Approach
Although most people with acute tonsillitis do not seek medical help, acute tonsillitis is one of the most common reasons for seeking medical advice.
It is usually seen in people between the ages of 5 and 15 years, and it occurs most commonly in the winter and early spring in temperate climates.[1][4][5]
Patients may have a history of contact with infected people, particularly in institutions or enclosed spaces (e.g., child care centres, schools, prison).
Clinical diagnosis
In the vast majority of patients, tonsillitis is a benign, self-limiting condition that requires only symptomatic treatment and no investigations. In these patients, the diagnosis is clinical. However, it is important to establish that the patient has tonsillitis and not another, potentially dangerous, cause of sore throat (such as retropharyngeal abscess, acute epiglottitis, HIV, or infectious mononucleosis); these conditions should be excluded on the basis of history and physical examination.
As part of the clinical diagnosis, decide if the patient's overall condition or any comorbidity warrants further testing for the causes of sore throat.
Patients with acute streptococcal tonsillitis will often report a sudden onset of sore throat and have pain on swallowing. The sore throat is typically accompanied by fever (>38°C [>100.5°F]), and patients may have headache, abdominal pain, nausea, and vomiting. The absence of a cough or runny nose makes a bacterial rather than a viral infection more likely.
Examination of the throat may show tonsillar exudate and enlargement and erythema of the tonsils. There may be anterior cervical lymphadenopathy.[Figure caption and citation for the preceding image starts]: Tonsillitis caused by group A beta-haemolytic streptococcusFrom the collection of Dr Eleftherios Margaritis [Citation ends].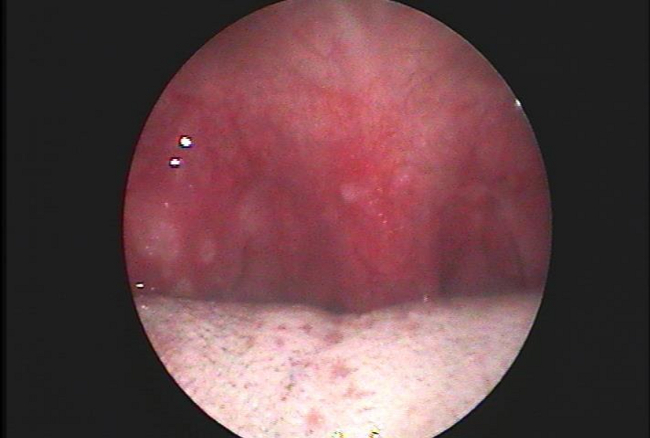
Clinical differentiation between streptococcal and other aetiology
Most patients with acute tonsillitis have a viral infection; however, beta-haemolytic streptococcal infection makes up between 5% to 15% of cases of pharyngitis in adults and 15% to 30% of cases in children.[1][2]
Individual signs and symptoms cannot be used to discriminate group A beta-haemolytic streptococci (GABHS) tonsillitis from other types of sore throat. There is not any powerful enough clinical prediction rule to definitely diagnose or rule out streptococcal pharyngitis in children. However, a Centor score ≥3 is a well-calibrated clinical prediction rule for suggesting a high probability of a patient >14 years old with acute tonsillitis having a GABHS infection.[11][12]
The Centor criteria that give a +1 score are:[12]
History of fever over 38°C (100.5°F)
Tonsillar exudate
Absence of cough
Tender anterior cervical lymphadenopathy.
If 3 or 4 of the Centor criteria are met, the positive predictive value is around 40% to 60%. The absence of 3 or 4 of the Centor criteria has a fairly high negative predictive value over 80%, and it is highly unlikely that a patient with fewer than 2 criteria will have GABHS tonsillitis.[13]
Because testing of all patients with sore throat is not practicable, it makes sense to confine microbiological testing for GABHS to patients with a high probability of GABHS: that is, patients with 3 or 4 Centor criteria.
The McIsaac score is a similar scoring system for sore throat that also incorporates age and season and can be used in anyone aged 3 years and over.[14] [ Sore Throat (Pharyngitis) Evaluation and Treatment Criteria (McIsaac) Opens in new window ]
The streptococcal score card gives an indication of the likelihood of a sore throat in children being due to infection with GABHS.[5] The criteria are:[5]
Age 5 to 15 years
Season (late autumn, winter, early spring)
Fever (≥38.3°C [≥101°F])
Cervical lymphadenopathy
Pharyngeal erythema, oedema, or exudate
No symptoms of a viral upper respiratory infection (conjunctivitis, rhinorrhoea, or cough).
If 5 of the criteria are met, a positive culture for GABHS is predicted in 59% of children; if 6 of the criteria are met, a positive culture is predicted in 75% of children.[5]
Diagnostic tests
In the rare instance when the diagnosis of GABHS infection needs to be made with certainty (i.e., in vulnerable patients or populations, such as those at high risk of rheumatic fever [e.g., from indigenous communities, developing countries]), GABHS infection can be diagnosed in adults by rapid streptococcal antigen testing and in children by rapid streptococcal antigen testing in conjunction with throat cultures.[2][15] Serological testing for streptococci may be useful in suspected rheumatic fever.
A full blood count may be helpful in patients with suspected infectious mononucleosis, in immunocompromised patients, and in patients with signs or symptoms of severe infection or sepsis. A raised white blood cell (WBC) count with neutrophilia is suggestive of a bacterial infection, whereas a raised WBC count with lymphocytosis and atypical lymphocytes is suggestive of infectious mononucleosis.[16][17]
Testing for reactive heterophile antibodies is also useful to rule out infectious mononucleosis and is indicated for patients with symptoms that persist, as well as for those with posterior (or anterior) cervical lymphadenopathy.
Vaginal and cervical, or penile, and rectal cultures should be performed if there is reason to suspect a gonococcal throat infection, especially in sexually active adolescents, in particular those engaging in oral-genital sex.
An HIV viral load assay is indicated for patients at risk of HIV infection who have persistent tonsillitis accompanied by severe constitutional symptoms (e.g., malaise, tiredness, weight loss, generalised lymphadenopathy).
A lateral cervical view x-ray, exposed for soft tissue, should be performed in patients who do not respond to treatment, in those who present with severe symptoms and/or significant trismus (lockjaw), and in those with neck swelling.
Use of this content is subject to our disclaimer