Mycoplasma pneumoniae is mainly a mucosal pathogen, but during disease it may have a systemic spread.[4]Waites KB, Talkington DF. Mycoplasma pneumoniae and its role as a human pathogen. Clin Microbiol Rev. 2004 Oct;17(4):697-728.
https://www.doi.org/10.1128/CMR.17.4.697-728.2004
http://www.ncbi.nlm.nih.gov/pubmed/15489344?tool=bestpractice.com
[18]Johnson SM, Bruckner F, Collins D. Distribution of Mycoplasma pneumoniae and Mycoplasma salivarium in the synovial fluid of arthritis patients. J Clin Microbiol. 2007;45:953-7.
http://jcm.asm.org/content/45/3/953.full
http://www.ncbi.nlm.nih.gov/pubmed/17122006?tool=bestpractice.com
[19]Daxboeck F, Khanakah G, Bauer C, et al. Detection of Mycoplasma pneumoniae in serum specimens from patients with Mycoplasma pneumonia by PCR. Int J Med Microbiol. 2005;295:279-85.
http://www.ncbi.nlm.nih.gov/pubmed/16128402?tool=bestpractice.com
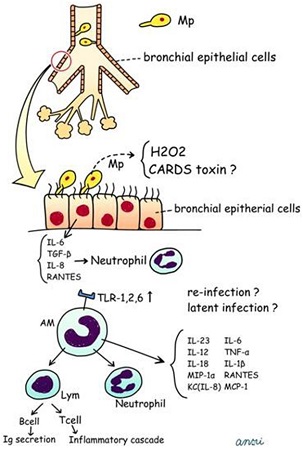
M pneumoniae disease is initiated by its attachment to the respiratory epithelium via a unique tip organelle. This organelle contains P1 adhesin and facilitates adherence and gliding motility. Following cytoadherence in the respiratory tract, M pneumoniae induces localised tissue disruption and cytotoxicity through production of hydrogen peroxide and other free radicals. The subsequent immune response, mediated by macrophages and lymphocytes, exacerbates clinical illness and contributes to pulmonary injury. Damage to epithelial cilia is associated with severe and persistent cough.[4]Waites KB, Talkington DF. Mycoplasma pneumoniae and its role as a human pathogen. Clin Microbiol Rev. 2004 Oct;17(4):697-728.
https://www.doi.org/10.1128/CMR.17.4.697-728.2004
http://www.ncbi.nlm.nih.gov/pubmed/15489344?tool=bestpractice.com
[20]Saraya T, Kurai D, Nakagaki K, et al. Novel aspects on the pathogenesis of Mycoplasma pneumoniae pneumonia and therapeutic implications. Front Microbiol. 2014;5:410.
https://www.doi.org/10.3389/fmicb.2014.00410
http://www.ncbi.nlm.nih.gov/pubmed/25157244?tool=bestpractice.com
M pneumoniae may have an intracellular lifestyle enabling it to escape from the immune system.[21]Katz B, Waites K. Emerging intracellular bacterial infections. Clin Lab Med. 2004;24:627-49.
http://www.ncbi.nlm.nih.gov/pubmed/15325059?tool=bestpractice.com
It may produce toxins that cause persistent cough, and the immunological response to M pneumoniae, particularly the release of pro-inflammatory cytokines, rarely also promotes acute exacerbations of asthma.[4]Waites KB, Talkington DF. Mycoplasma pneumoniae and its role as a human pathogen. Clin Microbiol Rev. 2004 Oct;17(4):697-728.
https://www.doi.org/10.1128/CMR.17.4.697-728.2004
http://www.ncbi.nlm.nih.gov/pubmed/15489344?tool=bestpractice.com
[20]Saraya T, Kurai D, Nakagaki K, et al. Novel aspects on the pathogenesis of Mycoplasma pneumoniae pneumonia and therapeutic implications. Front Microbiol. 2014;5:410.
https://www.doi.org/10.3389/fmicb.2014.00410
http://www.ncbi.nlm.nih.gov/pubmed/25157244?tool=bestpractice.com
[22]Johnston SL, Martin RJ. Chlamydophila pneumoniae and Mycoplasma pneumoniae: a role in asthma pathogenesis? Am J Respir Crit Care Med. 2005 Nov 1;172(9):1078-89.
http://www.ncbi.nlm.nih.gov/pubmed/15961690?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Proposed pathophysiologic cascade of Mycoplasma pneumoniae pneumonia in humansSaraya T, Kurai D, Nakagaki K, et al. Novel aspects on the pathogenesis of Mycoplasma pneumoniae pneumonia and therapeutic implications. Front Microbiol. 2014;5:410. (CC BY 2.0). [Citation ends].