Treatment of brachial plexus birth injury (BPBI) has been evolving and remains controversial. Different centres recommend different treatments for different reasons, but the overall goal is to maximise the use and function of the affected extremity.
Newborns (<4 weeks) or infants (from 4 weeks to 1 year): initial treatment
Supportive care
After ruling out other causes of pseudoparalysis of the upper extremity, the arm is protected by careful handling of the infant.[46]Shenaq SM, Bullocks JM, Dhillon G, et al. Management of infant brachial plexus injuries. Clin Plast Surg. 2005 Jan;32(1):79-98, ix.
http://www.ncbi.nlm.nih.gov/pubmed/15636767?tool=bestpractice.com
[47]Waters PM. Update on management of pediatric brachial plexus palsy. J Pediatr Orthop B. 2005 Jul;14(4):233-44.
http://www.ncbi.nlm.nih.gov/pubmed/15931025?tool=bestpractice.com
[48]Clarke HM, Curtis CG. An approach to obstetrical brachial plexus injuries. Hand Clin. 1995 Nov;11(4):563-80.
http://www.ncbi.nlm.nih.gov/pubmed/8567739?tool=bestpractice.com
[49]Zafeiriou DI, Psychogiou K. Obstetrical brachial plexus palsy. Pediatr Neurol. 2008 Apr;38(4):235-42.
http://www.ncbi.nlm.nih.gov/pubmed/18358400?tool=bestpractice.com
[86]Vuillermin C, Bauer AS. Boston Children's Hospital approach to brachial plexus birth palsy. J Pediatr Orthop B. 2016 Jul;25(4):296-304.
http://www.ncbi.nlm.nih.gov/pubmed/27137763?tool=bestpractice.com
The likelihood of potential re-injury during initial inflammatory response to the injury remains unclear.[47]Waters PM. Update on management of pediatric brachial plexus palsy. J Pediatr Orthop B. 2005 Jul;14(4):233-44.
http://www.ncbi.nlm.nih.gov/pubmed/15931025?tool=bestpractice.com
Instruct parents to avoid lifting the child under the arms and to lift him or her by supporting under the head and shoulders with one hand and under the buttocks with the other. When changing clothes, the affected arm should be placed into the sleeve first, followed by the head and the unaffected arm last. This avoids extremes of motion. When removing the clothes, the affected arm should be removed last. Normal bathing and infant care are otherwise instituted for the first 2 weeks.
In the past, safety-pinning the sleeve of the affected arm to the chest area was recommended, but this is no longer considered essential.
Physiotherapy or occupational therapy
Home stretches are typically initiated when the infant is 7 to 10 days old, unless there is a concomitant fracture. In that setting, stretches should begin at 3 to 4 weeks of age.[47]Waters PM. Update on management of pediatric brachial plexus palsy. J Pediatr Orthop B. 2005 Jul;14(4):233-44.
http://www.ncbi.nlm.nih.gov/pubmed/15931025?tool=bestpractice.com
[87]Abzug JM, Kozin SH. Evaluation and management of brachial plexus birth palsy. Orthop Clin North Am. 2014 Apr;45(2):225-32.
http://www.ncbi.nlm.nih.gov/pubmed/24684916?tool=bestpractice.com
[88]Buterbaugh KL, Shah AS. The natural history and management of brachial plexus birth palsy. Curr Rev Musculoskelet Med. 2016 Dec;9(4):418-26.
http://www.ncbi.nlm.nih.gov/pubmed/27680748?tool=bestpractice.com
[89]Frade F, Gómez-Salgado J, Jacobsohn L, et al. Rehabilitation of neonatal brachial plexus palsy: integrative literature review. J Clin Med. 2019 Jul 5;8(7):980.
https://www.mdpi.com/2077-0383/8/7/980/htm
http://www.ncbi.nlm.nih.gov/pubmed/31284431?tool=bestpractice.com
Parents are instructed in a home-based range-of-motion exercise programme, guided by weekly or bi-weekly formal therapy sessions.[46]Shenaq SM, Bullocks JM, Dhillon G, et al. Management of infant brachial plexus injuries. Clin Plast Surg. 2005 Jan;32(1):79-98, ix.
http://www.ncbi.nlm.nih.gov/pubmed/15636767?tool=bestpractice.com
[47]Waters PM. Update on management of pediatric brachial plexus palsy. J Pediatr Orthop B. 2005 Jul;14(4):233-44.
http://www.ncbi.nlm.nih.gov/pubmed/15931025?tool=bestpractice.com
[48]Clarke HM, Curtis CG. An approach to obstetrical brachial plexus injuries. Hand Clin. 1995 Nov;11(4):563-80.
http://www.ncbi.nlm.nih.gov/pubmed/8567739?tool=bestpractice.com
[49]Zafeiriou DI, Psychogiou K. Obstetrical brachial plexus palsy. Pediatr Neurol. 2008 Apr;38(4):235-42.
http://www.ncbi.nlm.nih.gov/pubmed/18358400?tool=bestpractice.com
[86]Vuillermin C, Bauer AS. Boston Children's Hospital approach to brachial plexus birth palsy. J Pediatr Orthop B. 2016 Jul;25(4):296-304.
http://www.ncbi.nlm.nih.gov/pubmed/27137763?tool=bestpractice.com
Success is impacted by the degree of nerve injury and recovery.
Parents should perform gentle passive motion of all of the joints of the upper extremity at home at the nappy change, several times per day. Shoulder external rotation stretches are particularly important.
Arrange monthly follow-up in a formal clinic setting to monitor recovery and ensure range of motion is being maintained. Various scales (e.g., the Toronto Test Score, Active Movement Scale) are used to numerically monitor recovery of arm function.[48]Clarke HM, Curtis CG. An approach to obstetrical brachial plexus injuries. Hand Clin. 1995 Nov;11(4):563-80.
http://www.ncbi.nlm.nih.gov/pubmed/8567739?tool=bestpractice.com
[53]Michelow BJ, Clarke HM, Curtis CG, et al. The natural history of obstetrical brachial plexus palsy. Plast Reconstr Surg. 1994 Apr;93(4):675-80.
http://www.ncbi.nlm.nih.gov/pubmed/8134425?tool=bestpractice.com
[54]Curtis C, Stephens D, Clarke HM, et al. The active movement scale: an evaluative tool for infants with obstetrical brachial plexus palsy. J Hand Surg Am. 2002 May;27(3):470-8.
http://www.ncbi.nlm.nih.gov/pubmed/12015722?tool=bestpractice.com
[55]Mallet J. Obstetrical paralysis of the brachial plexus. II. Therapeutics. Treatment of sequelae. Priority for the treatment of the shoulder. Method for the expression of results [in French]. Rev Chir Orthop Reparatrice Appar Mot. 1972;58:Suppl 1:166-8.
http://www.ncbi.nlm.nih.gov/pubmed/4263979?tool=bestpractice.com
[90]Chang KW, Justice D, Chung KC, et al. A systematic review of evaluation methods for neonatal brachial plexus palsy. J Neurosurg Pediatr. 2013 Oct;12(4):395-405.
http://www.ncbi.nlm.nih.gov/pubmed/23930602?tool=bestpractice.com
Most patients have relatively preserved hand and wrist function and develop reasonable elbow function; therefore, treatment is usually directed towards the shoulder.[46]Shenaq SM, Bullocks JM, Dhillon G, et al. Management of infant brachial plexus injuries. Clin Plast Surg. 2005 Jan;32(1):79-98, ix.
http://www.ncbi.nlm.nih.gov/pubmed/15636767?tool=bestpractice.com
[47]Waters PM. Update on management of pediatric brachial plexus palsy. J Pediatr Orthop B. 2005 Jul;14(4):233-44.
http://www.ncbi.nlm.nih.gov/pubmed/15931025?tool=bestpractice.com
[49]Zafeiriou DI, Psychogiou K. Obstetrical brachial plexus palsy. Pediatr Neurol. 2008 Apr;38(4):235-42.
http://www.ncbi.nlm.nih.gov/pubmed/18358400?tool=bestpractice.com
[86]Vuillermin C, Bauer AS. Boston Children's Hospital approach to brachial plexus birth palsy. J Pediatr Orthop B. 2016 Jul;25(4):296-304.
http://www.ncbi.nlm.nih.gov/pubmed/27137763?tool=bestpractice.com
[91]Hems TEJ, Savaridas T, Sherlock DA. The natural history of recovery of elbow flexion after obstetric brachial plexus injury managed without nerve repair. J Hand Surg Eur Vol. 2017 Sep;42(7):706-9.
http://www.ncbi.nlm.nih.gov/pubmed/28627963?tool=bestpractice.com
Special attention is given to maintenance of the motion of shoulder abduction and external rotation to avoid contracture. Stretches to maintain passive supination are also recommended.
Splinting of the hand and wrist may be used to prevent contracture in children with hand and wrist involvement.
Specialty care
Early referral to a BPBI clinic is imperative for oversight of the infant’s care.[92]Shah V, Coroneos CJ, Ng E. The evaluation and management of neonatal brachial plexus palsy. Paediatr Child Health. 2021 Dec;26(8):493-7.
https://www.doi.org/10.1093/pch/pxab083
http://www.ncbi.nlm.nih.gov/pubmed/34992702?tool=bestpractice.com
This facilitates serial examinations and timely surgical intervention if recovery is inadequate.[93]Nayak A, D'Souza A, Bhat AK, et al. Role of early referral and surgical intervention in brachial plexus birth palsy: awareness among obstetricians and pediatricians in a teaching hospital. Int Q Community Health Educ. 2020 Jul;40(4):363-6.
https://www.doi.org/10.1177/0272684X19883523
http://www.ncbi.nlm.nih.gov/pubmed/31652077?tool=bestpractice.com
[94]Schmieg S, Nguyen JC, Pehnke M, et al. Team approach: management of brachial plexus birth injury. JBJS Rev. 2020 Jul;8(7):e1900200.
http://www.ncbi.nlm.nih.gov/pubmed/32618739?tool=bestpractice.com
Severe injury at birth and/or poor recovery in infancy
Indications for, and timing of, nerve reconstruction procedures for BPBI remain controversial.[89]Frade F, Gómez-Salgado J, Jacobsohn L, et al. Rehabilitation of neonatal brachial plexus palsy: integrative literature review. J Clin Med. 2019 Jul 5;8(7):980.
https://www.mdpi.com/2077-0383/8/7/980/htm
http://www.ncbi.nlm.nih.gov/pubmed/31284431?tool=bestpractice.com
[94]Schmieg S, Nguyen JC, Pehnke M, et al. Team approach: management of brachial plexus birth injury. JBJS Rev. 2020 Jul;8(7):e1900200.
http://www.ncbi.nlm.nih.gov/pubmed/32618739?tool=bestpractice.com
[95]Malessy MJ, Pondaag W. Neonatal brachial plexus palsy with neurotmesis of C5 and avulsion of C6: supraclavicular reconstruction strategies and outcome. J Bone Joint Surg Am. 2014 Oct 15;96(20):e174.
http://www.ncbi.nlm.nih.gov/pubmed/25320204?tool=bestpractice.com
[96]Pondaag W, Malessy MJA. Evidence that nerve surgery improves functional outcome for obstetric brachial plexus injury. J Hand Surg Eur Vol. 2021 Mar;46(3):229-36.
https://www.doi.org/10.1177/1753193420934676
http://www.ncbi.nlm.nih.gov/pubmed/32588706?tool=bestpractice.com
Although certain instances clearly will require surgical intervention for any meaningful recovery to occur (nerve root avulsions or complete ruptures with no meaningful return of function), many children will have reasonable return of function on their own as time proceeds.[46]Shenaq SM, Bullocks JM, Dhillon G, et al. Management of infant brachial plexus injuries. Clin Plast Surg. 2005 Jan;32(1):79-98, ix.
http://www.ncbi.nlm.nih.gov/pubmed/15636767?tool=bestpractice.com
[47]Waters PM. Update on management of pediatric brachial plexus palsy. J Pediatr Orthop B. 2005 Jul;14(4):233-44.
http://www.ncbi.nlm.nih.gov/pubmed/15931025?tool=bestpractice.com
[48]Clarke HM, Curtis CG. An approach to obstetrical brachial plexus injuries. Hand Clin. 1995 Nov;11(4):563-80.
http://www.ncbi.nlm.nih.gov/pubmed/8567739?tool=bestpractice.com
[49]Zafeiriou DI, Psychogiou K. Obstetrical brachial plexus palsy. Pediatr Neurol. 2008 Apr;38(4):235-42.
http://www.ncbi.nlm.nih.gov/pubmed/18358400?tool=bestpractice.com
[86]Vuillermin C, Bauer AS. Boston Children's Hospital approach to brachial plexus birth palsy. J Pediatr Orthop B. 2016 Jul;25(4):296-304.
http://www.ncbi.nlm.nih.gov/pubmed/27137763?tool=bestpractice.com
[97]Hale HB, Bae DS, Waters PM. Current concepts in the management of brachial plexus birth palsy. J Hand Surg Am. 2010 Feb;35(2):322-31.
http://www.ncbi.nlm.nih.gov/pubmed/20141905?tool=bestpractice.com
[98]Borschel GH, Clarke HM. Obstetrical brachial plexus palsy. Plast Reconstr Surg. 2009 Jul;124(1 Suppl):144e-155e.
http://www.ncbi.nlm.nih.gov/pubmed/19568147?tool=bestpractice.com
One systematic review concluded that the evidence that nerve reconstruction improves outcomes compared with conservative management is weak, relying on low-quality observational studies.[96]Pondaag W, Malessy MJA. Evidence that nerve surgery improves functional outcome for obstetric brachial plexus injury. J Hand Surg Eur Vol. 2021 Mar;46(3):229-36.
https://www.doi.org/10.1177/1753193420934676
http://www.ncbi.nlm.nih.gov/pubmed/32588706?tool=bestpractice.com
Some authors have also highlighted a potential risk that some outcomes (e.g., elbow flexion) may be worse following surgical treatment.[99]Hems T. Commentary on: Evidence that nerve surgery improves functional outcome for obstetric brachial plexus injury. J Hand Surg Eur Vol. 2021 Mar;46(3):237-8.
http://www.ncbi.nlm.nih.gov/pubmed/33601971?tool=bestpractice.com
Some authors advocate early surgery at 3 months of age if the patient has not shown meaningful return of biceps, shoulder, or hand function.[77]Gilbert A. Repair of the brachial plexus in the obstetrical lesions of the newborn [in French]. Arch Pediatr. 2008 Mar;15(3):330-3.
http://www.ncbi.nlm.nih.gov/pubmed/18313907?tool=bestpractice.com
[100]Vekris MD, Lykissas MG, Beris AE, et al. Management of obstetrical brachial plexus palsy with early plexus microreconstruction and late muscle transfers. Microsurgery. 2008;28(4):252-61.
http://www.ncbi.nlm.nih.gov/pubmed/18381657?tool=bestpractice.com
[101]Gilbert A, Pivato G, Kheiralla T. Long-term results of primary repair of brachial plexus lesions in children. Microsurgery. 2006;26(4):334-42.
http://www.ncbi.nlm.nih.gov/pubmed/16634084?tool=bestpractice.com
[102]Birch R, Ahad N, Kono H, et al. Repair of obstetric brachial plexus palsy: results in 100 children. J Bone Joint Surg Br. 2005 Aug;87(8):1089-95.
http://www.ncbi.nlm.nih.gov/pubmed/16049245?tool=bestpractice.com
[103]Haerle M, Gilbert A. Management of complete obstetric brachial plexus lesions. J Pediatr Orthop. 2004 Mar-Apr;24(2):194-200.
http://www.ncbi.nlm.nih.gov/pubmed/15076607?tool=bestpractice.com
[104]Grossman JA. Early operative intervention for birth injuries to the brachial plexus. Semin Pediatr Neurol. 2000 Mar;7(1):36-43.
http://www.ncbi.nlm.nih.gov/pubmed/10749512?tool=bestpractice.com
Other authors have shown that natural recovery may continue beyond 3 months of age, demonstrating good functional results without nerve reconstruction surgery.[6]Smith NC, Rowan P, Benson LJ, et al. Neonatal brachial plexus palsy: outcome of absent biceps function at three months of age. J Bone Joint Surg Am. 2004 Oct;86-A(10):2163-70.
http://www.ncbi.nlm.nih.gov/pubmed/15466724?tool=bestpractice.com
[64]Waters PM. Comparison of the natural history, the outcome of microsurgical repair, and the outcome of operative reconstruction in brachial plexus birth palsy. J Bone Joint Surg Am. 1999 May;81(5):649-59.
http://www.ncbi.nlm.nih.gov/pubmed/10360693?tool=bestpractice.com
[105]Strombeck C, Krumlinde-Sundholm L, Forssberg H. Functional outcome at 5 years in children with obstetrical brachial plexus palsy with and without microsurgical reconstruction. Dev Med Child Neurol. 2000 Mar;42(3):148-57.
http://onlinelibrary.wiley.com/doi/10.1111/j.1469-8749.2000.tb00062.x/pdf
http://www.ncbi.nlm.nih.gov/pubmed/10755453?tool=bestpractice.com
[106]Nath RK, Liu X. Nerve reconstruction in patients with obstetric brachial plexus injury results in worsening of glenohumeral deformity: a case-control study of 75 patients. J Bone Joint Surg Br. 2009 May;91(5):649-54.
http://www.ncbi.nlm.nih.gov/pubmed/19407301?tool=bestpractice.com
No standardised treatment can be recommended at this time. In one comparative study, functional outcomes following brachial plexus reconstruction were better than functional outcomes of children with spontaneous recovery at 5 months of age.[64]Waters PM. Comparison of the natural history, the outcome of microsurgical repair, and the outcome of operative reconstruction in brachial plexus birth palsy. J Bone Joint Surg Am. 1999 May;81(5):649-59.
http://www.ncbi.nlm.nih.gov/pubmed/10360693?tool=bestpractice.com
However, another study demonstrated improvements in function after late (after 9 months) brachial plexus reconstruction.[107]Daly MC, Bauer AS, Lynch H, et al. Outcomes of late microsurgical nerve reconstruction for brachial plexus birth injury. J Hand Surg Am. 2020 Jun;45(6):555.e1-555.e9.
http://www.ncbi.nlm.nih.gov/pubmed/31928798?tool=bestpractice.com
Irreversible changes to muscle and motor endplates occur after 18 to 24 months of denervation.[108]Basit H, Ali CDM, Madhani NB. Erb palsy. 2022 Feb 27. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Feb 27.
https://www.ncbi.nlm.nih.gov/books/NBK513260
http://www.ncbi.nlm.nih.gov/pubmed/30020632?tool=bestpractice.com
Nerve regeneration occurs at a rate of approximately 1 mm per day.[109]Seddon HJ, Medawar PB, Smith H. Rate of regeneration of peripheral nerves in man. J Physiol. 1943 Sep 30;102(2):191-215.
https://www.doi.org/10.1113/jphysiol.1943.sp004027
http://www.ncbi.nlm.nih.gov/pubmed/16991601?tool=bestpractice.com
Surgical timing needs to take these time factors into account. The decision is based on the patient's recovery and the expertise and experience of the physician managing the patient's care. In general, children without full recovery by the age of 3 months are likely to have some residual impairment requiring ongoing treatment.[6]Smith NC, Rowan P, Benson LJ, et al. Neonatal brachial plexus palsy: outcome of absent biceps function at three months of age. J Bone Joint Surg Am. 2004 Oct;86-A(10):2163-70.
http://www.ncbi.nlm.nih.gov/pubmed/15466724?tool=bestpractice.com
[64]Waters PM. Comparison of the natural history, the outcome of microsurgical repair, and the outcome of operative reconstruction in brachial plexus birth palsy. J Bone Joint Surg Am. 1999 May;81(5):649-59.
http://www.ncbi.nlm.nih.gov/pubmed/10360693?tool=bestpractice.com
[105]Strombeck C, Krumlinde-Sundholm L, Forssberg H. Functional outcome at 5 years in children with obstetrical brachial plexus palsy with and without microsurgical reconstruction. Dev Med Child Neurol. 2000 Mar;42(3):148-57.
http://onlinelibrary.wiley.com/doi/10.1111/j.1469-8749.2000.tb00062.x/pdf
http://www.ncbi.nlm.nih.gov/pubmed/10755453?tool=bestpractice.com
[110]Annika J, Paul U, Anna-Lena L. Obstetric brachial plexus palsy - A prospective, population-based study of incidence, recovery and long-term residual impairment at 10 to 12 years of age. Eur J Paediatr Neurol. 2019 Jan;23(1):87-93.
https://www.doi.org/10.1016/j.ejpn.2018.06.006
http://www.ncbi.nlm.nih.gov/pubmed/30458977?tool=bestpractice.com
For babies with global plexus injuries and little to no recovery of hand function, surgery is typically recommended around 3 months of age.[96]Pondaag W, Malessy MJA. Evidence that nerve surgery improves functional outcome for obstetric brachial plexus injury. J Hand Surg Eur Vol. 2021 Mar;46(3):229-36.
https://www.doi.org/10.1177/1753193420934676
http://www.ncbi.nlm.nih.gov/pubmed/32588706?tool=bestpractice.com
[111]Thatte MR, Nayak NS, Hiremath AS. Management of birth brachial plexus injury including use of distal nerve transfers. J Hand Surg Asian Pac Vol. 2020 Sep;25(3):267-75.
http://www.ncbi.nlm.nih.gov/pubmed/32723053?tool=bestpractice.com
[112]Siqueira MG, Heise CO, Alencar GC, et al. Outcomes from primary surgical reconstruction of neonatal brachial plexus palsy in 104 children. Childs Nerv Syst. 2019 Feb;35(2):349-54.
http://www.ncbi.nlm.nih.gov/pubmed/30610478?tool=bestpractice.com
For children with Erb's palsy (C5/C6) and extended Erb's palsy (C5/C6/C7), surgery is recommended around 4 to 6 months of age.[96]Pondaag W, Malessy MJA. Evidence that nerve surgery improves functional outcome for obstetric brachial plexus injury. J Hand Surg Eur Vol. 2021 Mar;46(3):229-36.
https://www.doi.org/10.1177/1753193420934676
http://www.ncbi.nlm.nih.gov/pubmed/32588706?tool=bestpractice.com
[112]Siqueira MG, Heise CO, Alencar GC, et al. Outcomes from primary surgical reconstruction of neonatal brachial plexus palsy in 104 children. Childs Nerv Syst. 2019 Feb;35(2):349-54.
http://www.ncbi.nlm.nih.gov/pubmed/30610478?tool=bestpractice.com
Nerve grafting (removal of the damaged portion of the nerve and replacement with a portion of nerve from another area of the body) is preferred over neurolysis (clearing scar tissue from the nerve).[22]Smith BW, Daunter AK, Yang LJ, et al. An update on the management of neonatal brachial plexus palsy-replacing old paradigms: a review. JAMA Pediatr. 2018 Jun 1;172(6):585-91.
http://www.ncbi.nlm.nih.gov/pubmed/29710183?tool=bestpractice.com
[113]Lin JC, Schwentker-Colizza A, Curtis CG, et al. Final results of grafting versus neurolysis in obstetrical brachial plexus palsy. Plast Reconstr Surg. 2009 Mar;123(3):939-48.
http://www.ncbi.nlm.nih.gov/pubmed/19319058?tool=bestpractice.com
Nerve transfers offer another option for functional restoration. Nerve transfers may be utilised in conjunction with nerve grafting or in isolation for patients who do not have proximal roots available for grafting or who present late.[111]Thatte MR, Nayak NS, Hiremath AS. Management of birth brachial plexus injury including use of distal nerve transfers. J Hand Surg Asian Pac Vol. 2020 Sep;25(3):267-75.
http://www.ncbi.nlm.nih.gov/pubmed/32723053?tool=bestpractice.com
[114]Lara AM, Bhatia A, Correa JC, et al. Intercostal nerve transfers to the musculocutaneous - a reliable nerve transfer for restoration of elbow flexion in birth-related brachial plexus injuries. Indian J Plast Surg. 2020 Aug;53(2):254-9.
https://www.doi.org/10.1055/s-0040-1716186
http://www.ncbi.nlm.nih.gov/pubmed/32884191?tool=bestpractice.com
[115]Segal D, Cornwall R, Little KJ. Outcomes of spinal accessory-to-suprascapular nerve transfers for brachial plexus birth Injury. J Hand Surg Am. 2019 Jul;44(7):578-87.
http://www.ncbi.nlm.nih.gov/pubmed/30898464?tool=bestpractice.com
The home-based range-of-motion exercise programme must be continued after postoperative immobilisation is complete and must follow any range of motion restrictions based on the specific procedure performed.
Ongoing monitoring in childhood
Shoulder and upper extremity function is monitored with the modified Mallet classification, other range-of-motion measures, and Medical Research Council (MRC) strength assessment.[56]Abzug JM, Chafetz RS, Gaughan JP, et al. Shoulder function after medial approach and derotational humeral osteotomy in patients with brachial plexus birth palsy. J Pediatr Orthop. 2010 Jul-Aug;30(5):469-74.
http://www.ncbi.nlm.nih.gov/pubmed/20574265?tool=bestpractice.com
Children with BPBI may have limb length and girth discrepancies.[116]Bae DS, Ferretti M, Waters PM. Upper extremity size differences in brachial plexus birth palsy. Hand (N Y). 2008 Dec;3(4):297-303.
http://www.ncbi.nlm.nih.gov/pubmed/18780022?tool=bestpractice.com
[117]McDaid PJ, Kozin SH, Thoder JJ, et al. Upper extremity limb-length discrepancy in brachial plexus palsy. J Pediatr Orthop. 2002 May-Jun;22(3):364-6.
http://www.ncbi.nlm.nih.gov/pubmed/11961456?tool=bestpractice.com
The severity of the discrepancy correlates with the severity of the nerve injury.[117]McDaid PJ, Kozin SH, Thoder JJ, et al. Upper extremity limb-length discrepancy in brachial plexus palsy. J Pediatr Orthop. 2002 May-Jun;22(3):364-6.
http://www.ncbi.nlm.nih.gov/pubmed/11961456?tool=bestpractice.com
Elbow flexion contractures also frequently occur in children with BPBI.[118]Ho ES, Kim D, Klar K, et al. Prevalence and etiology of elbow flexion contractures in brachial plexus birth injury: a scoping review. J Pediatr Rehabil Med. 2019;12(1):75-86.
http://www.ncbi.nlm.nih.gov/pubmed/31006697?tool=bestpractice.com
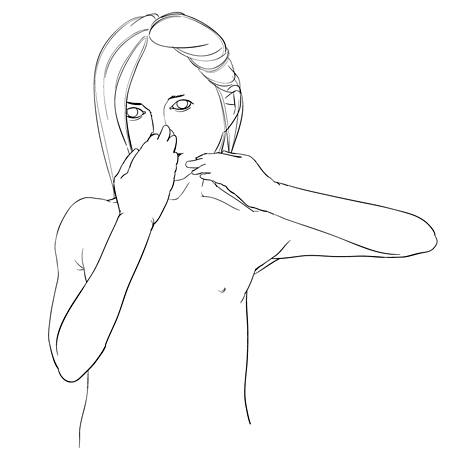
Although usually able to flex their elbow with good strength, patients can show difficulty with activities about the head, and will abduct their shoulder in order to touch their mouth. This is referred to as the 'trumpet sign' and demonstrates the lack of shoulder external rotation needed to perform these activities without shoulder abduction. The trumpet sign can also be associated with lack of forearm supination.[Figure caption and citation for the preceding image starts]: Trumpet sign (elevated elbow)Thomas Campbell by commission [Citation ends].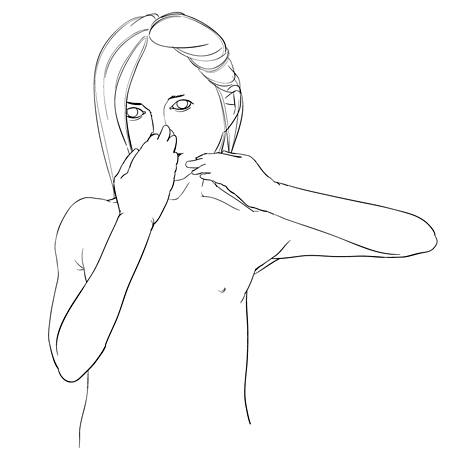
Monitoring is carried out for evidence of posterior shoulder subluxation, as the external rotators of the shoulder (supraspinatus, infraspinatus, and teres minor) are more severely involved than the internal rotators of the shoulder (pectoralis major, latissimus dorsi, teres major, and subscapularis) in patients with Erb's palsy. Patients who do not recover enough external rotation strength to counteract the internal rotators often show decreased function of the shoulder and arm.[46]Shenaq SM, Bullocks JM, Dhillon G, et al. Management of infant brachial plexus injuries. Clin Plast Surg. 2005 Jan;32(1):79-98, ix.
http://www.ncbi.nlm.nih.gov/pubmed/15636767?tool=bestpractice.com
[47]Waters PM. Update on management of pediatric brachial plexus palsy. J Pediatr Orthop B. 2005 Jul;14(4):233-44.
http://www.ncbi.nlm.nih.gov/pubmed/15931025?tool=bestpractice.com
[48]Clarke HM, Curtis CG. An approach to obstetrical brachial plexus injuries. Hand Clin. 1995 Nov;11(4):563-80.
http://www.ncbi.nlm.nih.gov/pubmed/8567739?tool=bestpractice.com
[49]Zafeiriou DI, Psychogiou K. Obstetrical brachial plexus palsy. Pediatr Neurol. 2008 Apr;38(4):235-42.
http://www.ncbi.nlm.nih.gov/pubmed/18358400?tool=bestpractice.com
[64]Waters PM. Comparison of the natural history, the outcome of microsurgical repair, and the outcome of operative reconstruction in brachial plexus birth palsy. J Bone Joint Surg Am. 1999 May;81(5):649-59.
http://www.ncbi.nlm.nih.gov/pubmed/10360693?tool=bestpractice.com
[86]Vuillermin C, Bauer AS. Boston Children's Hospital approach to brachial plexus birth palsy. J Pediatr Orthop B. 2016 Jul;25(4):296-304.
http://www.ncbi.nlm.nih.gov/pubmed/27137763?tool=bestpractice.com
[105]Strombeck C, Krumlinde-Sundholm L, Forssberg H. Functional outcome at 5 years in children with obstetrical brachial plexus palsy with and without microsurgical reconstruction. Dev Med Child Neurol. 2000 Mar;42(3):148-57.
http://onlinelibrary.wiley.com/doi/10.1111/j.1469-8749.2000.tb00062.x/pdf
http://www.ncbi.nlm.nih.gov/pubmed/10755453?tool=bestpractice.com
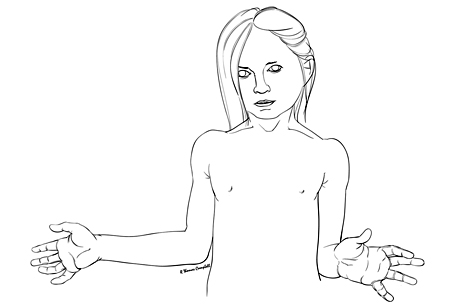
[Figure caption and citation for the preceding image starts]: Lack of external rotation after brachial plexus injuryThomas Campbell by commission [Citation ends].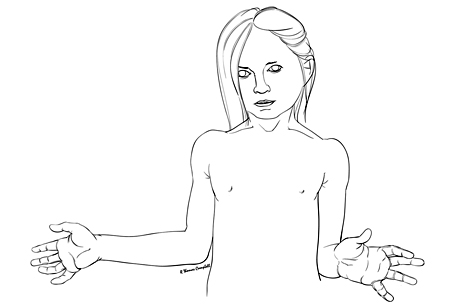 Additionally, denervated muscles have been shown to grow more slowly than the typical muscles, which contributes to contracture formation in children with BPBI.[119]Nikolaou S, Peterson E, Kim A, et al. Impaired growth of denervated muscle contributes to contracture formation following neonatal brachial plexus injury. J Bone Joint Surg Am. 2011 Mar 2;93(5):461-70.
http://www.ncbi.nlm.nih.gov/pubmed/21368078?tool=bestpractice.com
[120]Weekley H, Nikolaou S, Hu L, et al. The effects of denervation, reinnervation, and muscle imbalance on functional muscle length and elbow flexion contracture following neonatal brachial plexus injury. J Orthop Res. 2012 Aug;30(8):1335-42.
https://www.doi.org/10.1002/jor.22061
http://www.ncbi.nlm.nih.gov/pubmed/22227960?tool=bestpractice.com
Additionally, denervated muscles have been shown to grow more slowly than the typical muscles, which contributes to contracture formation in children with BPBI.[119]Nikolaou S, Peterson E, Kim A, et al. Impaired growth of denervated muscle contributes to contracture formation following neonatal brachial plexus injury. J Bone Joint Surg Am. 2011 Mar 2;93(5):461-70.
http://www.ncbi.nlm.nih.gov/pubmed/21368078?tool=bestpractice.com
[120]Weekley H, Nikolaou S, Hu L, et al. The effects of denervation, reinnervation, and muscle imbalance on functional muscle length and elbow flexion contracture following neonatal brachial plexus injury. J Orthop Res. 2012 Aug;30(8):1335-42.
https://www.doi.org/10.1002/jor.22061
http://www.ncbi.nlm.nih.gov/pubmed/22227960?tool=bestpractice.com
Signs of impending posterior subluxation include a decrease in passive external rotation of the shoulder (especially in adduction), shortening of the humeral segment (acromion to antecubital fold), asymmetric soft-tissue folds on the arm, a deep and asymmetric axilla, and a palpable humeral head posteriorly at the shoulder.[52]Moukoko D, Ezaki M, Wilkes D, et al. Posterior shoulder dislocation in infants with neonatal brachial plexus palsy. J Bone Joint Surg Am. 2004 Apr;86-A(4):787-93.
http://www.ncbi.nlm.nih.gov/pubmed/15069145?tool=bestpractice.com
[121]Kozin SH. Correlation between external rotation of the glenohumeral joint and deformity after brachial plexus birth palsy. J Pediatr Orthop. 2004 Mar-Apr;24(2):189-93.
http://www.ncbi.nlm.nih.gov/pubmed/15076606?tool=bestpractice.com
Orthopaedic treatments are directed towards maintaining the motion and function of the shoulder, elbow, wrist, and hand.
Parents should continue the home-based range-of-motion exercise programme, guided by weekly or bi-weekly formal therapy sessions as needed.
Secondary interventions: shoulder function
Choices concerning the most appropriate surgical procedure are individualised and are made by the treating surgical specialist. In infants and young children whose glenohumeral joint reduces in external rotation, the shoulder internal rotators may be injected with botulinum toxin type A and a shoulder spica cast applied in external rotation.[94]Schmieg S, Nguyen JC, Pehnke M, et al. Team approach: management of brachial plexus birth injury. JBJS Rev. 2020 Jul;8(7):e1900200.
http://www.ncbi.nlm.nih.gov/pubmed/32618739?tool=bestpractice.com
[111]Thatte MR, Nayak NS, Hiremath AS. Management of birth brachial plexus injury including use of distal nerve transfers. J Hand Surg Asian Pac Vol. 2020 Sep;25(3):267-75.
http://www.ncbi.nlm.nih.gov/pubmed/32723053?tool=bestpractice.com
[122]Buchanan PJ, Grossman JAI, Price AE, et al. The use of botulinum toxin injection for brachial plexus birth injuries: a systematic review of the literature. Hand (N Y). 2019 Mar;14(2):150-4.
http://www.ncbi.nlm.nih.gov/pubmed/29529875?tool=bestpractice.com
[123]Gobets D, Beckerman H, de Groot V, et al. Indications and effects of botulinum toxin A for obstetric brachial plexus injury: a systematic literature review. Dev Med Child Neurol. 2010 Jun;52(6):517-28.
http://onlinelibrary.wiley.com/doi/10.1111/j.1469-8749.2009.03607.x/full
http://www.ncbi.nlm.nih.gov/pubmed/20163432?tool=bestpractice.com
[124]Greenhill DA, Wissinger K, Trionfo A, et al. External rotation predicts outcomes after closed glenohumeral joint reduction with botulinum toxin type A in brachial plexus birth palsy. J Pediatr Orthop. 2018 Jan;38(1):32-7.
http://www.ncbi.nlm.nih.gov/pubmed/26886458?tool=bestpractice.com
This provides a prolonged, static stretch of the internal rotators. The temporary weakening of the internal rotators allows time for further recovery of the external rotators. The goal is to have more balanced forces about the glenohumeral joint when the effects of the botulinum toxin type A dissipate. Botulinum toxin injection is most likely to be successful in patients who still have at least 30 degrees of passive shoulder external rotation.[124]Greenhill DA, Wissinger K, Trionfo A, et al. External rotation predicts outcomes after closed glenohumeral joint reduction with botulinum toxin type A in brachial plexus birth palsy. J Pediatr Orthop. 2018 Jan;38(1):32-7.
http://www.ncbi.nlm.nih.gov/pubmed/26886458?tool=bestpractice.com
However, most available evidence is low quality, and additional studies are needed.[122]Buchanan PJ, Grossman JAI, Price AE, et al. The use of botulinum toxin injection for brachial plexus birth injuries: a systematic review of the literature. Hand (N Y). 2019 Mar;14(2):150-4.
http://www.ncbi.nlm.nih.gov/pubmed/29529875?tool=bestpractice.com
[123]Gobets D, Beckerman H, de Groot V, et al. Indications and effects of botulinum toxin A for obstetric brachial plexus injury: a systematic literature review. Dev Med Child Neurol. 2010 Jun;52(6):517-28.
http://onlinelibrary.wiley.com/doi/10.1111/j.1469-8749.2009.03607.x/full
http://www.ncbi.nlm.nih.gov/pubmed/20163432?tool=bestpractice.com
Children under the age of 5 with posterior shoulder subluxation or dislocation can be treated with muscle lengthening (pectoralis major and subscapularis), muscle transfers (latissimus dorsi and teres major), and/or joint reduction.[125]Waters PM, Bae DS. The early effects of tendon transfers and open capsulorrhaphy on glenohumeral deformity in brachial plexus birth palsy. J Bone Joint Surg Am. 2008 Oct;90(10):2171-9.
http://www.ncbi.nlm.nih.gov/pubmed/18829915?tool=bestpractice.com
[126]van Kooten EO, Fortuin S, Winters HA, et al. Results of latissimus dorsi transfer in obstetrical brachial plexus injury. Tech Hand Up Extrem Surg. 2008 Sep;12(3):195-9.
http://www.ncbi.nlm.nih.gov/pubmed/18776785?tool=bestpractice.com
[127]Waters PM, Bae DS. Effect of tendon transfers and extra-articular soft-tissue balancing on glenohumeral development in brachial plexus birth palsy. J Bone Joint Surg Am. 2005 Feb;87(2):320-5.
http://www.ncbi.nlm.nih.gov/pubmed/15687154?tool=bestpractice.com
[128]Pagnotta A, Haerle M, Gilbert A. Long-term results on abduction and external rotation of the shoulder after latissimus dorsi transfer for sequelae of obstetric palsy. Clin Orthop Relat Res. 2004 Sep;(426):199-205.
http://www.ncbi.nlm.nih.gov/pubmed/15346074?tool=bestpractice.com
[129]Hoffer MM, Wickenden R, Roper B. Brachial plexus birth palsies: results of tendon transfers to the rotator cuff. J Bone Joint Surg Am. 1978 Jul;60(5):691-5.
http://www.ncbi.nlm.nih.gov/pubmed/681392?tool=bestpractice.com
[130]Alluri RK, Lightdale-Miric N, Meisel E, et al. Functional outcomes of tendon transfer for brachial plexus birth palsy using the Hoffer technique. Bone Joint J. 2020 Feb;102-B(2):246-53.
http://www.ncbi.nlm.nih.gov/pubmed/32009423?tool=bestpractice.com
Arthroscopic treatments have also been shown to be effective in improving shoulder function by release of the subscapularis tendon with and without latissimus dorsi and teres major transfer.[131]Pearl ML, Edgerton BW, Kazimiroff PA, et al. Arthroscopic release and latissimus dorsi transfer for shoulder internal rotation contractures and glenohumeral deformity secondary to brachial plexus birth palsy. J Bone Joint Surg Am. 2006 Mar;88(3):564-74.
http://www.ncbi.nlm.nih.gov/pubmed/16510824?tool=bestpractice.com
[132]Pearl ML. Arthroscopic release of shoulder contracture secondary to birth palsy: an early report on findings and surgical technique. Arthroscopy. 2003 Jul-Aug;19(6):577-82.
http://www.ncbi.nlm.nih.gov/pubmed/12861195?tool=bestpractice.com
[133]Pedowitz DI, Gibson B, Williams GR, et al. Arthroscopic treatment of posterior glenohumeral joint subluxation resulting from brachial plexus birth palsy. J Shoulder Elbow Surg. 2007 Jan-Feb;16(1):6-13.
http://www.ncbi.nlm.nih.gov/pubmed/17055299?tool=bestpractice.com
[134]Kozin SH, Boardman MJ, Chafetz RS, et al. Arthroscopic treatment of internal rotation contracture and glenohumeral dysplasia in children with brachial plexus birth palsy. J Shoulder Elbow Surg. 2010 Jan;19(1):102-10.
http://www.ncbi.nlm.nih.gov/pubmed/19664938?tool=bestpractice.com
[135]Ruyer J, Grosclaude S, Lacroix P, et al. Arthroscopic isolated capsular release for shoulder contracture after brachial plexus birth palsy: clinical outcomes in a prospective cohort of 28 children with 2 years' follow-up. J Shoulder Elbow Surg. 2018 Aug;27(8):e243-51.
http://www.ncbi.nlm.nih.gov/pubmed/29609998?tool=bestpractice.com
Similar findings have been noted following open glenohumeral release.[136]Burnier M, Le Hanneur M, Cambon-Binder A, et al. Isolated open anterior shoulder release in brachial plexus birth palsy. J Shoulder Elbow Surg. 2019 Jul;28(7):1347-55.
http://www.ncbi.nlm.nih.gov/pubmed/30981548?tool=bestpractice.com
Some remodelling of the posterior glenoid and improved humeral head position can be expected, along with some remodelling of the humeral head.[66]Reading BD, Laor T, Salisbury SR, et al. Quantification of humeral head deformity following neonatal brachial plexus palsy. J Bone Joint Surg Am. 2012 Sep 19;94(18):e136(1-8).
http://www.ncbi.nlm.nih.gov/pubmed/22992884?tool=bestpractice.com
[125]Waters PM, Bae DS. The early effects of tendon transfers and open capsulorrhaphy on glenohumeral deformity in brachial plexus birth palsy. J Bone Joint Surg Am. 2008 Oct;90(10):2171-9.
http://www.ncbi.nlm.nih.gov/pubmed/18829915?tool=bestpractice.com
[127]Waters PM, Bae DS. Effect of tendon transfers and extra-articular soft-tissue balancing on glenohumeral development in brachial plexus birth palsy. J Bone Joint Surg Am. 2005 Feb;87(2):320-5.
http://www.ncbi.nlm.nih.gov/pubmed/15687154?tool=bestpractice.com
[136]Burnier M, Le Hanneur M, Cambon-Binder A, et al. Isolated open anterior shoulder release in brachial plexus birth palsy. J Shoulder Elbow Surg. 2019 Jul;28(7):1347-55.
http://www.ncbi.nlm.nih.gov/pubmed/30981548?tool=bestpractice.com
[137]Jönsson K, Werner M, Roos F, et al. Development of the glenohumeral joint after subscapular release and open relocation in children with brachial plexus birth palsy: long-term results in 61 patients. J Shoulder Elbow Surg. 2019 Oct;28(10):1983-90.
http://www.ncbi.nlm.nih.gov/pubmed/31085034?tool=bestpractice.com
Additionally, functional capabilities will dramatically improve in overhead, at-the-head, and/or external rotation activities.[136]Burnier M, Le Hanneur M, Cambon-Binder A, et al. Isolated open anterior shoulder release in brachial plexus birth palsy. J Shoulder Elbow Surg. 2019 Jul;28(7):1347-55.
http://www.ncbi.nlm.nih.gov/pubmed/30981548?tool=bestpractice.com
[138]Louden EJ, Broering CA, Mehlman CT, et al. Meta-analysis of function after secondary shoulder surgery in neonatal brachial plexus palsy. J Pediatr Orthop. 2013 Sep;33(6):656-63.
http://www.ncbi.nlm.nih.gov/pubmed/23872798?tool=bestpractice.com
[139]Brogan DM, Leversedge FJ. Surgical technique and anatomical considerations for the modified L'Episcopo tendon transfer. Hand (N Y). 2019 Jan;14(1):34-41.
https://www.doi.org/10.1177/1558944718803746
http://www.ncbi.nlm.nih.gov/pubmed/30295084?tool=bestpractice.com
[140]El-Gammal TA, Ali AE, Kotb MM, et al. Long-term evaluation of teres major to infraspinatus transfer for treatment of shoulder sequelae in obstetrical brachial plexus palsy. Ann Plast Surg. 2020 May;84(5):565-9.
http://www.ncbi.nlm.nih.gov/pubmed/32167943?tool=bestpractice.com
[141]Maurya S, Bhandari PS, Chaitanya S. Conjoint muscle transfer and subscapularis slide in brachial plexus birth palsy: clinical outcomes in shoulder functions. Med J Armed Forces India. 2021 Apr;77(2):181-6.
http://www.ncbi.nlm.nih.gov/pubmed/33867635?tool=bestpractice.com
[142]Maurel N, Diop A, Lallemant-Dudek P, et al. Upper limb kinematics after latissimus dorsi transfer in children with brachial plexus birth palsy. Clin Biomech (Bristol, Avon). 2021 Jul;87:105413.
http://www.ncbi.nlm.nih.gov/pubmed/34174673?tool=bestpractice.com
[143]Russo SA, Richardson RT, Richards JG, et al. Effect of glenohumeral reduction type combined with tendon transfer for brachial plexus injury on objective, functional, and patient-reported outcomes. J Hand Surg Am. 2021 Jul;46(7):624.e1-624.e11.
http://www.ncbi.nlm.nih.gov/pubmed/33526294?tool=bestpractice.com
[144]Shahcheraghi GH, Javid M, Zamir-Azad M. The outcome of soft-tissue release and tendon transfer in shoulders with brachial plexus birth palsy. JSES Int. 2021 Sep;5(5):905-11.
https://www.doi.org/10.1016/j.jseint.2021.05.004
http://www.ncbi.nlm.nih.gov/pubmed/34505104?tool=bestpractice.com
However, internal rotation is more limited as a result of these procedures, and deficits in midline function (toileting, zipping/buttoning trousers, and obtaining objects from the back pocket) are a potential complication.[131]Pearl ML, Edgerton BW, Kazimiroff PA, et al. Arthroscopic release and latissimus dorsi transfer for shoulder internal rotation contractures and glenohumeral deformity secondary to brachial plexus birth palsy. J Bone Joint Surg Am. 2006 Mar;88(3):564-74.
http://www.ncbi.nlm.nih.gov/pubmed/16510824?tool=bestpractice.com
[140]El-Gammal TA, Ali AE, Kotb MM, et al. Long-term evaluation of teres major to infraspinatus transfer for treatment of shoulder sequelae in obstetrical brachial plexus palsy. Ann Plast Surg. 2020 May;84(5):565-9.
http://www.ncbi.nlm.nih.gov/pubmed/32167943?tool=bestpractice.com
[145]Greenhill DA, Trionfo A, Ramsey FV, et al. Postoperative loss of midline function in brachial plexus birth palsy. J Hand Surg Am. 2018 Jun;43(6):565.e1-565.e10.
https://www.doi.org/10.1016/j.jhsa.2017.10.041
http://www.ncbi.nlm.nih.gov/pubmed/29223630?tool=bestpractice.com
[146]Abzug JM, Wyrick-Glover TO, Case AL, et al. Loss of midline function in brachial plexus birth palsy patients. J Pediatr Orthop. 2019 Mar;39(3):e232-5.
http://www.ncbi.nlm.nih.gov/pubmed/30211803?tool=bestpractice.com
[147]Abzug JM, Miller E, Case AL, et al. Single versus double tendon transfer to improve shoulder external rotation during the treatment of brachial plexus birth palsy. Hand (N Y). 2022 Jan;17(1):55-9.
http://www.ncbi.nlm.nih.gov/pubmed/32188298?tool=bestpractice.com
Patients older than 8 years with longer-standing shoulder dislocation or subluxation will not show remodelling and are often better served with an external rotation humeral osteotomy that will allow better arm position and function in a similar fashion to tendon transfers but with no attempt made to anatomically restore the integrity of the shoulder joint.[56]Abzug JM, Chafetz RS, Gaughan JP, et al. Shoulder function after medial approach and derotational humeral osteotomy in patients with brachial plexus birth palsy. J Pediatr Orthop. 2010 Jul-Aug;30(5):469-74.
http://www.ncbi.nlm.nih.gov/pubmed/20574265?tool=bestpractice.com
[148]Waters PM, Bae DS. The effect of derotational humeral osteotomy on global shoulder function in brachial plexus birth palsy. J Bone Joint Surg Am. 2006 May;88(5):1035-42.
http://www.ncbi.nlm.nih.gov/pubmed/16651578?tool=bestpractice.com
[149]Ruhmann O, Gosse F, Schmolke S, et al. Osteotomy of the humerus to improve external rotation in nine patients with brachial plexus palsy. Scand J Plast Reconstr Surg Hand Surg. 2002;36(6):349-55.
http://www.ncbi.nlm.nih.gov/pubmed/12564814?tool=bestpractice.com
Children aged between 5 and 8 may be indicated for any of these procedures depending on the severity of glenohumeral dysplasia and their clinical presentation. Ages 5 and 8 are not definitive age cutoffs, rather a general guide for which procedures are most commonly indicated in those age groups. The patient's active and passive range of motion, glenohumeral dysplasia severity, and patient-specific functional goals should all be considered in determining the most appropriate procedure.
Secondary interventions: elbow, forearm, wrist, and hand function
Choices concerning the most appropriate surgical procedure are individualised and are made by the treating surgical specialist.
Tendon transfers or other secondary procedures to other areas of the elbow, forearm, wrist, or fingers may be needed to improve function in these areas as well.[150]Duclos L, Gilbert A. Restoration of wrist extension by tendon transfer in cases of obstetrical brachial plexus palsy. Ann Chir Main Memb Super. 1999;18(1):7-12.
http://www.ncbi.nlm.nih.gov/pubmed/10941390?tool=bestpractice.com
[151]DeDeugd CM, Shin AY, Shaughnessy WJ. Derotational pronation-producing osteotomy of the radius and biceps tendon rerouting for supination contractures in neonatal brachial plexus palsy patients. Tech Hand Up Extrem Surg. 2018 Mar;22(1):10-14.
http://www.ncbi.nlm.nih.gov/pubmed/29369125?tool=bestpractice.com
[152]Clippinger BB, Plucknette BF, Soldado F, et al. The one-bone forearm in children: surgical technique and a retrospective review of outcomes. J Hand Surg Am. 2022 Feb;47(2):189.e1-189.e9.
http://www.ncbi.nlm.nih.gov/pubmed/34112543?tool=bestpractice.com
Tendon transfers can be considered for children with an appropriate and expendable donor. Tendon transfer (unlike nerve surgery) is not time-sensitive, so can be considered as second-line for children who were not candidates for or who did not see significant improvements with nerve surgery, as long as passive motion is maintained or can be restored.
Patients who lack elbow flexion may be candidates for bipolar latissimus dorsi flexorplasty if they have a functioning latissimus dorsi.[153]Loeffler BJ, Lewis DR. Restoration of elbow flexion. Hand Clin. 2016 Aug;32(3):311-21.
http://www.ncbi.nlm.nih.gov/pubmed/27387075?tool=bestpractice.com
Management of residual deficits in the forearm is largely dictated by the passive range of motion. Supination deformity may be addressed with biceps rerouting if passive motion is maintained. If passive motion is limited, osteotomy of the radius or radius and ulna may be added to correct the deformity. One-bone forearm osteotomy is not as widely used, but may be an option for patients with severe deformity and lack of passive forearm rotation.[152]Clippinger BB, Plucknette BF, Soldado F, et al. The one-bone forearm in children: surgical technique and a retrospective review of outcomes. J Hand Surg Am. 2022 Feb;47(2):189.e1-189.e9.
http://www.ncbi.nlm.nih.gov/pubmed/34112543?tool=bestpractice.com
Pronation deformity is generally better tolerated by patients than supination deformity.
Lack of wrist extension may be treated with tendon transfer in some patients.[154]Rondon AJ, Aversano MW, Kluemper CT, et al. Flexor digitorum superficialis tendon transfer for wrist extension. JBJS Essent Surg Tech. 2021 Oct-Dec;11(4):e21.
https://www.ncbi.nlm.nih.gov/pmc/articles/pmid/35186438
http://www.ncbi.nlm.nih.gov/pubmed/35186438?tool=bestpractice.com
Many of the typical tendon transfer donors are not available in patients with BPBI, but flexor digitorum superficialis to the long and ring fingers may be transferred to the long finger metacarpal for restoration of wrist extension in patients with normal flexor digitorum superficialis and flexor digitorum profundus function.[154]Rondon AJ, Aversano MW, Kluemper CT, et al. Flexor digitorum superficialis tendon transfer for wrist extension. JBJS Essent Surg Tech. 2021 Oct-Dec;11(4):e21.
https://www.ncbi.nlm.nih.gov/pmc/articles/pmid/35186438
http://www.ncbi.nlm.nih.gov/pubmed/35186438?tool=bestpractice.com
Occasionally, wrist arthrodesis may be considered in skeletally-mature patients with no available donors for tendon transfer.
Botulinum toxin type A injections have also been used for the elbow flexors in infants with co-contraction of the elbow flexors and extensors.[155]Ramachandran M, Eastwood DM. Botulinum toxin and its orthopaedic applications. J Bone Joint Surg Br. 2006;88:981-7.
http://www.ncbi.nlm.nih.gov/pubmed/16877592?tool=bestpractice.com
[156]Shin YB, Shin MJ, Chang JH, et al. Effects of botulinum toxin on reducing the co-contraction of antagonists in birth brachial plexus palsy. Ann Rehabil Med. 2014;38:127-31.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3953355
http://www.ncbi.nlm.nih.gov/pubmed/24639937?tool=bestpractice.com
[157]Morscher MA, Thomas MD, Sahgal S, et al. Onabotulinum toxin type A injection into the triceps unmasks elbow flexion in infant brachial plexus birth palsy: A retrospective observational cohort study. Medicine (Baltimore). 2020 Aug 21;99(34):e21830.
https://www.doi.org/10.1097/MD.0000000000021830
http://www.ncbi.nlm.nih.gov/pubmed/32846828?tool=bestpractice.com
Additionally, botulinum toxin injection and serial casting has been used to reduce elbow flexion contractures in older children.[118]Ho ES, Kim D, Klar K, et al. Prevalence and etiology of elbow flexion contractures in brachial plexus birth injury: a scoping review. J Pediatr Rehabil Med. 2019;12(1):75-86.
http://www.ncbi.nlm.nih.gov/pubmed/31006697?tool=bestpractice.com
[122]Buchanan PJ, Grossman JAI, Price AE, et al. The use of botulinum toxin injection for brachial plexus birth injuries: a systematic review of the literature. Hand (N Y). 2019 Mar;14(2):150-4.
http://www.ncbi.nlm.nih.gov/pubmed/29529875?tool=bestpractice.com
[123]Gobets D, Beckerman H, de Groot V, et al. Indications and effects of botulinum toxin A for obstetric brachial plexus injury: a systematic literature review. Dev Med Child Neurol. 2010 Jun;52(6):517-28.
http://onlinelibrary.wiley.com/doi/10.1111/j.1469-8749.2009.03607.x/full
http://www.ncbi.nlm.nih.gov/pubmed/20163432?tool=bestpractice.com
 Additionally, denervated muscles have been shown to grow more slowly than the typical muscles, which contributes to contracture formation in children with BPBI.[119][120]
Additionally, denervated muscles have been shown to grow more slowly than the typical muscles, which contributes to contracture formation in children with BPBI.[119][120]