Aetiology
Any of the following five mechanisms may give rise to arterial oxygen desaturation:
Hypoventilation
Ventilation-perfusion mismatching
Diffusion impairment
Significant right-to-left intracardiac or intrapulmonary shunting
Inadequate transport of oxygen by the haemoglobin.
During assessment, it is helpful to break down the aetiology into different systems. Cyanosis may be due to:
Cardiac causes (memorised as the 5-Ts mnemonic):
Transposition of great arteries: the great arteries (the aorta and the pulmonary artery) have their origins transposed so that the aorta originates from the right ventricle and the pulmonary artery originates from the left ventricle. Thus, deoxygenated blood is in the aorta, giving rise to severe cyanosis. Generally, these infants have an intra-cardiac shunt, such as a ventricular septal defect (VSD) or an atrial septal defect (ASD). The condition is a life-threatening emergency if there is no intra-cardiac shunt.
Tetralogy of Fallot: the four common components are right ventricular hypertrophy, infundibular pulmonary stenosis, overriding of the aorta, and a VSD. Most infants will be cyanotic at birth but a few of them will have adequate oxygen saturation depending on the pulmonary blood flow and shunt.
Total anomalous pulmonary venous return: the pulmonary veins drain into the right atrium (instead of the left atrium) and this condition leads to profound cyanosis and pulmonary congestion. The veins may also drain into the superior vena cava, inferior vena cava, or hepatic veins. The condition is generally associated with an ASD for intracardiac shunting. The condition can be partial or total, depending on whether all four pulmonary veins drain into the right side or not.
Truncus arteriosus: one large vessel originates from both ventricles, instead of two vessels (the aorta and the pulmonary artery). It is associated with a VSD. This gives rise to cyanosis and increased pulmonary blood flow.
Tricuspid atresia: right atrial blood is forced to shunt through foramen ovale or ASD to the left atrium; most patients also have a VSD. This condition is usually associated with a hypoplastic right ventricle.
Other less common cardiac causes:
Pulmonary atresia: generally associated with a VSD but may occur with intact ventricular septum, in which case pulmonary blood flow depends on the patent ductus arteriosus (PDA).
Ebstein's anomaly: the tricuspid valve is abnormal with two of its leaflets displaced towards the right ventricle with subsequent atrialisation of the right ventricle. The right atrium is significantly enlarged and there is regurgitation of the tricuspid valve; shunt takes place from right atrium through foramen ovale to left atrium.
Left-to-right shunt with pulmonary oedema: generally this takes place if there is a VSD or PDA. Cyanosis is less severe than in conditions where there is right-to-left shunt but they have more severe respiratory distress.
Single ventricle states (hypoplastic left or right heart).
Low cardiac output states.
Pulmonary causes:[4]
Parenchymal
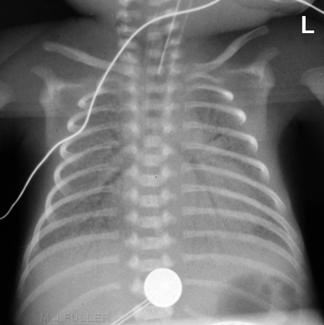
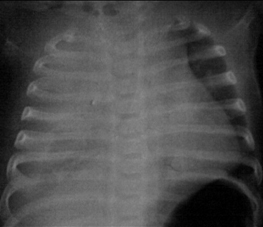
Respiratory distress syndrome due to surfactant deficiency in preterm infants and surfactant protein B deficiency or ABCA3 (adenosine triphosphate-binding cassette, sub-family A) mutations in full-term infants[Figure caption and citation for the preceding image starts]: Hyaline membrane disease (respiratory distress syndrome type 1): air bronchograms and a reticular granular patternFrom the collection of Ponthenkandath Sasidharan, MD; used with permission [Citation ends].
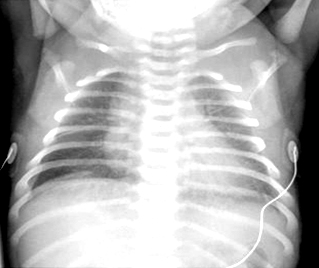
Transient tachypnoea of the newborn due to delayed clearance of fetal pulmonary fluid[Figure caption and citation for the preceding image starts]: Transient tachypnoea of the newborn (respiratory distress syndrome type 2): perihilar streakiness and horizontal fissural fluid on the rightFrom the collection of Ponthenkandath Sasidharan, MD; used with permission [Citation ends].
Aspiration (meconium, blood, or milk) can give rise to atelectasis or chemical pneumonitis[Figure caption and citation for the preceding image starts]: Meconium aspiration syndromeFrom the collection of Ponthenkandath Sasidharan, MD; used with permission [Citation ends].

Pneumonia
Pulmonary haemorrhage (seen in coagulopathy, asphyxia, or left-to-right shunts with pulmonary oedema)
Pulmonary oedema
Pulmonary hypoplasia (history of oligohydramnios, prolonged premature rupture of membranes, or congenital diaphragmatic hernia)[Figure caption and citation for the preceding image starts]: Congenital diaphragmatic herniaFrom the collection of Ponthenkandath Sasidharan, MD; used with permission [Citation ends].

Congenital lobar emphysema
Congenital pulmonary airway malformation (CPAM; formerly known as congenital cystic adenomatoid malformation [CCAM])[Figure caption and citation for the preceding image starts]: Congenital pulmonary airway malformation (CPAM; formerly known as congenital cystic adenomatoid malformation [CCAM])From the collection of Ponthenkandath Sasidharan, MD; used with permission [Citation ends].

Pulmonary lymphangiectasia: a rare congenital condition with pulmonary subpleural, interlobar, perivascular, and peribronchial lymphatic dilation, leading to significant respiratory distress at birth.
Non-parenchymal
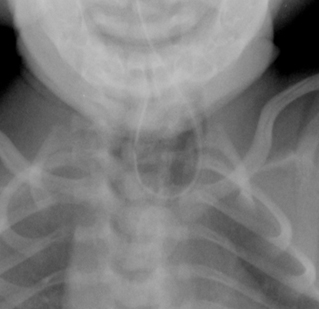
Tracheo-oesophageal fistula/oesophageal atresia[Figure caption and citation for the preceding image starts]: Tracheo-oesophageal fistula: orogastric tube curled in the oesophagusFrom the collection of Ponthenkandath Sasidharan, MD; used with permission [Citation ends].
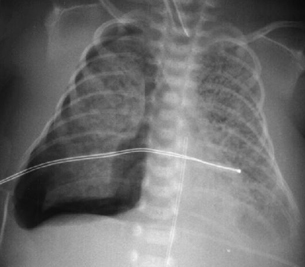
Pneumothorax[Figure caption and citation for the preceding image starts]: Pneumothorax (right side)From the collection of Ponthenkandath Sasidharan, MD; used with permission [Citation ends].
Pleural effusion[Figure caption and citation for the preceding image starts]: Pleural effusion (right side) with mediastinal shift to the leftFrom the collection of Ponthenkandath Sasidharan, MD; used with permission [Citation ends].
Upper airway obstruction (choanal atresia, laryngeal web, laryngomalacia, subglottic stenosis, and vocal cord paralysis)
Persistent pulmonary hypertension of the newborn.
Other important conditions to consider include:
Methaemoglobinaemia
Sepsis giving rise to apnoea; pulmonary haemorrhage may be seen in severe cases, in the presence of disseminated intravascular coagulation
Hypoglycaemia leading to apnoea or seizures
Polycythaemia, usually does not result in central cyanosis, but may give rise to increased pulmonary vascular resistance and delayed clearance of fetal pulmonary fluid; acrocyanosis is frequently seen
Asphyxia resulting in subsequent hypoventilation
Arteriovenous malformation leading to (high output) congestive heart failure.
Other disorders of haemoglobin (haemoglobin M and sulfhaemoglobinaemia) occur very rarely. Cyanosis can also result in any severely ill infant when a range of other features are present (e.g., metabolic acidosis, seizures).
Use of this content is subject to our disclaimer