instability; lethargy, irritability or non-responsiveness; poor feeding, or emesis; may present with apnoea and cyanosis or with circulatory shock
Exam
tachycardia, tachypnoea, fever (>38℃ [>100.4°F]) or hypothermia (<36℃ [<96.8°F]); infants and young children may be hypotonic with normal or poor peripheral perfusion and hypotension; prolonged capillary refill, mottled or ashen skin, cyanosis, low oxygen saturation, reduced urine output; may be absence of bowel sounds; hypo- or hyperglycaemia may be present
1st investigation
- blood culture:
may be positive for organism
More - serum lactate:
may be elevated
More - FBC with differential:
abnormal WBC count (i.e., above or below normal range for age or >10% immature white cells); low platelets
More - C-reactive protein:
elevated
- blood urea and serum electrolytes:
serum electrolytes may be deranged; blood urea may be elevated
- serum creatinine:
may be elevated
More - liver function tests:
may show elevated bilirubin, alanine aminotransferase, aspartate aminotransferase
- coagulation studies:
may be abnormal
- blood gases:
may be hypoxaemia, hypercapnia, elevated anion gap, metabolic acidosis
Other investigations
- chest x-ray:
may show consolidation; demonstrates position of central venous catheter and tracheal tube
- urine microscopy and culture:
may be positive for nitrites, protein or blood; elevated leukocyte count; positive culture for organism
- lumbar puncture:
presence of organism on microscopy and positive culture
More
Uncommon
Total anomalous pulmonary venous return
History
clinical condition depends on the presence of pulmonary venous obstruction; pulmonary congestion (pulmonary oedema) with respiratory distress and cyanosis can be mistaken for interstitial pneumonitis
Exam
prominent right ventricular heave; widely split S2; systolic ejection murmur at the left upper sternal border may occur; hepatomegaly is common; response to alprostadil (prostaglandin E1) infusion is generally ineffective to minimal
1st investigation
- chest x-ray:
cardiomegaly; 'snowman' pulmonary congestion
More - echocardiogram:
definitive diagnostic test; reveals pulmonary venous drainage, characteristic cardiac anatomy and function
Other investigations
- ECG:
right ventricular hypertrophy
Hypoplastic left heart syndrome or single ventricle physiology states
History
most cases are diagnosed prenatally; more common in boys; if unrecognised at birth, infants become symptomatic at the time of the closure of the ductus arteriosus; when the ductus arteriosus closes, respiratory distress develops, shock and cyanosis with poor peripheral perfusion generally occur within the first 3 days of life; severe cyanosis can occur at birth when the foramen ovale is closed or restrictive
Exam
right ventricular heave and single S2 are present
1st investigation
- chest x-ray:
cardiomegaly with some degree of pulmonary congestion
- echocardiogram:
definitive diagnostic test that reveals abnormal cardiac anatomy and function
Other investigations
- ECG:
right ventricular hypertrophy
Tricuspid atresia
History
most cases are diagnosed antenatally by fetal echo; symptoms depend on the presence of ventricular septal defect (VSD); if there is a large shunt through the VSD, many infants may have mild cyanosis or none in the neonatal period; many infants present with congestive heart failure later; if the VSD is very restrictive, severe cyanosis may develop when the ductus arteriosus closes
Exam
systolic ejection murmur at the left upper sternal border and prominent left ventricular impulse
1st investigation
- chest x-ray:
depends on the degree of pulmonary blood flow and may present with pulmonary congestion
- echocardiogram:
definitive diagnostic test that reveals tricuspid atresia; enlarged right atrium and dilated right ventricle
Other investigations
- ECG:
left axis deviation and left ventricular hypertrophy
Truncus arteriosus
History
mild to moderate cyanosis with or without respiratory distress may present in first week of life; velocardiofacial syndrome (22q deletion) is present in 30% to 50% of truncus arteriosus cases
Exam
hyperdynamic precordium with loud single S2; loud systolic and diastolic murmur with wide pulse pressure and bounding pulses; respiratory distress depends on the degree of pulmonary congestion and worsens when pulmonary vascular resistance drops after the first 2 to 3 days; congestive heart failure may develop as a result
1st investigation
- chest x-ray:
cardiomegaly and increased pulmonary blood flow
- echocardiogram:
definitive diagnostic test; may reveal abnormal morphology and functional derangement of the truncal valve
Other investigations
- ECG:
biventricular hypertrophy
Pulmonary haemorrhage
History
most cases occurring in full-term infants will give a history of severe asphyxia or coagulopathy; in preterm infants who have haemodynamically significant patent ductus arteriosus (PDA) with left-to-right shunt, pulmonary haemorrhage may develop; most of these infants are ventilated post-surfactant instillation
Exam
sudden appearance of cyanosis or increased requirement of oxygen when infant is being ventilated is the earliest sign; bloody secretions from the trachea may be suctioned from the endotracheal tube; rales or diminished air entry found on the affected side, but condition is generally bilateral
1st investigation
- chest x-ray:
fluffy infiltrates bilaterally
- ABG:
severe hypoxia and hypercarbia
- FBC:
normal but in some cases thrombocytopenia may be present
- disseminated intravascular coagulation screen:
prolonged prothrombin time and PTT; low fibrinogen and low platelet count with increase in D-dimers
Other investigations
- echocardiogram:
to rule out significant PDA in preterm infants
Pulmonary hypoplasia
History
history of oligohydramnios and respiratory distress soon after birth are present; higher incidence of pneumothorax in these cases
Exam
tachypnoea, cyanosis, and fair to poor aeration of lungs present; S2 is loud with associated pulmonary hypertension
1st investigation
- chest x-ray:
decreased lung volume
- ABG:
hypoxia and hypercarbia
Other investigations
- echocardiogram:
pulmonary hypertension may be present
Congenital lobar emphysema
History
generally asymptomatic at birth; respiratory distress becomes progressively worse over the next few days
Exam
tachypnoea and cyanosis are present; diminished air entry over the affected side (commonly over left upper chest)
1st investigation
- chest x-ray:
hyperinflation of the affected lobe present; in severe cases, there may be herniation to the opposite side
- ABG:
hypoxia and hypercarbia
Other investigations
- chest CT:
demarcates the exact anatomical involvement of the lung
Pulmonary lymphangiectasia
History
respiratory distress and cyanosis in the newborn
Exam
tachypnoea and cyanosis in a full-term newborn; air entry will not be diminished; occasionally rales may be heard
1st investigation
- chest x-ray:
diffuse reticular opacities bilaterally
Other investigations
- CT scan of the chest:
suggestive of the extent of involvement of lymphangiectasia
- lung biopsy:
lymphatic dilation evident in 3 lymphatic sites; periarterial, subpleural, and interlobular septae
Tracheo-oesophageal fistula (TOF)/oesophageal atresia (OA)
History
history of polyhydramnios and large amount of pharyngeal secretions present after birth; inability to pass an orogastric or nasogastric tube is diagnostic; OA associated with VACTERL (vertebral anomalies, imperforate anus, cardiac lesions, TOF, renal and limb anomalies)
Exam
respiratory distress with frothy secretions at the mouth following birth is usually present; conducted upper airway sounds will be heard on auscultation; presentation at birth is typically the result of OA with/without tracheo-oesophageal fistula; respiratory distress is due to secretions in the upper airway and aspiration
1st investigation
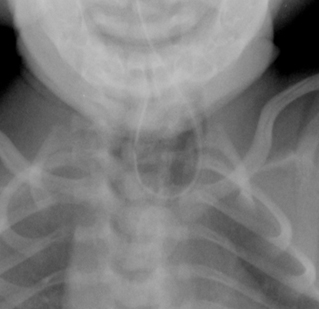
- chest x-ray:
diagnostic with an indwelling orogastric tube curled in the upper oesophageal pouch
More
Pleural effusion
History
most pleural effusions present at birth are seen in infants with hydrops fetalis and are diagnosed by antenatal ultrasound; in severe cases it will be difficult to ventilate unless needle aspiration or chest tube insertion occurs to remove the fluid; minor degrees of pleural effusion are seen in pneumonitis, meconium aspiration syndrome, and persistent pulmonary hypertension of newborn
Exam
in severe cases, diminished air entry will be present on the affected side; in bilateral effusions, as seen in hydrops fetalis, it will be difficult to ventilate the lungs unless the pleural fluid is evacuated
1st investigation
- chest x-ray:
opacity on the lateral border of the chest with blunting of the cardiophrenic angle in unilateral effusions; in severe cases, mediastinal shift to contralateral side if the effusion is unilateral; in severe bilateral pleural effusions, the whole chest is opaque with an indistinguishable cardiac border
More
Other investigations
- ultrasound of the chest:
characteristic for pleural effusion
Arteriovenous malformation
History
congestive heart failure, large head due to hydrocephalus, seizures
Exam
bruit may be heard over the cranium on auscultation
1st investigation
- chest x-ray:
may show cardiomegaly
Other investigations
- angiogram or MRA (magnetic resonance angiogram):
may reveal the vascular abnormality
Use of this content is subject to our disclaimer