Approach
The diagnosis of CRPS is clinical. The diagnosis is usually straightforward if all diagnostic criteria are met at examination.[36] However, symptoms and signs can change with time, even in the course of a day, and sometimes in response to ambient temperatures and stress. Frequently, not all symptoms or signs are present at the same time, leading to confusion in the diagnosis, especially if providers are unfamiliar with the presentation of CRPS.
History
There is usually a history of an initiating noxious event to the affected part, such as a fracture, sprain, or surgical procedure. The pain usually begins immediately or within a few days or weeks, and is often described as burning, lancinating, sharp, shooting, or aching. CRPS affects the extremities; the upper limb is more frequently affected than the lower limb.[4][5]
Pain is not confined to a specific dermatomal distribution and may spread contiguously, to involve the entire limb. The pain may spread to the other ipsilateral limb (e.g., from left arm to left leg) or to the same limb contralaterally (e.g., left arm to right arm); diagonal contralateral spread (e.g., right arm and left leg involvement) is relatively rare (approximately 17%).[33] Most significant is that pain persists past the healing phase of injury and is out of proportion to the severity of the initiating event. It is spontaneous and continuous, and is often worsened by minor stimuli: for example, clothing and movement. Stimulus-evoked pain, such as allodynia (the appreciation of pain to a non-noxious stimulus such as a brush or cold) or hyperalgesia (the appreciation of a pain out of proportion to a noxious stimulus such as a pin), occurs in almost all patients at some point in their clinical course and is most pronounced distally. Patients may report a difference in skin temperature, sweating changes, or oedema. Abnormal posturing, tremors, and weakness are also common complaints. Body scheme changes (body perception disturbance) are becoming increasingly recognised as part of the clinical presentation of CRPS. Slowed and inaccurate finger perception is common and when combined with abnormal body perception is accurate in predicting persistent pain post-trauma.[37][38]
A constellation of symptoms is required for a diagnosis of CRPS, as outlined by the International Association for the Study of Pain, which has adopted the Budapest diagnostic criteria for CRPS. These criteria state that at least one symptom must be present from three of four categories: sensory, motor, sudomotor, and vasomotor.[1][2][3][36] See Diagnostic criteria.
Examination
Sudomotor and vasomotor abnormalities may be apparent, such as a difference in temperature between affected and surrounding areas or when compared with the opposite limb. Skin colour may change. Warm skin with erythema is most frequently seen in the early stages; later, the limb often appears bluish and cold. Uncommonly, bullae may form over the affected skin area and there may be an absence or excess of local hair growth. Trophic changes of the skin and nails are common.
Allodynia and hyperalgesia can often be demonstrated, and sensory deficits (hypoaesthesia) may occur in the same distribution or in a non-dermatomal glove or stocking distribution in the distal limb.
Motor abnormalities are common, especially in severe cases. Many patients hold the affected limb immobile with the potential to develop contractures. Dystonic posturing of the limb, tremor, and myoclonic jerks can be seen. Reflexes are often hyperreflexic.[Figure caption and citation for the preceding image starts]: Atrophic skin and loss of hair; ulcer on right footReprinted with permission from the Reflex Sympathetic Dystrophy Syndrome Association [Citation ends]. [Figure caption and citation for the preceding image starts]: Brawny oedema with reddened and thickened skin, increased nail growth of great toe, and deep ulcerated lesion at top of footReprinted with permission from the Reflex Sympathetic Dystrophy Syndrome Association [Citation ends].
[Figure caption and citation for the preceding image starts]: Brawny oedema with reddened and thickened skin, increased nail growth of great toe, and deep ulcerated lesion at top of footReprinted with permission from the Reflex Sympathetic Dystrophy Syndrome Association [Citation ends]. [Figure caption and citation for the preceding image starts]: Skin shedding from arm and upper bodyReprinted with permission from the Reflex Sympathetic Dystrophy Syndrome Association [Citation ends].
[Figure caption and citation for the preceding image starts]: Skin shedding from arm and upper bodyReprinted with permission from the Reflex Sympathetic Dystrophy Syndrome Association [Citation ends].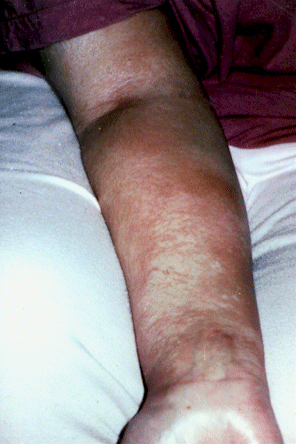
According to the Budapest diagnostic criteria, at least one sign must be present at the time of evaluation in two or more of the following categories: sensory, motor, sudomotor, and vasomotor.[1][2][3] See Diagnostic criteria.
Investigations
CRPS is principally a clinical diagnosis; diagnostic tests are not required.[36] Investigations that may rule out other differentials, or support the diagnosis, include the following.
Electromyogram and nerve conduction studies
To exclude a generalised or focal peripheral neuropathy affecting large myelinated fibres. Nerve conduction studies test only the large (fast-conducting) myelinated A alpha/beta fibres in mixed peripheral nerves.
These investigations do not test small A delta and C fibres, those primarily affected in CRPS.
Punch skin biopsy
May reveal defects in the small axonal fibres.
Abnormalities are common in small-fibre neuropathies and inheritable neuropathies, and are seen in CRPS patients, but they are not specific for CRPS.[39]
Bone studies
Radiography, bone scintigraphy, or bone densitometry of the affected limb (compared with the unaffected limb) may be utilised. Bone scintigraphy can detect a variety of disorders, and triple-phase bone scintigraphy may detect alterations in bone metabolism for patients with CRPS who have bone resorption as part of their presentation.[40] Bone densitometry or radiography may show evidence of osteoporosis in the affected limb compared with the contralateral limb. Positive or negative findings do not rule in/out the diagnosis of CRPS, but can be helpful as diagnostic measures in atypical presentations or for consideration of bisphosphonate therapy.[41]
Dual-energy x-ray absorptiometry (DXA), quantitative CT, or ultrasound may reveal regional osteopenia in the trabeculated bone, with the cortical bone usually preserved.[40][42][43][44] Osteoporosis may be evident in chronic cases. Bone scanning may detect changes earlier, and bone densitometry measurements will improve in response to treatment.
Magnetic resonance imaging
To identify soft-tissue and occult bone injuries, including bone oedema syndromes and stress fractures.[45]
Normal scan does not exclude CRPS.
Vascular studies
To rule out arterial compression, or venous thrombosis or incompetence.
Therapeutic trials of sympathetic nerve blocks and regional or selective nerve blocks
There is limited evidence for these, despite being a common practice in CRPS.[46][47]
If sympathetic nerve blocks are successful, the patient may have a degree of sympathetically mediated pain. However, lack of response does not exclude the diagnosis, as pain associated with CRPS can be sympathetically independent.
If regional or selective nerve blocks are successful, the target may represent a peripheral target that is contributing to the presentation and perhaps resulting in a degree of central nervous system plasticity. This may offer an option for targeted treatment in appropriate circumstances. However, lack of response or otherwise does not change the diagnosis of CRPS, which is made based on signs and symptoms as described in the Budapest Criteria.[1][3]
Use of this content is subject to our disclaimer