Aetiology
The aetiology of blepharitis is typically determined by its location, being grouped into anterior or posterior blepharitis.[1] There is overlap, and both anterior and posterior blepharitis may be present.
Anterior blepharitis is thought to be caused by pathogenic bacteria on the eyelids, with Staphylococcus epidermidis (95.8%), Propionibacterium acnes (92.8%), and Corynebacterium species (76.8%) frequently isolated.[11][12]Staphylococcus aureus is also cultured in 46% to 51% of cases compared with only 8% in controls.[13]
Posterior blepharitis is associated with quantitative and qualitative changes to the meibomian glands and their secretions, with meibum breakdown by bacterial lipases thought to cause abnormal secretions and an unstable tear film.[1][14] Meibomian gland dysfunction is closely related to dry eye disease, which itself is associated with both staphylococcal and seborrhoeic blepharitis.[1][15] See Dry eye disease.
Demodex mites are considered an important cause of blepharitis.[9][10][16][17] Demodex folliculorum and Demodex brevis are more common in patients with blepharitis than in controls.[18][19]
Other predisposing factors include seborrhoeic dermatitis, ocular rosacea, and intraocular or lid surgery.[1]
Pathophysiology
Bacterial anterior blepharitis is associated with three primary mechanisms.[20][21][22][23]
Direct bacterial infection.
Response to bacterial toxins: topical application of filtrate from S aureus cultures can produce a toxic form of conjunctivitis and keratitis. Bacterial lipases that act on meibomian gland cholesterol esters can produce toxic free fatty acids and disrupt gland integrity and function. Free cholesterol can stimulate the growth of S aureus, producing synergism.
Delayed hypersensitivity reactions to bacterial antigens: enhanced cell-mediated immunity to S aureus has been demonstrated in patients with chronic blepharitis.
Posterior blepharitis involves structural alterations and secretory dysfunction of the meibomian glands.[1][5][24][25][26][27][28][29]
Meibomian glands secrete meibum, the external lipid layer of the tear film, which is responsible for decreasing tear film evaporation and preventing contamination.
Gland dysfunction can be obstructive (secondary to hyperkeratinisation of ductal epithelium) or atrophic (due to abnormal meibocytes).
Altered structure with gland drop-out in posterior blepharitis has been demonstrated with meibography, while hyperkeratinisation has been associated with altered acinar cell differentiation and gland function.
Meibum composition is altered. Different ratios of free fatty acids to cholesterol esters could promote sealing of the gland orifice.
Demodex mites are considered an important cause of blepharitis. Among the reported 94% of patients in whom Demodex was identified in an ophthalmic outpatient study, 92% had cylindrical dandruff, 58% had collarettes, and about 14% were diagnosed with blepharitis.[9] Demodex folliculorum appears to be associated with anterior blepharitis (affects the lash base), whereas Demodex brevis appears to be associated with posterior blepharitis (occupies the meibomian gland).[30]
Classification
Blepharitis is typically classified by anatomical location, namely anterior or posterior blepharitis.[1] There is overlap, and both anterior and posterior blepharitis may be present.
Further sub-categorisation is by presentation: anterior blepharitis referring to staphylococcal and seborrhoeic blepharitis; posterior blepharitis referring to meibomian gland dysfunction; or a combination thereof.[1][2]
Anterior blepharitis
Primarily involves the eyelid skin, base of the eyelashes, and the eyelash follicles.
Staphylococcal blepharitis
Lid erythema, telangiectasias, and collarettes (fibrinous scales) around the lashes.
Bulbar conjunctival hyperaemia and tarsal conjunctival papillary hypertrophy.
In patients with chronic inflammation, depigmentation of lashes, trichiasis (turning in of lashes), madarosis (loss of lashes), and eyelid margin thickening and ulceration can occur.
Corneal changes may result in visual impairment. The most common finding is punctate epithelial keratitis and appears as small punctate areas of fluorescein staining, typically involving the lower third of the cornea. Marginal infiltrates appear first as superficial stromal infiltrates near the limbus and later may evolve into ulceration. In phlyctenular keratitis, limbal nodules subsequently develop into marginal ulcers with no intervening space between the ulcer and the limbus.
About 50% of patients will have dry eye disease.
Seborrhoeic blepharitis
Greasy scales around the lashes.
Strongly associated with seborrhoeic dermatitis, which presents with flaking and greasy skin on the scalp, retroauricular area, glabella, and nasolabial folds.
Less frequent chronic corneal changes than seen in staphylococcal blepharitis.
About 25% to 40% of patients will have dry eye disease.
Demodex blepharitis
Lid margin hyperaemia
Cylindrical dandruff characterised by a collarette that covers the lash base and extends along the lash (further than with staphylococci).
Lash misalignment, trichiasis, and even madarosis can occur.
[Figure caption and citation for the preceding image starts]: Anterior blepharitis: collarettes with lid erythemaFrom the collection of Dr E. Akpek [Citation ends].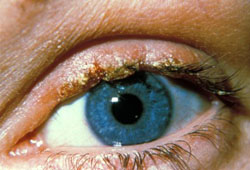 [Figure caption and citation for the preceding image starts]: Corneal complication: punctate epithelial erosions that stain with fluoresceinFrom the collection of Dr E. Akpek [Citation ends].
[Figure caption and citation for the preceding image starts]: Corneal complication: punctate epithelial erosions that stain with fluoresceinFrom the collection of Dr E. Akpek [Citation ends].
Posterior blepharitis
Posterior blepharitis (meibomian gland dysfunction): primarily affects the meibomian glands located on the posterior lid.[1][3][4][5]
Prominent vessels along the mucocutaneous junction
Frothy discharge along the lid margin
Thickening of the eyelid margin
Plugging of the meibomian orifices.
Sub-categories of meibomian gland dysfunction include hyposecretory, obstructive, and hypersecretory forms.[1]
[Figure caption and citation for the preceding image starts]: Posterior blepharitis: inspissated meibomian glands and lid telangiectasiaFrom the collection of Dr E. Akpek [Citation ends].

Use of this content is subject to our disclaimer