Aetiology
Amoebiasis is contracted by ingestion of the cyst of Entamoeba histolytica, which is found in faecally contaminated food and water. Transmission can also occur directly through sexual intercourse (especially oral-anal sexual contact) or contact with faecally contaminated objects. Cysts are environmentally stable, being resistant to chlorination and desiccation.[Figure caption and citation for the preceding image starts]: Cyst of Entamoeba histolytica: iodine stain of stool sampleReproduced from Current Concepts (2003); used with permission [Citation ends].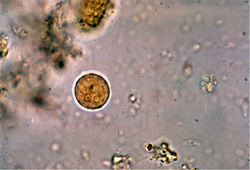 [Figure caption and citation for the preceding image starts]: Cyst of Entamoeba histolytica: unstained (A), and iodine stained (B) after formalin-ether concentration of stool sample.Original photos from National Center for Global Health and Medicine, Tokyo, Japan. [Citation ends].
[Figure caption and citation for the preceding image starts]: Cyst of Entamoeba histolytica: unstained (A), and iodine stained (B) after formalin-ether concentration of stool sample.Original photos from National Center for Global Health and Medicine, Tokyo, Japan. [Citation ends].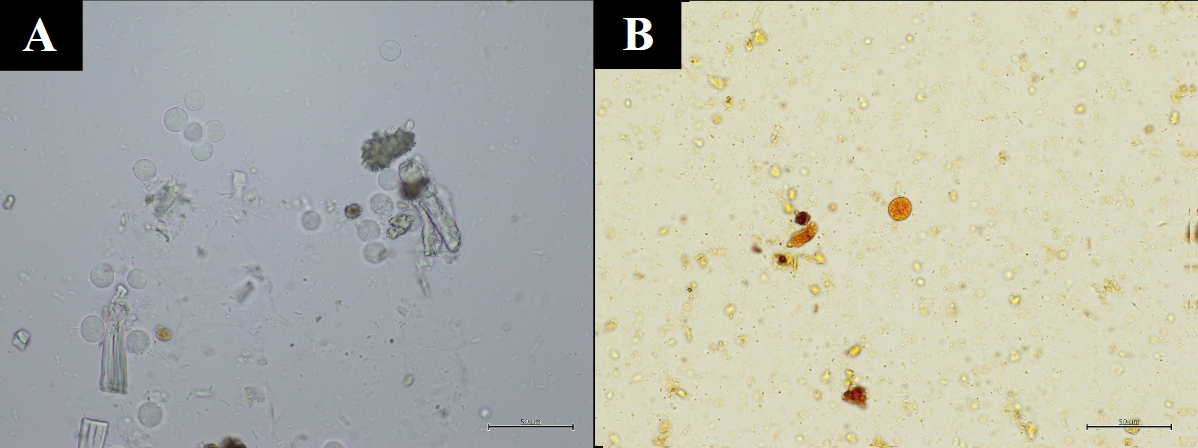
Pathophysiology
The life-cycle of E histolytica typically begins with ingestion of faecally contaminated food or water. Sexual transmission due to anal-oral contact is also possible.[11][16][17] The infective cyst form of the parasite survives passage through the stomach and small intestine. It excysts in the bowel lumen to form motile and potentially invasive trophozoites.
[Figure caption and citation for the preceding image starts]: Life-cycle of Entamoeba histolyticaReproduced from New England Journal of Medicine (2003); used with permission [Citation ends].
In most infections, the trophozoites aggregate in the intestinal mucin layer and form new cysts, resulting in a self-limiting and asymptomatic infection. However, galactose/N-acetyl-galactosamine (Gal/GalNAc) lectin-mediated adherence to and lysis of the colonic epithelium can initiate trophozoite invasion into the colon in some cases.
[Figure caption and citation for the preceding image starts]: Trophozoites of Entamoeba histolytica: trichrome stain of stool sampleReproduced from Clinical Infectious Diseases (1999); used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Trophozoite of Entamoeba histolytica with pseudopod (red arrow): direct unstained stool sample.Original photo from National Center for Global Health and Medicine, Tokyo, Japan. [Citation ends].
[Figure caption and citation for the preceding image starts]: Trophozoite of Entamoeba histolytica with pseudopod (red arrow): direct unstained stool sample.Original photo from National Center for Global Health and Medicine, Tokyo, Japan. [Citation ends]. [Figure caption and citation for the preceding image starts]: Amoebic ulcerations of the colon: colonic ulcers averaging 1 mm to 2 mm in diameter on gross pathologyReproduced from New England Journal of Medicine (2003); used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Amoebic ulcerations of the colon: colonic ulcers averaging 1 mm to 2 mm in diameter on gross pathologyReproduced from New England Journal of Medicine (2003); used with permission [Citation ends].
Neutrophils responding to invasion contribute to cellular damage at the site of invasion. Once the intestinal epithelium is invaded, extraintestinal spread into the peritoneum, liver, and other sites is possible.
[Figure caption and citation for the preceding image starts]: Posterior-anterior and lateral CXR of a patient with amoebic liver abscess: CXR findings include elevated right hemidiaphragm and evidence of atelectasisReproduced from New England Journal of Medicine (2003); used with permission [Citation ends].
Factors controlling invasion versus encystation include parasite quorum sensing signalled by the Gal/GalNAc lectin interactions of amoebae with the bacterial flora of the intestine, and host innate and acquired immune responses.
Trophozoites are always present in the gut in patients with amoebic diarrhoea and dysentery (diarrhoea with blood or mucus), and diagnosis should concentrate on identifying the parasite in stool by antigen detection and the serum antibody response against the invasive parasite.[1][2]
Invasion of the trophozoites through the intestinal epithelium leads to amoebic diarrhoea and colitis. Invasion involves a unique nibbling process by the parasite on the intestinal lining, termed amoebic trogocytosis.[18]
Haematogenous dissemination via the portal venous system results in amoebic liver abscess and infection in other sites such as the brain, although this is rare.[1][2][3][4][5]
[Figure caption and citation for the preceding image starts]: Entamoeba histolytica brain abscessReproduced from Transactions of the Royal Society of Tropical Medicine and Hygiene (2007); used with permission [Citation ends].
Classification
Taxonomy classification[6]
Infectious:
Entamoeba histolytica
Commensal:
Entamoeba dispar
Entamoeba moshkovskii
Entamoeba bangladeshi
Entamoeba coli
Entamoeba hartmanni
Entamoeba polecki
Entamoeba gingivalis
Clinical manifestations[2]
1. Asymptomatic colonisation
Presence of E histolytica in stool in the absence of colitis or extraintestinal manifestations
2. Intestinal amoebiasis
3. Extraintestinal amoebiasis
Amoebic liver abscess
Splenic abscess
Empyema
Pericarditis
Brain abscess
Use of this content is subject to our disclaimer