Slipped capital femoral epiphysis
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
unstable SCFE
urgent surgical repair
The treatment of unstable SCFE is similar to that of stable SCFE. However, there are differences regarding timing of the surgery, decompression of hip joint, incidental reduction of the SCFE, and stabilisation method with 1 or 2 screws.[Figure caption and citation for the preceding image starts]: Unstable SCFE of the right hip fixed with 2 screws. Left hip prophylactic fixation with a single screw. Antero-posterior post-operative x-rayImage courtesy of John M. Flynn, MD [Citation ends]. [Figure caption and citation for the preceding image starts]: Unstable SCFE of the right hip fixed with 2 screws. Left hip prophylactic fixation with a single screw. Frog-leg lateral post-operative x-rayImage courtesy of John M. Flynn, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Unstable SCFE of the right hip fixed with 2 screws. Left hip prophylactic fixation with a single screw. Frog-leg lateral post-operative x-rayImage courtesy of John M. Flynn, MD [Citation ends].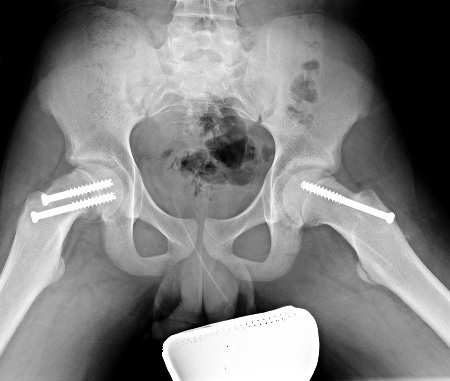 An accepted approach is to operate acutely, with percutaneous decompression of the hip joint, incidental repositioning of the slip, and fixation with 2 screws. Early manipulative reduction of SCFE is recommended.
An accepted approach is to operate acutely, with percutaneous decompression of the hip joint, incidental repositioning of the slip, and fixation with 2 screws. Early manipulative reduction of SCFE is recommended.
Open reduction and internal fixation with the modified Dunn procedure, in addition to surgical hip dislocation, allows restoration of proximal femoral anatomy and may decrease the risk of avascular necrosis (AVN) in unstable SCFE. This procedure is associated with low complication rates in the hands of surgeons experienced with the technique.[29]Ziebarth K, Zilkens C, Spencer S, et al. Capital realignment for moderate and severe SCFE using a modified Dunn procedure. Clin Orthop Relat Res. 2009 Mar;467(3):704-16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2635450 http://www.ncbi.nlm.nih.gov/pubmed/19142692?tool=bestpractice.com [30]Slongo T, Kakaty D, Krause F, et al. Treatment of slipped capital femoral epiphysis with a modified Dunn procedure. J Bone Joint Surg Am. 2010 Dec 15;92(18):2898-908. http://www.ncbi.nlm.nih.gov/pubmed/21159990?tool=bestpractice.com [31]Davis RL 2nd, Samora WP 3rd, Persinger F, et al. Treatment of Unstable Versus Stable Slipped Capital Femoral Epiphysis Using the Modified Dunn Procedure. J Pediatr Orthop. 2019 Sep;39(8):411-415. https://www.doi.org/10.1097/BPO.0000000000000975 http://www.ncbi.nlm.nih.gov/pubmed/31393301?tool=bestpractice.com Further long-term studies are needed to determine if it will be a better treatment long term gentle repositioning with decompression and screw fixation.
Meta-analysis of 4 studies comparing outcomes in reduced or unreduced unstable slipped capital femoral epiphysis found no statistically significant difference in risk of AVN between treatment groups.[33]Lowndes S, Khanna A, Emery D, et al. Management of unstable slipped upper femoral epiphysis: a meta-analysis. Br Med Bull. 2009;90:133-46. http://www.ncbi.nlm.nih.gov/pubmed/19376800?tool=bestpractice.com Meta-analysis of five studies that assessed timing of management found that treatment within 24 hours from the onset of instability was associated with a lower risk of AVN than treatment beyond that time.[33]Lowndes S, Khanna A, Emery D, et al. Management of unstable slipped upper femoral epiphysis: a meta-analysis. Br Med Bull. 2009;90:133-46. http://www.ncbi.nlm.nih.gov/pubmed/19376800?tool=bestpractice.com
prophylactic fixation of contralateral hip
Additional treatment recommended for SOME patients in selected patient group
Many surgeons have a low threshold for prophylactic fixation of contralateral hip in pathological SCFE (underlying metabolic disorder or endocrinopathy). There is no consensus on prophylactic fixation of contralateral hip in idiopathic SCFE.
Many variables have been investigated to predict subsequent SCFE in unilateral idiopathic SCFE. These include: sex, symptom duration, obesity, trauma, severity of index slip, laterality, patient age, modified Oxford bone score, and bone age.[36]Swarup I, Goodbody C, Goto R, et al. Risk Factors for Contralateral Slipped Capital Femoral Epiphysis: A Meta-analysis of Cohort and Case-control Studies. J Pediatr Orthop. 2020 Jul;40(6):e446-e453. https://www.doi.org/10.1097/BPO.0000000000001482 http://www.ncbi.nlm.nih.gov/pubmed/32501913?tool=bestpractice.com
The posterior sloping angle (PSA), defined as the angle between the line along the plane of the physis and the line perpendicular to the femoral neck-diaphyseal axis on axial radiograph, has been shown to be predictive of a contralateral slip in patients presenting with unilateral SCFE.[37]Park S, Hsu JE, Rendon N, et al. The utility of posterior sloping angle in predicting contralateral slipped capital femoral epiphysis. J Pediatr Orthop. 2010 Oct-Nov;30(7):683-9. http://www.ncbi.nlm.nih.gov/pubmed/20864853?tool=bestpractice.com In one study, PSA was more predictive in girls; the authors recommended prophylactic pinning with a PSA >13.[37]Park S, Hsu JE, Rendon N, et al. The utility of posterior sloping angle in predicting contralateral slipped capital femoral epiphysis. J Pediatr Orthop. 2010 Oct-Nov;30(7):683-9. http://www.ncbi.nlm.nih.gov/pubmed/20864853?tool=bestpractice.com According to one meta-analysis, younger patients with a high PSA of the unaffected hip are those most likely to benefit from prophylactic fixation.[36]Swarup I, Goodbody C, Goto R, et al. Risk Factors for Contralateral Slipped Capital Femoral Epiphysis: A Meta-analysis of Cohort and Case-control Studies. J Pediatr Orthop. 2020 Jul;40(6):e446-e453. https://www.doi.org/10.1097/BPO.0000000000001482 http://www.ncbi.nlm.nih.gov/pubmed/32501913?tool=bestpractice.com
Prophylactic pinning is likely to be beneficial for the long-term outcome of SCFE in some cases where underlying metabolic disorders are present. However, clinicians should consider each case on its own merits before offering prophylactic intervention.
stable SCFE
in situ screw fixation
The recommended treatment of stable SCFE is in situ fixation of the epiphysis with a single screw. However, other treatments including bone graft epiphysiodesis, spica cast, or in situ fixation with multiple pins have been described.
In situ single-screw fixation is the widely accepted first-line treatment for SCFE. The screw is placed in the centre of the epiphysis both on the antero-posterior and lateral aspects.[Figure caption and citation for the preceding image starts]: Unstable SCFE of the right hip fixed with 2 screws. Left hip prophylactic fixation with a single screw. Antero-posterior post-operative x-rayImage courtesy of John M. Flynn, MD [Citation ends]. [Figure caption and citation for the preceding image starts]: Unstable SCFE of the right hip fixed with 2 screws. Left hip prophylactic fixation with a single screw. Frog-leg lateral post-operative x-rayImage courtesy of John M. Flynn, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Unstable SCFE of the right hip fixed with 2 screws. Left hip prophylactic fixation with a single screw. Frog-leg lateral post-operative x-rayImage courtesy of John M. Flynn, MD [Citation ends].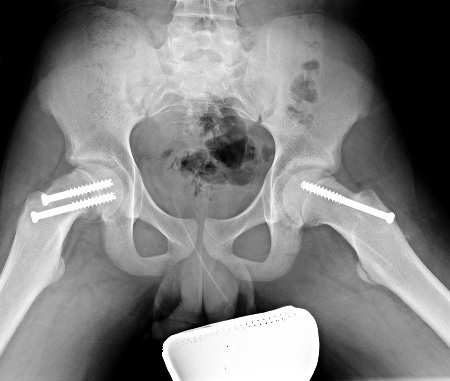 Advantages of in situ single-screw fixation include easy technique, low further slip rate, and prevention of complications.[26]Aronsson DD, Loder RT, Breur GJ, et al. Slipped capital femoral epiphysis: current concepts. J Am Acad Orthop Surg. 2006 Nov;14(12):666-79.
http://www.ncbi.nlm.nih.gov/pubmed/17077339?tool=bestpractice.com
Post-operatively, toe-touch weight bearing is permitted for the first 2 weeks followed by weight bearing as tolerated.
Advantages of in situ single-screw fixation include easy technique, low further slip rate, and prevention of complications.[26]Aronsson DD, Loder RT, Breur GJ, et al. Slipped capital femoral epiphysis: current concepts. J Am Acad Orthop Surg. 2006 Nov;14(12):666-79.
http://www.ncbi.nlm.nih.gov/pubmed/17077339?tool=bestpractice.com
Post-operatively, toe-touch weight bearing is permitted for the first 2 weeks followed by weight bearing as tolerated.
prophylactic fixation of contralateral hip
Additional treatment recommended for SOME patients in selected patient group
Many surgeons have a low threshold for prophylactic fixation of contralateral hip in pathological SCFE (underlying metabolic disorder or endocrinopathy). There is no consensus on prophylactic fixation of contralateral hip in idiopathic SCFE.
Many variables have been investigated to predict subsequent SCFE in unilateral idiopathic SCFE. These include: sex, symptom duration, obesity, trauma, severity of index slip, laterality, patient age, modified Oxford bone score, and bone age.[36]Swarup I, Goodbody C, Goto R, et al. Risk Factors for Contralateral Slipped Capital Femoral Epiphysis: A Meta-analysis of Cohort and Case-control Studies. J Pediatr Orthop. 2020 Jul;40(6):e446-e453. https://www.doi.org/10.1097/BPO.0000000000001482 http://www.ncbi.nlm.nih.gov/pubmed/32501913?tool=bestpractice.com
The posterior sloping angle (PSA), defined as the angle between the line along the plane of the physis and the line perpendicular to the femoral neck-diaphyseal axis on axial radiograph, has been shown to be predictive of a contralateral slip in patients presenting with unilateral SCFE.[37]Park S, Hsu JE, Rendon N, et al. The utility of posterior sloping angle in predicting contralateral slipped capital femoral epiphysis. J Pediatr Orthop. 2010 Oct-Nov;30(7):683-9. http://www.ncbi.nlm.nih.gov/pubmed/20864853?tool=bestpractice.com In one study, PSA was more predictive in girls; the authors recommended prophylactic pinning with a PSA >13.[37]Park S, Hsu JE, Rendon N, et al. The utility of posterior sloping angle in predicting contralateral slipped capital femoral epiphysis. J Pediatr Orthop. 2010 Oct-Nov;30(7):683-9. http://www.ncbi.nlm.nih.gov/pubmed/20864853?tool=bestpractice.com According to one meta-analysis, younger patients with a high PSA of the unaffected hip are those most likely to benefit from prophylactic fixation.[36]Swarup I, Goodbody C, Goto R, et al. Risk Factors for Contralateral Slipped Capital Femoral Epiphysis: A Meta-analysis of Cohort and Case-control Studies. J Pediatr Orthop. 2020 Jul;40(6):e446-e453. https://www.doi.org/10.1097/BPO.0000000000001482 http://www.ncbi.nlm.nih.gov/pubmed/32501913?tool=bestpractice.com
Prophylactic pinning is likely to be beneficial for the long-term outcome of SCFE in some cases where underlying metabolic disorders are present. However, clinicians should consider each case on its own merits before offering prophylactic intervention.
open reduction + internal fixation with surgical hip dislocation
Open reduction and internal fixation with the modified Dunn procedure in addition to surgical hip dislocation allows restoration of proximal femoral anatomy and may decrease the risk of AVN in unstable SCFE. Even in the clinically stable SCFE, the physis is often mobile, suggesting that the capital reduction procedure can be used.[29]Ziebarth K, Zilkens C, Spencer S, et al. Capital realignment for moderate and severe SCFE using a modified Dunn procedure. Clin Orthop Relat Res. 2009 Mar;467(3):704-16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2635450 http://www.ncbi.nlm.nih.gov/pubmed/19142692?tool=bestpractice.com
This procedure is associated with low complication rates in the hands of surgeons experienced with it.[29]Ziebarth K, Zilkens C, Spencer S, et al. Capital realignment for moderate and severe SCFE using a modified Dunn procedure. Clin Orthop Relat Res. 2009 Mar;467(3):704-16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2635450 http://www.ncbi.nlm.nih.gov/pubmed/19142692?tool=bestpractice.com [30]Slongo T, Kakaty D, Krause F, et al. Treatment of slipped capital femoral epiphysis with a modified Dunn procedure. J Bone Joint Surg Am. 2010 Dec 15;92(18):2898-908. http://www.ncbi.nlm.nih.gov/pubmed/21159990?tool=bestpractice.com However, the technique is technically demanding and, in one study, the avascular necrosis rate following treatment with the modified Dunn procedure was much higher in stable SCFEs (29%) than unstable SCFEs (6%).[31]Davis RL 2nd, Samora WP 3rd, Persinger F, et al. Treatment of Unstable Versus Stable Slipped Capital Femoral Epiphysis Using the Modified Dunn Procedure. J Pediatr Orthop. 2019 Sep;39(8):411-415. https://www.doi.org/10.1097/BPO.0000000000000975 http://www.ncbi.nlm.nih.gov/pubmed/31393301?tool=bestpractice.com
Further long-term studies are needed to determine if it will be a better treatment long term than in-situ fixation.
prophylactic fixation of contralateral hip
Additional treatment recommended for SOME patients in selected patient group
Many surgeons have a low threshold for prophylactic fixation of contralateral hip in pathological SCFE (underlying metabolic disorder or endocrinopathy). There is no consensus on prophylactic fixation of contralateral hip in idiopathic SCFE.
Many variables have been investigated to predict subsequent SCFE in unilateral idiopathic SCFE. These include: sex, symptom duration, obesity, trauma, severity of index slip, laterality, patient age, modified Oxford bone score, and bone age.[36]Swarup I, Goodbody C, Goto R, et al. Risk Factors for Contralateral Slipped Capital Femoral Epiphysis: A Meta-analysis of Cohort and Case-control Studies. J Pediatr Orthop. 2020 Jul;40(6):e446-e453. https://www.doi.org/10.1097/BPO.0000000000001482 http://www.ncbi.nlm.nih.gov/pubmed/32501913?tool=bestpractice.com
The posterior sloping angle (PSA), defined as the angle between the line along the plane of the physis and the line perpendicular to the femoral neck-diaphyseal axis on axial radiograph, has been shown to be predictive of a contralateral slip in patients presenting with unilateral SCFE.[37]Park S, Hsu JE, Rendon N, et al. The utility of posterior sloping angle in predicting contralateral slipped capital femoral epiphysis. J Pediatr Orthop. 2010 Oct-Nov;30(7):683-9. http://www.ncbi.nlm.nih.gov/pubmed/20864853?tool=bestpractice.com In one study, PSA was more predictive in girls; the authors recommended prophylactic pinning with a PSA >13.[37]Park S, Hsu JE, Rendon N, et al. The utility of posterior sloping angle in predicting contralateral slipped capital femoral epiphysis. J Pediatr Orthop. 2010 Oct-Nov;30(7):683-9. http://www.ncbi.nlm.nih.gov/pubmed/20864853?tool=bestpractice.com According to one meta-analysis, younger patients with a high PSA of the unaffected hip are those most likely to benefit from prophylactic fixation.[36]Swarup I, Goodbody C, Goto R, et al. Risk Factors for Contralateral Slipped Capital Femoral Epiphysis: A Meta-analysis of Cohort and Case-control Studies. J Pediatr Orthop. 2020 Jul;40(6):e446-e453. https://www.doi.org/10.1097/BPO.0000000000001482 http://www.ncbi.nlm.nih.gov/pubmed/32501913?tool=bestpractice.com
Prophylactic pinning is likely to be beneficial for the long-term outcome of SCFE in some cases where underlying metabolic disorders are present. However, clinicians should consider each case on its own merits before offering prophylactic intervention.
bone graft epiphysiodesis
Bone graft epiphysiodesis involves removing a portion of residual physis with drill and curettage, through a rectangular window on the anterior aspect of the neck. A cylindrical tract is created which is filled with autologous graft obtained from the iliac crest. The disadvantages of this technique are a wider extensive exposure, blood loss, longer hospital stay, and the potential for further slippage until the physis is closed.
prophylactic fixation of contralateral hip
Additional treatment recommended for SOME patients in selected patient group
Many surgeons have a low threshold for prophylactic fixation of contralateral hip in pathological SCFE (underlying metabolic disorder or endocrinopathy). There is no consensus on prophylactic fixation of contralateral hip in idiopathic SCFE.
Many variables have been investigated to predict subsequent SCFE in unilateral idiopathic SCFE. These include: sex, symptom duration, obesity, trauma, severity of index slip, laterality, patient age, modified Oxford bone score, and bone age.[36]Swarup I, Goodbody C, Goto R, et al. Risk Factors for Contralateral Slipped Capital Femoral Epiphysis: A Meta-analysis of Cohort and Case-control Studies. J Pediatr Orthop. 2020 Jul;40(6):e446-e453. https://www.doi.org/10.1097/BPO.0000000000001482 http://www.ncbi.nlm.nih.gov/pubmed/32501913?tool=bestpractice.com
The posterior sloping angle (PSA), defined as the angle between the line along the plane of the physis and the line perpendicular to the femoral neck-diaphyseal axis on axial radiograph, has been shown to be predictive of a contralateral slip in patients presenting with unilateral SCFE.[37]Park S, Hsu JE, Rendon N, et al. The utility of posterior sloping angle in predicting contralateral slipped capital femoral epiphysis. J Pediatr Orthop. 2010 Oct-Nov;30(7):683-9. http://www.ncbi.nlm.nih.gov/pubmed/20864853?tool=bestpractice.com In one study, PSA was more predictive in girls; the authors recommended prophylactic pinning with a PSA >13.[37]Park S, Hsu JE, Rendon N, et al. The utility of posterior sloping angle in predicting contralateral slipped capital femoral epiphysis. J Pediatr Orthop. 2010 Oct-Nov;30(7):683-9. http://www.ncbi.nlm.nih.gov/pubmed/20864853?tool=bestpractice.com According to one meta-analysis, younger patients with a high PSA of the unaffected hip are those most likely to benefit from prophylactic fixation.[36]Swarup I, Goodbody C, Goto R, et al. Risk Factors for Contralateral Slipped Capital Femoral Epiphysis: A Meta-analysis of Cohort and Case-control Studies. J Pediatr Orthop. 2020 Jul;40(6):e446-e453. https://www.doi.org/10.1097/BPO.0000000000001482 http://www.ncbi.nlm.nih.gov/pubmed/32501913?tool=bestpractice.com
Prophylactic pinning is likely to be beneficial for the long-term outcome of SCFE in some cases where underlying metabolic disorders are present. However, clinicians should consider each case on its own merits before offering prophylactic intervention.
late deformity
corrective surgery
The retroverted deformity of femoral head remodels over a period of time. However, disabling external rotation deformity persists in some patients, causing gait disturbance and femoro-acetabular impingement. This in turn leads to pain and restricted range of motion at hip.
This can be corrected by creating a secondary deformity counteracting the principal deformity through osteotomy. In SCFE the deformity is in the physis and osteotomy closer to the apex of deformity is preferable. Both femoral neck and inter-trochanteric osteotomies have been performed. Cuneiform osteotomy through the femoral neck achieves better correction but is technically demanding and associated with increased risk of osteonecrosis.[34]Gage JR, Sundberg AB, Nolan DR, et al. Complications after cuneiform osteotomy for moderately or severely slipped capital femoral epiphysis. J Bone Joint Surg Am. 1978 Mar;60(2):157-65. http://www.ncbi.nlm.nih.gov/pubmed/641077?tool=bestpractice.com [35]Hall JE. The results of treatment of slipped femoral epiphysis. J Bone Joint Surg Br. 1957 Nov;39-B(4):659-73. http://www.ncbi.nlm.nih.gov/pubmed/13491628?tool=bestpractice.com
Inter-trochanteric osteotomies such as Southwick's or Imhauser's are surgically less demanding than cuneiform osteotomy and the incidence of osteonecrosis is less. In Imhauser's osteotomy an anterior-based wedge is removed from the inter-trochanteric region and the distal fragment is flexed and internally rotated. This is fixed with either an angled blade plate or a plate-and-screw system.

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer