Aetiology
The exact aetiology for TS remains unknown. However, the features have been repeatedly observed and suggest that TS is the result of bacterial infection:
There are numerous descriptions of TS epidemics including household outbreaks[3]
The disease tends to follow the course of an acute diarrhoeal illness[6]
Coliform bacteria have been isolated at significantly higher rates from the jejunal aspirates of patients with TS compared with controls[7][8][9][10][11]
Antibiotics are an effective treatment for TS.
Less robust evidence suggests that coronaviruses may be involved in the aetiology of TS.[12] Further data suggest that certain HLA sub-types, specifically the Aw-19 series, are associated with TS.[13] It is possible that TS occurs as a result of genetic predisposition triggered by bacterial infection, which then leads to the clinical syndrome. Novel micro-organisms yet to be cultivated may also play a role in the aetiology of TS.[14]
Pathophysiology
TS causes mucosal changes throughout the digestive tract. Marked villous atrophy is evident throughout the small bowel. This results in a decrease in total absorptive surface area. Marked impairment in the absorption of long-chain fatty acids causes steatorrhoea, although the absorption of medium-chain fatty acids is preserved.[15] The altered small-bowel mucosa results in decreased protein absorption and protein loss through the leaky mucosal membrane.[16][17] This increase in small intestinal permeability has been demonstrated using nuclear magnetic resonance spectroscopy of urinary lactulose and mannitol.[18] Villous atrophy also results in a decrease in brush-border disaccharidases, leading to carbohydrate malabsorption.[19]
Folate deficiency, which is a defining feature of the disease, has dual factor aetiology.
There is a loss of the jejunal folate conjugase necessary to deconjugate dietary folate polyglutamates for absorption.[20]
Unabsorbed carbohydrates are metabolised by excess bacteria to form ethanol, which impairs the active transport of low concentrations of folate across the brush-border membrane.[21]
Proximal bowel involvement usually precedes impairment of the distal small bowel and colon. However, the terminal ileum is eventually affected, thus limiting the absorption of vitamin B12 bound to intrinsic factor. It is worth noting that 70% of patients with TS have atrophic gastritis, which points to a possible additional contribution of pernicious anaemia due to impaired production of intrinsic factor.[22]
The impaired terminal ileum results in a decreased re-absorption of bile acids. Diarrhoea associated with TS is thus partially due to a choleretic effect as excess bile acids reach the colon. There is also a direct colopathy in TS resulting in impaired colonic absorption of water and sodium.[23][Figure caption and citation for the preceding image starts]: Tropical sprue; ridged and foveolar patterns, duodenumFrom the collection of Dr M. Guelrud; used with permission [Citation ends].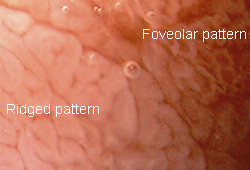 [Figure caption and citation for the preceding image starts]: Endoscopy, normal and tropical sprue (TS) villi changes, duodenumFrom the collection of Dr M. Guelrud; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Endoscopy, normal and tropical sprue (TS) villi changes, duodenumFrom the collection of Dr M. Guelrud; used with permission [Citation ends].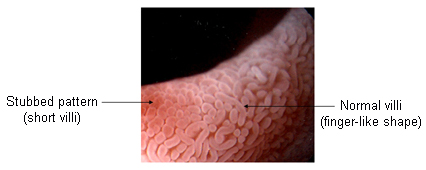 [Figure caption and citation for the preceding image starts]: Normal duodenum, standard endoscopyFrom the collection of Dr M. Guelrud; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Normal duodenum, standard endoscopyFrom the collection of Dr M. Guelrud; used with permission [Citation ends].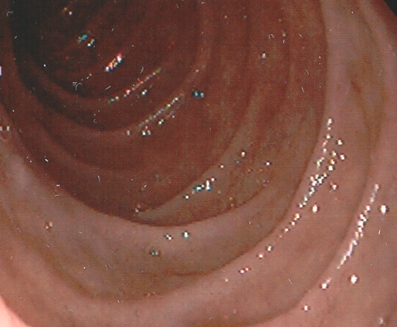 [Figure caption and citation for the preceding image starts]: Tropical sprue; scalloping, mosaic appearance, and mucosal grooves; duodenumFrom the collection of Dr M. Guelrud; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Tropical sprue; scalloping, mosaic appearance, and mucosal grooves; duodenumFrom the collection of Dr M. Guelrud; used with permission [Citation ends].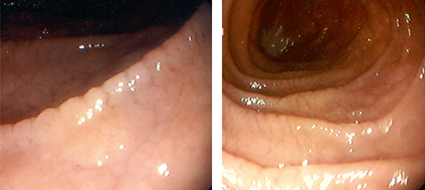
Use of this content is subject to our disclaimer