Approach
SCFE should be treated surgically as soon as it is recognised. The patient should be advised not to bear weight on the affected hip and should be immediately referred to an orthopaedic surgeon. Early surgical intervention can prevent slip progression and complications such as osteonecrosis.
The aim of treatment in SCFE is to prevent progression of slip. This can be achieved with in situ fixation of the epiphysis. Prophylactic fixation of the contralateral hip may be necessary and should be considered on a case-by-case basis. Late deformity of the hip is a chronic and disabling complication that may require intervention.
Stable slipped capital femoral epiphysis
The mainstay treatment of stable slip is in situ fixation of the epiphysis with a single screw. However, other treatments including bone graft epiphysiodesis, spica cast, or in situ fixation with multiple pins have been described.
In situ single-screw fixation is the widely accepted first-line treatment for SCFE. A screw is placed in the centre of the epiphysis on both the antero-posterior and the lateral view.[Figure caption and citation for the preceding image starts]: Unstable SCFE of the right hip fixed with 2 screws. Left hip prophylactic fixation with a single screw. Antero-posterior post-operative x-rayImage courtesy of John M. Flynn, MD [Citation ends]. [Figure caption and citation for the preceding image starts]: Unstable SCFE of the right hip fixed with 2 screws. Left hip prophylactic fixation with a single screw. Frog-leg lateral post-operative x-rayImage courtesy of John M. Flynn, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Unstable SCFE of the right hip fixed with 2 screws. Left hip prophylactic fixation with a single screw. Frog-leg lateral post-operative x-rayImage courtesy of John M. Flynn, MD [Citation ends].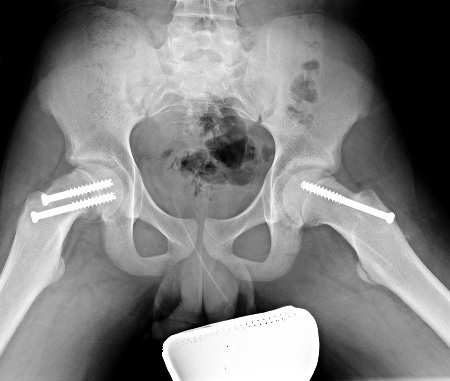 The benefits of in situ single-screw fixation include easy technique, low subsequent slip rate, and few complications.[26] Post-operatively, toe-touch weight bearing is permitted for the first 2 weeks followed by weight bearing as tolerated.
The benefits of in situ single-screw fixation include easy technique, low subsequent slip rate, and few complications.[26] Post-operatively, toe-touch weight bearing is permitted for the first 2 weeks followed by weight bearing as tolerated.
Surgical dislocation of adult hip without the risk of avascular necrosis has created interest in open treatment of SCFE to anatomically realign the slip.[27] This treatment is proposed for unstable as well as for stable SCFE.[28] In late deformity the retroverted proximal femur causes femoro-acetabular impingement. This treatment should be restricted to select specialised centres until long-term results and outcome are available. In small patient series, treatment with a modified capital reorientation (Dunn) procedure, that included surgical hip dislocation in both stable and unstable SCFE, was associated with good results, and low complication rates, in the hands of surgeons experienced with the technique.[29][30] The open reduction allows for the restoration of a more normal proximal femoral anatomy with complete correction of the slip angle and head-neck offset. However, the technique is technically demanding and, in one study, the avascular necrosis rate following treatment with the modified Dunn procedure was much higher in stable SCFEs (29%) than unstable SCFEs (6%).[31]
Bone graft epiphysiodesis involves removing a portion of residual physis with drill and curettage, through a rectangular window on the anterior aspect of the femoral neck. A cylindrical tract is created, which is filled with autologous graft obtained from the iliac crest. The disadvantages of this technique are:
A wider extensive exposure
Blood loss
Longer hospital stay
Risk of further slippage until the physis is closed.
Hip spica cast immobilisation is an antiquated technique. It involved immobilising both hips in a hip spica. Chondrolysis and further slip are the most common complications.[32]
Unstable slipped capital femoral epiphysis
The treatment of unstable SCFE is similar to that of stable SCFE. Differences include:
Timing of the surgery
Decompression of hip joint
Reduction of the SCFE
Stabilisation with 1 or 2 screws.
One accepted approach is to treat the condition acutely with percutaneous decompression of the hip joint, incidental repositioning of the slip, and fixation with 2 screws.
Open reduction and internal fixation with the modified Dunn procedure in addition to surgical hip dislocation allows restoration of proximal femoral anatomy and may decrease the risk of avascular necrosis (AVN) in unstable SCFE. This procedure is associated with low complication rates in the hands of surgeons experienced with the technique.[29][30][31] Further long-term studies are needed to determine if it will be a better treatment long term than gentle repositioning with joint decompression and screw fixation.
Meta-analysis of 4 studies comparing outcomes in reduced or unreduced unstable slipped capital femoral epiphysis found no statistically significant difference in risk of avascular necrosis between treatment groups.[33] Meta-analysis of five studies that assessed timing of management found that treatment within 24 hours from the onset of instability was associated with a lower risk of AVN than treatment beyond that time.[33] The retrospective studies included in these meta-analyses were deemed to be susceptible to bias.[33]
It should be emphasised that unstable SCFEs should be treated within 24 hours, as manipulation after this time is associated with a higher rate of AVN.
Late deformity and corrective surgery
The retroverted deformity of the femoral head remodels over a period of time. However, disabling external rotation deformity persists in a few patients, causing gait disturbance and femoro-acetabular impingement. This leads to pain and restricted range of motion at the hip.
This can be corrected by creating a secondary deformity counteracting the principal deformity through osteotomy. In SCFE the deformity is in the physis and osteotomy close to the apex of deformity is preferable. Both femoral neck and inter-trochanteric osteotomies have been performed. Cuneiform osteotomy performed through the femoral neck achieves better results but is technically demanding and associated with increased risk of osteonecrosis.[34][35]
Inter-trochanteric osteotomies such as Southwick's or Imhauser's are surgically less demanding than cuneiform osteotomy, and the incidence of osteonecrosis is less. In Imhauser's osteotomy an anterior-based wedge is removed from inter-trochanteric region and the distal fragment is flexed and internally rotated. This is fixed with either an angled blade plate or a plate-and-screw system.
Prophylactic fixation of contralateral hip
Many surgeons have a low threshold for prophylactic fixation of contralateral hip in pathological SCFE (underlying metabolic disorder or endocrinopathy). Despite this, there is no consensus on prophylactic fixation of contralateral hip in idiopathic SCFE.
Many variables have been investigated to predict subsequent SCFE in unilateral idiopathic SCFE.
These include:[36]
Sex of patient
Symptom duration
Obesity
Trauma
Severity of index slip
Laterality
Patient age
Modified Oxford bone score
Bone age.
The posterior sloping angle (PSA), defined as the angle between the line along the plane of the physis and the line perpendicular to the femoral neck-diaphyseal axis on axial radiograph, has been shown to be predictive of a contralateral slip in patients presenting with unilateral SCFE.[37] In one study, PSA was more predictive in girls; the authors recommended prophylactic pinning with a PSA >13.[37] According to one meta-analysis, younger patients with a high PSA of the unaffected hip are those most likely to benefit from prophylactic fixation.[36]
Prophylactic pinning is likely to be beneficial for the long-term outcome of contralateral SCFE in some cases where underlying metabolic disorders are present. However, clinicians should consider each case on its own merits before offering prophylactic intervention.
Use of this content is subject to our disclaimer