Approach
Treatment should be based on the specific pathophysiological cause of nausea and vomiting. Causes are numerous and varied, and so a thorough history and physical examination is essential to aid diagnosis. For some patients, the cause of nausea and vomiting cannot be defined, and empirical treatment is then necessary.
In general, the physician needs to determine whether the nausea and vomiting is acute or chronic and whether the cause of nausea and vomiting is related to gastrointestinal or non-gastrointestinal causes.
Acute nausea and vomiting is sudden in onset and has a duration of 1 to 3 days. Volume depletion and electrolyte abnormalities are the initial adverse consequences that must be addressed. Rapidly reversible causes include mechanical obstructions of the gastrointestinal tract, infections of the central nervous system (CNS), and stroke.
Although causes of acute symptoms are the same as for chronic nausea and vomiting, the more common causes of chronic symptoms are gastric neuromuscular dysfunctions, (including gastric electrical and mechanical disorders, resulting in severe functional dyspepsia), unexplained nausea and vomiting, gastroparesis-like syndrome, and gastroparesis. Specific medication and dietary approaches are used to treat chronic disorders.
Non-gastrointestinal causes include CNS disorders such as migraine headache, stroke, and meningitis, and can often be excluded by history and examination. Metabolic and endocrine disorders, especially Addison's disease, should be considered.
History
A detailed history of the presenting symptoms and any previous medical and surgical history can narrow the differential diagnosis and aid in the interpretation of key examination findings. The primary purpose of the initial encounter is to evaluate whether the patient requires immediate surgical evaluation or if the symptoms suggest a serious underlying condition.
Quality, timing (including the pattern of cyclic or non-cyclic symptoms), and the radiation of any associated pain
Cramping pain that precedes the onset of nausea and vomiting may be due to gastrointestinal tract obstruction.
Obstruction may be of the gastrointestinal tract lumen or the cystic duct, common bile duct, or pancreatic duct due to adhesions, strictures, stones, or tumours.
Gastric or duodenal ulcers classically are associated with an achy or crampy epigastric or right upper quadrant pain.
Flank pain and dysuria suggest renal stones.
Treatment of obstructions of the gastrointestinal tract is often definitive, whether by surgery, stent, balloon dilation, or sphincterotomy, and results in rapid relief of symptoms.
Characteristics of the vomiting
Vomiting of gastric juices suggests gastric outlet obstruction.
Vomiting of bilious material suggests small bowel obstruction.
Vomiting of feculent material suggests colo-intestinal or colo-gastric fistulae.
Symptom-free week(s) followed by days of extremely severe nausea and vomiting suggests cyclic vomiting syndrome (CVS).[29][30]
The Rome IV criteria for CVS in adults stipulate:[30][31]
Episodes of acute-onset vomiting lasting <7 days.
Episodes of acute-onset vomiting should be separated by at least 1 week of baseline health.
Symptoms in relation to meals
Symptoms that are worse after ingestion of food may relate to gastric dysrhythmias such as tachygastria, bradygastria, or gastroparesis.
Patients with idiopathic nausea and vomiting or "functional" dyspepsia often have a history of nausea that is worse after eating, with or without vomiting of undigested or chewed food. Other symptoms are early satiety and epigastric fullness.
Patients with eating disorders such as bulimia rarely present themselves to the gastroenterologist or physician seeking a diagnosis and treatment for these symptoms.
Presence of anorexia or weight loss
Anorexia may be a symptom of extensive liver metastases associated with nausea.
Ovarian cancers should be considered in middle-aged women who report vague abdominal discomfort, loss of appetite, and early satiety.[26][27]
Renal cell carcinoma is also nauseogenic, and small cell cancers of the lungs are associated with paraneoplastic syndromes that include gastroparesis, nausea, and vomiting. Infiltrating adenocarcinomas of the stomach may result in linitis plastica (morphological variant of diffuse or infiltrating stomach cancer) and symptoms of early satiety, fullness, nausea, and vomiting.
Anorexia nervosa presents with nausea, anorexia, and weight loss.
Presence of diarrhoea
Acute and chronic viral and bacterial gastroenteritis present with vomiting and diarrhoea with or without nausea.
Food poisoning presents with vomiting and diarrhoea within several hours to days following consumption of contaminated food.[32]
Neurological symptoms
Patients with migraine have recurrent nausea, with or without vomiting, associated with headache and blurred vision.
Unexplained recent headaches, change in vision or motor function, and disturbances of balance may point toward a serious diagnosis of a tumour or stroke.
Patients with complex partial seizures have more subtle symptoms characterised by the sensation of a bizarre smell, the appearance of being in a daydream, or staring blankly.
A patient with meningitis may have a high-grade fever, rash, and photophobia. Those with a cerebral abscess may have focal deficits.
Vertigo and balance disorders may suggest vestibular nerve lesions such as an acoustic neuroma, or there may be a history characteristic of motion sickness.
Current medicine/drug history
Drug classes associated with a high incidence of nausea include non-steroidal anti-inflammatory drugs, antidepressants, opioids, anti-arrhythmics, chemotherapy, and oestrogen and progesterone agents. Specific drugs include digoxin, theophylline, lubiprostone, metformin, and exenatide. Careful review of the patient medicine list may reveal drugs as the chief source of nausea and vomiting.
Cannabinoid hyperemesis has been described mainly in younger adults who are chronic users.[16] In one case series, all patients were younger than 50 years of age. Most had used cannabis for more than 2 years and at a frequency of more than once per week. Abdominal pain, as well as nausea/vomiting, is common. Patients report relief with hot showers or baths (suggesting autonomic nervous system [ANS] arousal).[17][18]
Previous history of surgeries
History of previous abdominal surgeries is a predisposing risk for acute small bowel obstruction.
Small bowel obstruction has been reported in up to 5% of patients undergoing laparoscopic Roux-en-Y gastric bypass.[33]
Fundoplication (possibly with inadvertent vagal nerve damage), fundic and distal oesophageal resections for oesophageal cancer, antrectomy and vagotomy for peptic ulcer or cancer (Bilroth I and Bilroth II, Roux-en-Y) are associated with resultant gastric dysrhythmias and gastric emptying abnormalities.
Previous medical history
There may be symptoms of hypothyroidism such as fatigue and cold intolerance, or dyspepsia symptoms.
Hyperthyroidism may be suspected if there is heat intolerance, nausea, and weight loss.
Adrenal insufficiency presents with chronic nausea and vomiting, absent abdominal pain, and diarrhoea. It is a life-threatening disorder that requires urgent consideration.
Patients with ischaemic gastroparesis may have a history of other atherosclerotic diseases such as coronary artery disease, carotid atherosclerosis, or intermittent claudication. These patients do not have severe abdominal pain, unless the arterial occlusions advance to total obstruction, at which time typical severe abdominal angina with impending small bowel infarction occurs. Some patients will have progressive weight loss and non-specific, diffuse abdominal tenderness.
Pseudo-obstruction can occur in patients with scleroderma or amyloidosis.
Irritable bowel syndrome presenting with constipation or simple, severe constipation is associated with nausea as a result of pseudo-obstruction.
Nausea that is more pronounced with a change in position (e.g., supine to upright) may indicate postural orthostatic tachycardia syndrome (POTS). Patients with POTS also often report lightheadedness with a change in position.
Female patients
The date of the last menstrual period, contraception used, and current pregnancy status should be checked.
Nausea and vomiting ranges from mild to severe in nausea of pregnancy, a disorder that occurs in 80% of women during the first trimester of pregnancy.[34][35] It is imperative to rule out pregnancy as a cause in women of child-bearing age.
Physical examination
Important aspects of the physical examination should include the following.
Measurement of vital signs/general examination
Patients should be assessed for volume depletion and adequate peripheral perfusion.
Patients with anorexia nervosa or advanced malignancies may be profoundly underweight and undernourished.
Loss of dental enamel because of frequent vomiting or regurgitation may be present in people with eating disorders.
Comprehensive abdominal examination
Presence of healed abdominal incisions suggests previous surgical procedures. Assessment for an abdominal wall syndrome by eliciting tender areas for a positive Carnett's sign is indicated. A positive Carnett's sign occurs when a combination of pressure on the scar and flexion of the head clearly exacerbates the patient's typical pain, indicating that the pain originates in the abdominal wall, often the rectus muscle sheaths.[19]
Patients may be lying still if they have peritonitis. A rigid abdomen is a distinguishing sign for an acute abdomen. Rebound tenderness and guarding may be present in bowel perforation.
Abdomen may be distended and tympanitic with high-pitched bowel sounds and pain located in the epigastrium, periumbilical area, or lower abdominal quadrants in gastrointestinal obstruction.
Epigastric tenderness is often elicited by palpation in small bowel inflammation due to coeliac disease or eosinophilic enteritis, gastric neuromuscular disorders, or violent retching.
Palpation may reveal an abdominal mass suggestive of a carcinoma that may require further investigations.
If percussion induces pain, there may be peritoneal inflammation. Percussion is also used to detect the presence of shifting dullness in the presence of ascites.
Hyperactive bowel sounds that diminish with time are heard in small bowel obstruction. Absent bowel sounds indicate pseudo-obstruction, especially when there is a distended abdomen that is tympanitic and tender to palpation.
An abdominal bruit may indicate ischaemic gastroparesis and is found in approximately half of these patients. Some patients with ischaemic gastroparesis have progressive weight loss and non-specific, diffuse abdominal tenderness.
Signs of heat damage to cutaneous abdominal skin, which may indicate prolonged use of heat pad.
If examination is equivocal, distracting the patient can be useful.
Pelvic examination is indicated for most women if there is pain in the lower abdomen.
An ovarian mass may indicate an ovarian tumour.
Confirmation or exclusion of pregnancy is necessary.
Endocrine assessment
The patient is assessed for signs of hypothyroidism such as hair loss, dry skin, delayed reflexes, and presence of goitre.
Eye signs and a goitre with tremors may be present in patients with hyperthyroidism who also appear anxious and distressed.
The endocrine examination may be entirely normal in patients with adrenal insufficiency or diabetes. Patients with diabetes may have peripheral neuropathy or orthostatic hypotension. Patients with adrenal insufficiency may have orthostatic hypotension, hyperpigmentation, or calcified pinnae.[36][37]
Neurological assessment
Neurological examination may be normal if nausea and vomiting are due to a neurological cause. However, autonomic nervous system assessments may reveal abnormalities.
Examination may reveal features of Parkinson's disease (e.g., shuffling gait, pill-rolling tremor, cog-wheel rigidity), nystagmus, postural instability, or neurological deficits related to strokes or seizures.
Patients with meningitis may have neck stiffness, and those with a brain abscess may demonstrate focal neurological deficits.
Subtle sub-clinical neurological signs may be elicited in patients with meningeal irritation due to fungal infections, with meningeal lymphoma, and in complex partial seizures.
Per rectal examination
Performed in the presence of occult or frank blood in stools. May indicate mucosal inflammation or gastrointestinal malignancies.
Laboratory investigations
Appropriate investigations should be tailored to history and examination findings, and be made on a case-by-case basis.
White blood cell count ranges from normal to elevated in inflammatory disorders.
Electrolyte abnormalities such as hyponatraemia and hypokalaemia may occur in volume depletion. Hyperkalaemia is suggestive of adrenal insufficiency. Variable electrolyte abnormalities are observed in patients with eating disorders.
Erythrocyte sedimentation rate is elevated in peritonitis and abdominal abscess, and in most chronic inflammatory disorders.
When investigating peptic ulcer disease or gastritis, Helicobacter pyloriurea breath testing may be indicated.
Stool culture may help to identify the offending organism in cases of acute gastroenteritis or food poisoning.
If infection of the central nervous system is suspected (e.g., headache, fever, photophobia, rash, neck stiffness) a lumbar puncture should be performed.
Diagnostic lumbar puncture in adults: animated demonstrationHow to perform a diagnostic lumbar puncture in adults. Includes a discussion of patient positioning, choice of needle, and measurement of opening and closing pressure.
Endocrine investigations:
fasting plasma glucose and HbA1c are elevated in patients with diabetes mellitus
thyroid-stimulating hormone and thyroid hormone levels are indicated in patients with suspected hypothyroidism or hyperthyroidism
fasting cortisol is generally low in adrenal insufficiency; acute or chronic adrenal insufficiency is investigated with a cosyntropin (adrenocorticotropic hormone) stimulation test
in the setting of hypercalcaemia, parathyroid hormone level aids in the diagnosis (high in hyperparathyroidism, suppressed in other diagnoses such as malignancy).
Urine or blood pregnancy test is indicated to rule out pregnancy.
24-hour urine creatinine clearance is necessary to calculate glomerular filtration rate (GFR) in patients with uraemia. [ Glomerular Filtration Rate Estimate by the IDMS-Traceable MDRD Study Equation Opens in new window ] Alternatively, the estimated GFR (eGFR) can be determined.[38] Renal profile may reveal hyperkalaemia, acidosis, hypocalcaemia, and hyperphosphataemia.
Positive antinuclear antibodies level is suggestive of secondary pseudo-obstruction due to a vasculitic disorder.
Common radiological/endoscopic investigations
Abdominal x-ray series
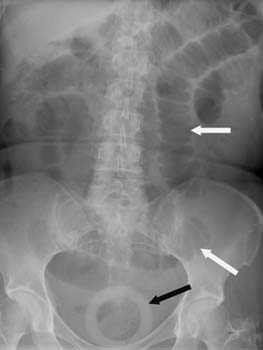
Confirms air fluid levels and the point of obstruction in patients with mechanical obstructions.
Shows distended loops of small bowel, colon, or gastric distension in pseudo-obstruction, irritable bowel syndrome, and severe constipation.[Figure caption and citation for the preceding image starts]: Plain abdominal x-ray showing dilated centrally placed bowel loops with valvulae conniventes (white arrows). No dilated large bowel segments can be seen, representing small bowel obstruction. The black arrow shows an incidental ring pessaryGrant L, Hampson FA, Shaw AS. Student BMJ. 2009;17:114-116; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Large bowel obstruction as seen on x-rayBickle I, Kelly B. Student BMJ. 2002;5:140; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Large bowel obstruction as seen on x-rayBickle I, Kelly B. Student BMJ. 2002;5:140; used with permission [Citation ends].
Chest x-ray
A standard posteroanterior and lateral chest x-ray is an inexpensive and simple initial step to evaluate any cough, chest pain, and/or haemoptysis (suggestive of lung cancer).
Upper gastrointestinal barium studies
Shows mucosal irregularities consistent with mucosal ulceration. Barium studies are generally done by non-gastroenterologists if, for example, there is limited access to endoscopy.
Ultrasound abdomen, kidneys, or pelvis
May aid in the diagnosis of bile duct or cystic duct obstruction (ultrasound gallbladder, pancreas, liver), uraemia (ultrasound kidneys for size), ovarian cancer (ultrasound pelvis), renal cancer (ultrasound abdomen/pelvis), and pregnancy (ultrasound pelvis).
Computed tomography (CT) abdomen
May reveal the source and site of obstructive anatomy in mechanical obstructions and the absence of localised obstruction in pseudo-obstruction.
Reveals peritoneal diseases or fluid collections in patients with peritonitis and malignancies.
Reveals thickened gastric wall, masses on the kidneys or the ovaries, and liver metastases, and leads to specific diagnosis of carcinomas.
Upper gastrointestinal endoscopy
Reveals pyloric or duodenal obstructions and their causes (e.g., ulcers or cancers).
Most specific diagnostic test for mucosal inflammation of oesophagus, stomach, and duodenum.
Can rule out mucosal inflammation and sub-total stenosis of an anastomosis of previous operations.
Measurements of pyloric compliance
Can be done with a functional luminal imaging probe (FLIP), especially of the pylorus, but also of the oesophagus, looking for dysfunction of these sphincters.[39]
Spasm, if quantified and found to be abnormal, can sometimes be treated with injections of botulinum toxin.
Further investigations
Gastric electrical activity
Records gastric electrical activity and confirms the presence of objective neuromuscular dysfunction in patients with previous gastric operations, if diagnosis in doubt.
Can be performed with a single-point first-generation device, a several-electrode second-generation device, or a multi-electrode third-generation device. Some devices measure not only gastric electrical frequency, but also amplitude and propagation of signals, often associated with recording of symptoms. This helps to map the stomach more akin to invasive studies.[40]
Gastric electrical dysfunctions are common in patients with gastric neuromuscular disorders; many of them will have documented gastroparesis.
Some patients with gastric neuromuscular disorders have abnormalities of gastric relaxation or gastric visceral hypersensitivity.
Gastric emptying study (scintigraphy)
Considered the definitive test for the diagnosis of gastroparesis. The test is non-invasive and can assess for solid and liquid emptying.[41][42]
Gastric retention >60% after 2 hours or >10% after 4 hours after consumption of the meal is considered to be delayed gastric emptying.[43]
Colonoscopy
May aid in the diagnosis of colonic obstruction.
Motility studies
Reveal gastroparesis, small bowel neuromuscular dysfunction, and/or colonic inertia in gastrointestinal pseudo-obstruction, irritable bowel syndrome, constipation.
CT head
Aids in the diagnosis of intracranial lesions or stroke.
Electroencephalogram
Indicated in patients presenting with complex partial seizure.
Audiometry and electronystagmography
Should be performed when suspecting vestibular nerve lesions (e.g., dizziness, vertigo, decreased hearing, difficulties with balance).
CT chest
May reveal a mass in the lung in cases of suspected lung cancer (e.g., history of smoking, weight loss, shortness of breath, cough).
Abdominal paracentesis with biopsy
Histology of aspirated abdominal fluid and biopsied mass or peritoneum confirms diagnosis of carcinomatous peritonitis.
Mesenteric duplex ultrasound examination and CT angiogram
Mesenteric duplex ultrasound examination confirms blood flow disturbance in the superior mesenteric artery or coeliac artery in patients with suspected chronic mesenteric ischaemia (e.g., diffuse abdominal tenderness, abdominal bruit), while CT angiogram identifies site of blood vessel stenosis in these patients.[12]
ANS tests
ANS testing can be done directly with sympathetic and parasympathetic measures, or indirectly with heart rate variability (HRV). It can include postural manoeuvres and/or be combined with tilt table testing.
In patients with an orthostatic component to the onset of nausea, a tilt table test should be ordered. Blood pressure and/or pulse rate do not increase in response to upright tilt and nausea is provoked during the test.
Non-digestible capsule test
An alternative first test for the diagnosis of gastroparesis, if available.[7] Diagnosis is confirmed if the capsule (brand name: SmartPill) is not emptied within 5 hours of ingestion. The capsule wirelessly transmits data about the gastrointestinal tract to a recording device.
Use of this content is subject to our disclaimer
