Differentials
Common
Alzheimer's dementia
History
short-term episodic memory loss (e.g., repetitive questioning, misplacing belongings) in early disease, visuospatial dysfunction (e.g., becoming lost in familiar places, not recognising people), language problems (e.g., difficulty naming things, difficulty speaking), loss of insight, mild personality changes (e.g., apathy, depression), long-term memory problems with progression of disease, prosopagnosia, autoprosopagnosia, personality/social conduct and motor function usually preserved until late stages
Exam
significant short-term memory deficits (e.g., trouble recalling lists of words or reconstructing a two-dimensional figure shown previously from memory), visuospatial deficits, acalculia
1st investigation
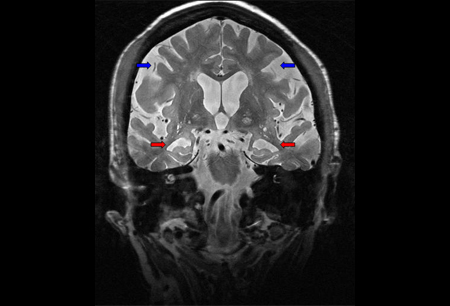
- MRI brain:
atrophy in medial temporal lobes (hippocampi) and inferolateral temporal lobes,[90] parietal lobes, and posterior cingulate gyrus, dilation of the perihippocampal fissure,[90] atrophy in frontal lobes later in the disease; include T1 axial/coronal and/or sagittal, T2 axial, fluid-attenuated inversion-recovery (FLAIR) axial/coronal, haemosiderin sequence (e.g., gradient echo)
More
Other investigations
- neuropsychological testing:
evidence of significant short-term memory deficits
- cerebrospinal fluid (CSF) testing for Abeta42, total-tau, and phosphorylated tau ratios:
CSF tau levels are elevated and Abeta 42 levels are decreased in AD
More - genetic testing:
presenilin-1 (PS1), presenilin-2 (PS2), or amyloid precursor protein (APP) mutation
More
Vascular dementia
History
risk factors present (i.e., hypertension, diabetes, hypercholesterolaemia, cardiac disease, and prior stroke), may have progressive stepwise cognitive decline, or gradual cognitive decline in small vessel disease; cognitive deficits vary according to area of the brain affected, may include difficulty problem solving, perseveration, disinhibition, and slowed processing; depression, hallucinations, and delusions; may report gait changes, poor balance, falls[91]
Exam
frontal pattern of memory loss with impaired retrieval but intact encoding, aphasia, homonymous hemianopsia, hemiparesis, hemisensory loss, apraxia, frontal executive deficits, visuospatial deficits, neglect[91]
1st investigation
- MRI/CT brain:
hypodensities within brain parenchyma on CT and T1-weighted MRI; focal ischaemic infarcts and/or small vessel ischaemic disease with hyperintensities on T2-weighted MRI
Other investigations
- neuropsychological testing:
impaired retrieval but intact encoding, frontal executive deficits
Dementia with Lewy bodies
History
Exam
1st investigation
- MRI brain:
non-specific atrophy, often more posterior
More - brain CT-SPECT:
hypometabolism of parietal-occipital cortex
Other investigations
Traumatic brain injury
History
<4-week interval between head trauma with loss of consciousness and development of symptoms; headache, dizziness, fatigue, noise intolerance, neuropsychiatric symptoms (e.g., irritability, depression, insomnia, anxiety), symptoms of basal skull fracture (e.g., 'panda' eyes, cerebrospinal fluid leakage from the ear or nose).[135][136]
Exam
inattentiveness, lethargy, papilloedema, aphasia, hemiplegia, focal weakness, signs of basal skull fracture (haemotympanum, 'panda' eyes, cerebrospinal fluid leakage from the ear or nose, Battle's sign).[135]
1st investigation
- MRI/CT brain:
brain lesions (anterior frontal and temporal contusions, corpus callosal, and Duret's haemorrhages) or skull fracture
More
Other investigations
- CT/MR angiography:
carotid dissection[135]
Hypothyroidism
History
forgetfulness, neuropsychiatric symptoms (e.g., depression, insomnia, irritability, emotional lability), myopathy, systemic symptoms associated with low thyroid (e.g., cold intolerance, hair loss, lethargy)[137]
Exam
inattentiveness, visuospatial deficits, ataxia, dry skin, pretibial myxoedema, delayed relaxation of deep tendon reflexes, hearing impairment, peripheral neuropathy, cerebellar deficits (e.g., limb ataxia)[138]
1st investigation
Other investigations
- thyroglobulin and thyroid peroxidase antibodies:
positive in Hashimoto’s thyroiditis
More
Hypoxic injury after cardiac arrest
History
loss of consciousness and/or coma in the setting of cardiac arrest
Exam
often severe amnesia post-arrest, immediate amnesia for short-term memory that often improves quickly over days, and chronic impairment in memory, inattentiveness, impaired arousability, frontal executive deficits, visuospatial deficits, mild deficits in tapping motor speed and dexterity, and motor control, all secondary to cardiac arrest[20]
1st investigation
- MRI brain:
hyperintensity in the superficial layers of the cortex (cortical laminae) on diffusion-weighted imaging sequence[20]
Other investigations
- neuropsychological testing:
transient episodic memory loss or chronic impairment in working and episodic memory, frontal executive deficits
Ischaemic stroke
History
presence of multiple stroke risk factors (i.e., advanced age, hypertension, coronary artery disease, high cholesterol, diabetes, prior stroke), sudden onset of symptoms, mental status changes, visual field cut, slurred speech; anterior thalamic infarcts may result in chronic symptoms of apathy, perseveration, and amnesia, whereas certain thalamic infarcts may lead to executive dysfunction[139]
Exam
depends on location of stroke, aphasia, ataxia, dysarthria, homonymous hemianopsia, facial weakness, hemiplegia, limb ataxia, focal weakness, numbness
1st investigation
- CT brain without contrast:
may be normal or demonstrate hypoattenuation (darkness) of the brain parenchyma; loss of grey matter-white matter differentiation and sulcal effacement; hyperattenuation (brightness) in an artery indicates a clot within the vessel lumen
More - MRI brain:
hyperintensity on diffusion-weighted imaging, usually with corresponding hypointensity on apparent diffusion coefficient sequences
More
Other investigations
- perfusion CT scan brain:
perfusion defects (often larger than ischaemic penumbra)
More - CT/MR angiography head and neck:
may show intracranial vessel thrombosis and/or cerebrovascular disease in anterior (carotid) or posterior (vertebrobasilar system) circulation
- echocardiogram/Holter monitor:
atrial thrombus or patent foramen ovale in patients <50 years of age may be seen on echo; source of embolus such as atrial fibrillation may be seen on Holter
- neuropsychological testing:
episodic memory impairment in hippocampal or anterior thalamic infarcts
Haemorrhagic stroke
History
presence of risk factors (e.g., hypertension, amyloid angiopathy, venous sinus thrombosis, haemorrhagic tumour, arteriovenous malformation), sudden onset of severe headache, lethargy, focal weakness, or numbness within minutes
Exam
focal deficits vary depending on location of the bleed: cortical haemorrhage in dominant hemisphere results in aphasia whereas haemorrhage in the non-dominant hemisphere may result in neglect and anosognosia, subcortical haemorrhages lead to contralateral weakness and/or sensory loss, brain stem haemorrhages can result in coma and death
1st investigation
- CT brain without contrast:
subcortical haematoma (basal ganglia and thalamus) in haemorrhagic stroke related to hypertension; lobar haemorrhage present in amyloid angiopathy, haemorrhagic tumour, aneurysmal bleed and cortical venous thrombosis; arteriovascular malformations may occur cortically or subcortically depending on the location
Other investigations
- MRI brain:
subcortical haematoma (basal ganglia and thalamus) in haemorrhagic stroke related to hypertension; lobar haemorrhage present in amyloid angiopathy, haemorrhagic tumour, and cortical venous thrombosis; arteriovascular malformations may occur cortically or subcortically depending on the location; gradient echo MRI sequences may reveal micro-haemorrhages in cases of haemorrhage secondary to amyloid angiopathy
- CT angiography:
arteriovenous malformation or venous cavernoma
Seizures
History
presence of risk factors (e.g., prior history of head injury, developmental delay, infantile febrile seizures, prior meningoencephalitis, intra-parenchymal mass lesions such as tumour); repeated, stereotyped episodes of altered consciousness (may be partial complex seizures or absence seizures) that may be accompanied by generalised tonic-clonic motor activity (generalised tonic-clonic seizures); patients with temporal lobe epilepsy suffer from chronic deficits of encoding, storage, and retrieval of new information in addition to memory loss during the seizure[21]
Exam
focal neurological deficits, aphasia, hemiparesis
1st investigation
- electroencephalogram (EEG):
focal epileptiform activity or slowing (partial complex seizures); generalised epileptiform activity or slowing (generalised tonic-clonic seizures)
More
Other investigations
- MRI brain:
may show focal lesion (such as brain tumour), developmental anomaly (e.g., cortical dysplasia, heterotopia), or regions of encephalomalacia; diffusion-weighted imaging sequence may show regions of hyperintensity, particularly in the cortex
- cerebrospinal fluid examination:
elevated proteins and WBC count in cases of seizures related to central nervous system infection
- neuropsychological testing:
chronic deficits of encoding, storage, and retrieval of new information in temporal lobe epilepsy
Migraine
History
episodes of repeated unilateral, throbbing head pain, which may or may not be accompanied by a visual aura, typically associated with nausea, vomiting, phonophobia and/or photophobia, specific triggers (e.g., wine, cheese), cognitive symptoms including memory loss, duration of symptoms may last 4 to 72 hours[140]
Exam
diagnosis based on history and tests
1st investigation
- no tests:
clinical diagnosis
Other investigations
Vitamin B12 deficiency
History
presence of risk factors (e.g., strict vegan diet without vitamin supplements, malnutrition, pernicious anaemia, extensive bowel surgery, institutionalisation, anaemia, gastric atrophy), vision loss in one eye, cognitive impairment (e.g., irritability, apathy, somnolence, suspiciousness, emotional instability, confusion)[127]
Exam
diminished large fibre sensation (proprioception and vibration), lower extremity numbness, gait unsteadiness, hyporeflexia, positive Babinski's sign[127]
1st investigation
- serum vitamin B12, methylmalonic acid, homocysteine:
vitamin B12 <148 picomol/L (200 picogram/mL); homocysteine >15 micromol/L; methylmalonic acid >300 micromol/L
Other investigations
- MRI spinal cord:
T2-weighted hyperintensity in the posterior columns of spinal cord
- FBC:
macrocytic anaemia
Mild cognitive impairment
History
memory (or other cognitive) problems or complaints by patient or informant without functional impairment.[12]
Exam
amnestic mild cognitive impairment (MCI): the most common form, memory is the primary problem; MCI in other cognitive domains including language, visuospatial, and frontal executive[12]
1st investigation
Chronic traumatic encephalopathy
History
associated with repetitive mild traumatic brain injury, classically as occurs in boxing, often begins with headache and loss of concentration, followed by fatigue, early amnesia, altered mental status, depression, explosivity, and short-term memory loss
Exam
short-term memory loss, with more serious cognitive impairment in serious cases such as executive dysfunction and difficulty in finding words
1st investigation
- CT brain:
anterior frontal and temporal contusions; corpus callosal and Duret haemorrhages (small areas of bleeding in the ventral and paramedian parts of the upper mid-brain and pons); skull fracture[147][148][149]
More - MRI brain:
cortical atrophy with enlargement of the lateral ventricles and sulci; hippocampal and vermis atrophy; a cavum septum pellucidum; diffuse axonal injury; pituitary gland atrophy; periventricular white matter changes[147][148][149]
More
Uncommon
Frontotemporal dementia
History
profound personality and social conduct changes early in disease (i.e., apathy and disinhibition), decreased empathy, cognitive decline (e.g., disorganisation and poor judgement, changes in eating behaviour such as over-eating or favouring sweets), sometimes associated with amyotrophic lateral sclerosis[95][96]
Exam
frontal executive function deficits (early in disease), frontal release signs (e.g., grasp, palmomentalis, rooting), poor comportment, patients have little insight into their personality changes
1st investigation
- MRI brain:
atrophy of frontal and anterior temporal structures
Other investigations
- brain fluorodeoxyglucose (FDG)-PET scan:
bifrontal (cingulate, orbitofrontal, and dorsolateral prefrontal cortices) and temporal hypometabolism
More - genetic testing:
mutations in progranulin, microtubule-associated protein tau, C9ORF72 (expansion of a non-coding GGGGCC hexanucleotide repeat in the gene C9ORF72 in frontotemporal dementia/amyotrophic lateral sclerosis patients), the valosin-containing protein, multivesicular body protein 2B (CHMB2), transactive response-DNA binding protein, or fused in sarcoma genes
More
Semantic dementia
History
word-finding difficulty, word or object comprehension loss, loss of ability to recognise emotions on faces of others and empathise[98]
Exam
episodic memory preserved in early stages, whereas memory for remote autobiographical events may be lost; fluent anomic aphasia (marked by word-finding difficulties and trouble naming objects, places, and people; word meanings are lost whereas the ability to read, write, and spell these words is retained); impairment in object naming, word-to-picture matching, surface dyslexia, facial recognition, and category fluency[98]
1st investigation
- MRI brain:
asymmetrical atrophy in anterior temporal lobe (either left or right)
Other investigations
- neuropsychological testing:
impaired semantic memory, preserved episodic memory until later stages of the disease
Creutzfeldt-Jakob disease (CJD)
History
Exam
1st investigation
- MRI brain:
fluid-attenuated inversion-recovery (FLAIR) hyperintensity and restricted diffusion (on diffusion-weighted imaging [DWI] and apparent diffusion co-efficient [ADC] sequences) in cortex and/or in deep grey nuclei; might be symmetrical or asymmetrical; cortex more commonly involved than deep grey nuclei[102][103]
More - electroencephalogram:
focal or diffuse slowing of background rhythm (early stages); periodic sharp or tri-phasic waves (late stages)
More
Other investigations
- cerebrospinal fluid examination:
grossly normal, except possibly mildly elevated protein
More
Progressive supranuclear palsy
History
Exam
frontal-subcortical dementia (e.g., forgetfulness, bradyphrenia, emotional/personality changes, inability to manipulate acquired knowledge), deficits in spontaneous recall with preserved recognition on memory testing, predominant wide-eyed stare and furrowed brow, hypophonia, atypical parkinsonism (axial greater than appendicular rigidity), expressive aphasia, ophthalmoplegia (impaired downwards gaze), dysarthria[109][110][111][112][113][114]
1st investigation
Other investigations
- neuropsychological testing:
forgetfulness, bradyphrenia, emotional/personality changes, inability to manipulate acquired knowledge, deficits in spontaneous recall with preserved recognition
Corticobasal syndrome
History
significant overlap with progressive supranuclear palsy, asymmetrical problems controlling body movement often starting in one limb and spreading progressively over time in a clockwise or counterclockwise direction, progressive loss of ability to speak (non-fluent aphasia), decreased comprehension with fluent aphasia, depression, apathy and/or anxiety early in the course are common
Exam
frontal-subcortical dementia (e.g., forgetfulness; bradyphrenia; emotional/personality changes such as apathy, depression, and irritability; inability to manipulate acquired knowledge), deficits in spontaneous recall with preserved recognition, problems with episodic/semantic/working memory, ideomotor apraxia, acalculia, incoordination, aphasia, speech apraxia, occasional cortical sensory deficits (e.g., astereognosis, agraphaesthesia, extinction to double simultaneous stimuli), ophthalmoplegia, dysarthria, asymmetrical parkinsonism, myoclonus, limb dystonia, apraxia, mirror movements, alien limb phenomenon[109][111][116][117][118]
1st investigation
Other investigations
- neuropsychological testing:
forgetfulness, bradyphrenia, emotional/personality changes, inability to manipulate acquired knowledge, deficits in spontaneous recall with preserved recognition problems with episodic, semantic, and working memory
Normal pressure hydrocephalus
History
Exam
1st investigation
- MRI/CT brain:
ventricular enlargement not entirely attributable to cerebral atrophy or congenital enlargement (Evans ratio >0.3), may be enlarged Sylvian fissures out of proportion to atrophy in cortical regions
More
Other investigations
HIV dementia
History
Exam
frontal-executive deficits, inattentiveness, aphasia, ataxia, psychomotor slowing, impairment of visual smooth pursuit, tremor, manual dexterity impairment, heightened tendon reflexes, grasp/suck reflexes, positive Babinski's sign[124]
1st investigation
Other investigations
- cerebrospinal fluid (CSF) examination:
elevated CSF proteins; elevated WBC with mild lymphocytosis[124]
- neuropsychological testing:
frontal executive deficits
Neurosyphilis
History
history of prior unprotected sexual activity, may have distant history of genital lesion (chancre) or palmar rash with any of the following neurological presentations: meningitis, secondary vasculitis with stroke, uveitis, iritis, monocular blindness,[127] seizures in secondary syphilis; lower extremity numbness and unsteadiness (tabes dorsalis), psychosis and dementia (general paresis of the insane) in tertiary syphilis
Exam
pupils constrict to accommodation but not light (Argyll Robertson pupils), optic neuritis on fundoscopy examination, stroke-like signs (e.g., focal weakness, numbness), large fibre sensory loss with positive Romberg's sign (due to posterior column degeneration)[127]
1st investigation
- serum rapid plasma reagin (RPR) test:
reactive (positive); titre of >16 indicates active disease and the need for treatment[128]
More - cerebrospinal fluid (CSF) or serum Venereal Disease Research Laboratory (VDRL) test:
turn positive 1-2 weeks after chancre (painless sore) formation, titre of >16 indicates active disease and the need for treatment[128]
More
Other investigations
- CSF or serum fluorescent treponemal antibody absorption (FTA-ABS):
reactive (positive) if antibodies against Treponema pallidum are present
More - serum treponema pallidum particle agglutination assay:
reactive (positive) if antibodies against Treponema pallidum are present
More - CSF examination:
elevated protein; pleocytosis; positive oligoclonal bands; elevated IgG Index (>0.6)
More
Limbic encephalopathy
History
onset of symptoms is days to weeks, forgetfulness, behavioural changes, seizures (fever and altered consciousness in herpes simplex virus [HSV] encephalitis)
Exam
episodic memory loss, extrapyramidal findings, ataxia, myoclonus, global memory impairment, and decreased consciousness in severe cases
1st investigation
- encephalitis (paraneoplastic and non-paraneoplastic) panel serum and/or CSF antibodies:
positive or elevated (e.g., anti-Hu, Ma2, CV2, amphiphysin, Zic4, voltage-gated potassium channel [VGKC]-associated [leucine-rich glioma-inactivated 1 {LGI1}, contactin-associated protein 2 {CASPR2}], N-methyl D-aspartate receptor [NMDAR], alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor [AMPAR], glutamic acid decarboxylase [GAD] and other antibodies)[34][76][130][131]
More - non-paraneoplastic serum antibody panel (VGKC, GAD, thyroperoxidase, thyroglobulin antibodies):
positive or elevated[34][130][131]
More - serum electrolyte level (in VGKC-associated):
sodium <135 mmol/L (135 mEq/L)
More - MRI brain:
normal or might show hyperintensities in medial temporal lobes, white matter, and elsewhere on fluid-attenuated inversion-recovery (FLAIR)/T2 imaging (all limbic encephalopathies);[131][132][133] anti-CV2 often associated with T2/FLAIR hyperintensities in the basal ganglia;[134] hyperintensities in the medial temporal lobes, may be contrast-enhancing, sometimes haemorrhagic, early involvement of white matter, the inferomedial portion of the temporal lobe most commonly affected (HSV encephalitis)
More - CSF examination:
infectious limbic encephalopathy may cause ele elevated CSF proteins, elevated WBC with lymphocyte predominance, normal or mildly decreased glucose values, elevated IgG index and positive oligoclonal bands, positive HSV polymerase chain reaction (PCR) for herpes viruses (HSV-1 and HSV-2); CSF examination in autoimmune antibody-mediated encephalopathy may be normal or show elevated protein, mild pleocytosis, positive oligoclonal bands, and/or elevated IgG Index (>0.6)
More
Other investigations
- electroencephalogram:
generalised slowing with focal sharp waves or epileptiform activity (anti-voltage-gated potassium channel-associated encephalopathy);[133] focal abnormalities (e.g., spike and slow- or periodic sharp-wave patterns over the involved temporal lobes) or diffuse slowing; slowing or periodic lateralised epileptiform discharges in temporal lobes (HSV encephalitis)
More - neuropsychological testing:
episodic and often remote memory loss
Hashimoto's encephalopathy
History
Exam
inattentiveness, ataxia, myoclonus, tremor[32]
1st investigation
- MRI brain:
normal or may show focal to diffuse (or even confluent) hyperintense T2-weighted signal in subcortical and periventricular white matter, and non-specific white matter abnormalities[32]
- cerebrospinal fluid (CSF) examination:
normal or elevated CSF proteins; normal cell count or mild pleocytosis[32]
- anti-thyroid peroxidase (ATPO) antibodies or anti-thyroglobulin (ATG) antibodies:
ATPO antibodies >25 IU/mL; ATG antibodies >20 IU/mL, depending on the laboratory[33]
More
Other investigations
- electroencephalogram:
seizures, spikes, 1 Hz spikes and waves, or slowing
Brain tumour
History
signs of raised intracranial pressure: nausea, vomiting, headache, altered mental status; seizures; gait abnormality; diplopia if sixth cranial nerve palsy present; focal neurological deficits according to tumour location (e.g., motor weakness, sensory loss, ataxia, visual field defects, aphasia, emotional lability, personality change); may be a history of lung, breast, colorectal or kidney cancer, or melanoma
Exam
may have papilloedema and/or sixth cranial nerve palsy; focal neurological deficits according to tumour location
1st investigation
- MRI brain:
area of hypointensity on T1 sequences and hyperintensity on T2 sequences; contrast enhancement with gadolinium injection
More
Other investigations
- CT brain:
area of hypodensity; enhancement with contrast depending on type or grade of the tumour; hyperdensity if calcification or haemorrhage present
More
Transient global amnesia
History
Exam
acute onset of anterograde amnesia lasting on average 4 to 6 hours in the absence of other neurological symptoms, retrograde amnesia extending as far back as weeks or months may be present, initial impairment of verbal recall tests with gradual improvement over serial testing (typically over period of hours)
1st investigation
Other investigations
- neuropsychological testing:
acute onset of episodic memory deficits lasting on average 4 to 6 hours, or retrograde amnesia extending as far back as weeks or months
Wernicke-Korsakoff's syndrome
History
memory loss, confusion, onset of symptoms is within days to weeks, risk factors for thiamine deficiency (e.g., alcoholism, recent bariatric surgery, malnutrition)[137]
Exam
altered mental state and consciousness, peripheral neuropathy, confabulation, ophthalmoplegia (sixth and other cranial nerve palsies), nystagmus, ataxia, coma, problems with gait or coordination[127]
1st investigation
- serum thiamine level:
decreased
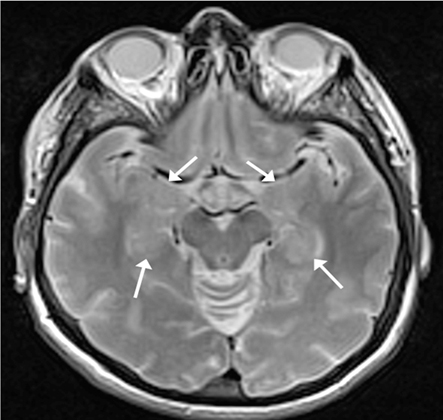
More - MRI brain:
hyper-intensities in the mediodorsal thalamus, fornix, mammillary bodies, periaqueductal regions, and/or superior colliculi on fluid-attenuated inversion-recovery (FLAIR)/T2 imaging; high signal intensities in the thalami and the midbrain tectal plate on DWI sequence;[119] cortical ribboning or gyral hyperintensity with restricted diffusion has also been reported
More
Other investigations
- neuropsychological testing:
confabulation (false memories)
Use of this content is subject to our disclaimer