Approach
Accurate diagnosis of Legg-Calvé-Perthes' (Perthes') disease involves a detailed history for risk factors and onset of symptoms, examination of the hip and gait, and radiographic evaluation. Laboratory investigations are rarely indicated unless the patient has an acute exacerbation.
History
The patient usually presents with a painless limp and normal activities. If pain is present, it may have a varied radiation based on the different nerves that innervate the hip joint; it may radiate to the suprapatellar portion of the knee through the femoral nerve, the medial aspect of the thigh via the obturator nerve, or the buttocks via the sciatic nerve. This may occasionally lead to a delay in diagnosis. There may be an associated history of trauma at presentation. Perthes' disease is a non-traumatic condition, although a history of minor trauma may be noted. Some studies have reported synovitis to be the first symptom although this has not been proven, and the association may be incidental.[30][31]
Perthes' disease typically affects 4- to 8-year-old children, although the age range at onset can be from 2 to 12 years and can also rarely affect adolescents. It is 4 to 5 times more common in males than females. When girls are affected, involvement of the femoral head is more severe compared with that in boys of the same age. The higher the age at onset, the more severe the involvement as there is less re-modelling potential, a higher extent of incongruity at the end of the natural history, and a worse prognosis. Females also tend to have a more severe involvement than males at a later age.
There is often a history of short stature as compared to peers and hence previous assessment of growth is important. However, children with Perthes' attain puberty and a normal final height by the mid teens. A history suggestive of any other endocrinopathy should also be sought.
A history of passive smoking in the environment, or of maternal smoking during pregnancy or early childhood, should be obtained. The social history should also be obtained as there is a link between Perthes' disease and a low socio-economic status. Family history may indicate presence of skeletal dysplasias or a thrombotic disease.
The patient should also be assessed for the presence of an ADHD. Children with this disease tend to be hyperactive and indulge in several sporting activities unless symptomatic. Overall, they are in good health.
Physical examination
Examination reveals a stature that is shorter than that of peers. The gait is a painless limp that can be described as a gluteus medius lurch, though may be antalgic during acutely painful episodes.
Quadriceps and gluteal muscle wasting are common and the Trendelenburg's test is positive. The Trendelenburg test is performed by asking the patient to stand on one leg for 30 seconds without leaning to any side. A normal test is defined if the pelvis stays level, or rises, during the one-leg stance. A positive Trendelenburg Test is defined if the pelvis drops toward the unsupported side during unilateral weight bearing.
An associated adduction contracture at the hip may account for an apparent limb length shortening. Range of motion at the hip joint in the acute phase is limited due to muscle spasm. With progression of the disease, internal rotation and abduction in extension are limited owing to head shape. The later stage of the disease may be characterised by a global reduction in all ranges of motion with associated pain, indicative of joint arthritis.
Radiographic evaluation
These are the mainstay of diagnosis and follow-up of the disease process through its several stages:
Stage 1, ischaemia: may initially appear normal but careful comparison with the opposite side may show a pseudosubluxation or subtle widening of the joint space (Waldenstrom's sign), which is due to relative cartilage overgrowth, especially in the later phases of this stage.
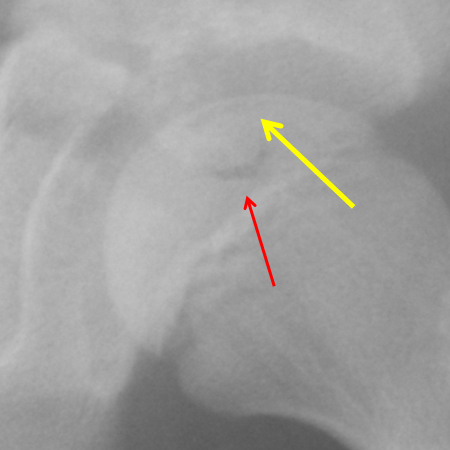
Stage 2; resorption, fragmentation, re-vascularisation, and repair: a subchondral fracture, if seen, may be the first finding of the disease. However, a subchondral fracture is difficult to visualise, requires very good quality radiograph images, and is only seen in 50% of cases. This is known as Salter's, Caffrey's, or the crescent sign. Resorption of the ischaemic bone appears as fragmentation of the affected area of the proximal femoral head on plain x-rays. Metaphyseal cysts and osteolysis of the superolateral portion of the femoral head (Gage's sign) are noted during the early phases of this stage. Resorption of the dead trabeculae and replacement with reparative tissue takes place over a period of 12 to 18 months. During this stage the softened femoral head progressively gets deformed by the joint forces. The true extent of the ischaemia of the femoral head is evident at the conclusion of this phase.[Figure caption and citation for the preceding image starts]: X-ray of stage 2 showing a subchondral fracture line (yellow arrow) and fragmentation (red arrow)From the personal collection of Dominique Knight [Citation ends].
Stage 3; re-ossification and resolution: this starts at the epiphyseal margins (paraphyseal ossification). The femoral head is ossified in its deformed shape. Bone bridges across the growth plate lead to growth arrests.[Figure caption and citation for the preceding image starts]: X-ray of stage 3 showing re-ossificationFrom the personal collection of Dominique Knight [Citation ends].

Stage 4; re-modelling: the age of the child at the onset of presentation is vital because the re-modelling potential reduces with age. Re-modelling changes in the acetabulum can lead to a congruent lining with the aspherical head. However, the potential for re-modelling is progressively lost in the older child and the aspheric femoral head remains incongruous with the acetabulum. This can lead to severe osteoarthritis at a young age. Congruence is a more important predictor of future osteoarthritis compared with femoral head sphericity.
Laboratory studies
Laboratory investigations are only indicated in the presence of pain, any acute symptoms, or to help exclude other diagnoses. FBC is typically normal. Erythrocyte sedimentation rate and other inflammatory markers such as C-reactive protein may be reactively increased in the symptomatic phase of the disease or may indicate an alternative pathology.
Other investigations
Scintigraphy bone scans may be used in Stage 1 (ischaemia), when radiographs may appear normal. This will detect a "cold spot" in the affected hip early in the disease process.
MRI is also a useful adjunct in the early stages of diagnosis. This investigation is a sensitive modality in diagnosing Perthes' disease.[58] If performed 6 months after disease onset, an MRI can accurately demonstrate the degree of epiphyseal involvement.[59] A low MR perfusion index has demonstrated to be a potential early predictor of greater deformity at 2 years.[60] Furthermore, a preliminary study using early perfusion MRI has shown it to be predictive of eventual lateral pillar involvement.[61] After re-ossification, MRI of the hips may also be useful in assessing the extent of the damage in one or both hips.[Figure caption and citation for the preceding image starts]: MRI scans of the same patient taken 8 years apart showing Perthes' disease of the left femoral epiphysis and proportional increase in cartilage thickness compared to the right side. Later scan (image on right) starting to show uptakeFrom the personal collection of Dominique Knight [Citation ends].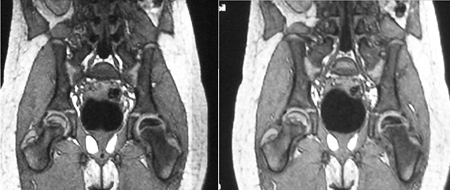 [Figure caption and citation for the preceding image starts]: MRI showing partial collapse of the left femoral head with areas of necrosisFrom BMJ Case Reports http://casereports.bmj.com/cgi/content/full/2009/jan08_1/bcr2007132811Copyright © 2011 by BMJ Publishing Group Ltd [Citation ends].
[Figure caption and citation for the preceding image starts]: MRI showing partial collapse of the left femoral head with areas of necrosisFrom BMJ Case Reports http://casereports.bmj.com/cgi/content/full/2009/jan08_1/bcr2007132811Copyright © 2011 by BMJ Publishing Group Ltd [Citation ends].
Use of this content is subject to our disclaimer