Elevated prolactin (PRL) levels are found in several pathological conditions and physiological states. One retrospective multicentre study of 1234 patients with hyperprolactinaemia showed that 56.2% had prolactinomas, 14.5% had drug-induced hyperprolactinaemia, 9.3% had macroprolactinaemia, 6.6% had non-functioning pituitary adenomas, 6.3% had primary hypothyroidism, 3.6% had idiopathic hyperprolactinaemia, and 3.2% had acromegaly.[12]Vilar L, Freitas MC, Naves LA, et al. Diagnosis and management of hyperprolactinemia: results of a Brazilian multicenter study with 1234 patients. J Endocrinol Invest. 2008 May;31(5):436-44.
http://www.ncbi.nlm.nih.gov/pubmed/18560262?tool=bestpractice.com
Thus, the aetiology of hyperprolactinaemia can be categorised as pathological, physiological, pharmacological, or idiopathic.
Pathological
Pathological hyperprolactinaemia is mainly due to PRL-secreting pituitary adenomas (prolactinomas), masses compressing the pituitary stalk (due to inhibition of dopamine transport from the hypothalamus to lactotroph cells), pituitary adenomas co-secreting growth hormone (GH), hypothyroidism (due to increased hypothalamic synthesis of thyrotropin-releasing hormone), and chronic renal failure (due to decreased PRL clearance).
Tumour pathologies
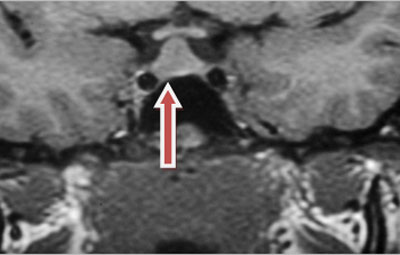
Prolactinomas, 90% of which are microprolactinomas (tumours <10 mm in diameter), account for 25% to 30% of functioning pituitary tumours and are the most common cause of hyperprolactinaemia. Macroprolactinomas (tumours >10 mm in diameter) are relatively uncommon and make up the remainder of prolactinomas.[Figure caption and citation for the preceding image starts]: MRI showing macroprolactinomaFrom the collection of Faidon Harsoulis, MD; used with permission [Citation ends].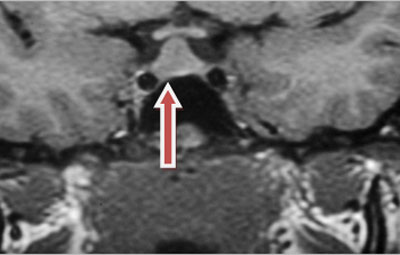 Macroprolactinomas present more frequently in men, possibly due to delayed diagnosis in this patient group.[3]Mah PM, Webster J. Hyperprolactinemia: etiology, diagnosis, and management. Semin Reprod Med. 2002 Nov;20(4):365-74.
http://www.ncbi.nlm.nih.gov/pubmed/12536359?tool=bestpractice.com
[13]Schlechte JA. Long-term management of prolactinomas. J Clin Endocrinol Metab. 2007 Aug;92(8):2861-5.
https://academic.oup.com/jcem/article/92/8/2861/2597201
http://www.ncbi.nlm.nih.gov/pubmed/17682084?tool=bestpractice.com
Serum PRL levels usually parallel tumour size, and it is rare for a prolactinoma to expand significantly without a marked increase in PRL.
Macroprolactinomas present more frequently in men, possibly due to delayed diagnosis in this patient group.[3]Mah PM, Webster J. Hyperprolactinemia: etiology, diagnosis, and management. Semin Reprod Med. 2002 Nov;20(4):365-74.
http://www.ncbi.nlm.nih.gov/pubmed/12536359?tool=bestpractice.com
[13]Schlechte JA. Long-term management of prolactinomas. J Clin Endocrinol Metab. 2007 Aug;92(8):2861-5.
https://academic.oup.com/jcem/article/92/8/2861/2597201
http://www.ncbi.nlm.nih.gov/pubmed/17682084?tool=bestpractice.com
Serum PRL levels usually parallel tumour size, and it is rare for a prolactinoma to expand significantly without a marked increase in PRL.
Most patients with PRL levels >6522 picomol/L (150 micrograms/L) have a prolactinoma. Macroprolactinomas usually present with PRL concentrations >10,870 picomol/L (250 micrograms/L), and sometimes >43,478 picomol/L (1000 micrograms/L).[1]Casanueva FF, Molitch ME, Schlechte JA, et al. Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas. Clin Endocrinol (Oxf). 2006 Aug;65(2):265-73.
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2265.2006.02562.x
http://www.ncbi.nlm.nih.gov/pubmed/16886971?tool=bestpractice.com
[13]Schlechte JA. Long-term management of prolactinomas. J Clin Endocrinol Metab. 2007 Aug;92(8):2861-5.
https://academic.oup.com/jcem/article/92/8/2861/2597201
http://www.ncbi.nlm.nih.gov/pubmed/17682084?tool=bestpractice.com
Patients presenting with a pituitary macroadenoma and mild hyperprolactinaemia <4348 picomol/L (100 micrograms/L) most likely have a non-secreting pituitary tumour rather than a prolactinoma.[14]Bevan JS, Burke CW, Esiri MM, et al. Misinterpretation of prolactin levels leading to management errors in patients with sellar enlargement. Am J Med. 1987 Jan;82(1):29-32.
http://www.ncbi.nlm.nih.gov/pubmed/3799691?tool=bestpractice.com
Nonetheless, these associations are not absolute.[1]Casanueva FF, Molitch ME, Schlechte JA, et al. Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas. Clin Endocrinol (Oxf). 2006 Aug;65(2):265-73.
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2265.2006.02562.x
http://www.ncbi.nlm.nih.gov/pubmed/16886971?tool=bestpractice.com
[13]Schlechte JA. Long-term management of prolactinomas. J Clin Endocrinol Metab. 2007 Aug;92(8):2861-5.
https://academic.oup.com/jcem/article/92/8/2861/2597201
http://www.ncbi.nlm.nih.gov/pubmed/17682084?tool=bestpractice.com
Most prolactinomas secrete only PRL, but approximately 5% contain somatotroph cells and thus also secrete GH.[15]Kasantikul V, Shuangshoti S. Pituitary adenomas: immunohistochemical: study of 90 cases. J Med Assoc Thai. 1990 Sep;73(9):514-21.
http://www.ncbi.nlm.nih.gov/pubmed/2262756?tool=bestpractice.com
They can rarely produce thyroid-stimulating hormone and adrenocorticotrophic hormone.
Masses affecting the hypothalamus and compressing the pituitary stalk usually result in PRL levels of <10,870 picomol/L (250 micrograms/L). These include non-functioning adenomas, craniopharyngiomas, gliomas, and metastatic disease.[1]Casanueva FF, Molitch ME, Schlechte JA, et al. Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas. Clin Endocrinol (Oxf). 2006 Aug;65(2):265-73.
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2265.2006.02562.x
http://www.ncbi.nlm.nih.gov/pubmed/16886971?tool=bestpractice.com
[2]Serri O, Chik CL, Ur E, et al. Diagnosis and management of hyperprolactinemia. CMAJ. 2003 Sep 16;169(6):575-81.
http://www.cmaj.ca/content/169/6/575.long
http://www.ncbi.nlm.nih.gov/pubmed/12975226?tool=bestpractice.com
[3]Mah PM, Webster J. Hyperprolactinemia: etiology, diagnosis, and management. Semin Reprod Med. 2002 Nov;20(4):365-74.
http://www.ncbi.nlm.nih.gov/pubmed/12536359?tool=bestpractice.com
Tumours that produce GH may also secrete PRL in nearly 25% of cases. These include mixed cell adenomas, acidophil stem cell-derived adenomas, mammosomatotroph cell-derived adenomas, and stalk compression by a solely GH-secreting macroadenoma.[16]Bonert VS, Melmed S. Acromegaly with moderate hyperprolactinemia caused by an intrasellar macroadenoma. Nat Clin Pract Endocrinol Metab. 2006 Jul;2(7):408-12.
http://www.ncbi.nlm.nih.gov/pubmed/16932323?tool=bestpractice.com
These tumours are associated with both acromegaly and hyperprolactinaemia, either by cells co-secreting GH and PRL or by the co-existence of two different cell populations, one secreting GH and the other PRL.
Non-tumour pathologies affecting the pituitary gland
Traumatic sectioning of the pituitary stalk.
Lymphocytic hypophysitis is caused by autoimmune conditions of the pituitary with lymphocytic infiltration. This state usually, but not exclusively, occurs at the end of gestation or in the early postnatal period. It may co-exist with other autoimmune diseases such as autoimmune thyroid diseases (mainly Hashimoto's thyroiditis), Addison's disease, type 1 diabetes mellitus, hypoparathyroidism, and autoimmune hepatitis. It can also be part of the autoimmune polyendocrinopathy syndrome.[1]Casanueva FF, Molitch ME, Schlechte JA, et al. Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas. Clin Endocrinol (Oxf). 2006 Aug;65(2):265-73.
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2265.2006.02562.x
http://www.ncbi.nlm.nih.gov/pubmed/16886971?tool=bestpractice.com
[2]Serri O, Chik CL, Ur E, et al. Diagnosis and management of hyperprolactinemia. CMAJ. 2003 Sep 16;169(6):575-81.
http://www.cmaj.ca/content/169/6/575.long
http://www.ncbi.nlm.nih.gov/pubmed/12975226?tool=bestpractice.com
[17]Beressi N, Beressi JP, Cohen R, et al. Lymphocytic hypophysitis. A review of 145 cases. Ann Med Interne (Paris). 1999 Jun;150(4):327-41.
http://www.ncbi.nlm.nih.gov/pubmed/10519020?tool=bestpractice.com
Granulomatous hypophysitis is caused by sarcoidosis and other granulomatous disorders such as tuberculosis, syphilis, histiocytosis X, and idiopathic granulomatous hypophysitis.[18]Bhardwaj M, Sharma A, Pal HK. Granulomatous hypophysitis. Neurol India. 2005 Sep;53(3):364-5.
http://www.neurologyindia.com/article.asp?issn=0028-3886;year=2005;volume=53;issue=3;spage=364;epage=365;aulast=Bhardwaj
http://www.ncbi.nlm.nih.gov/pubmed/16230818?tool=bestpractice.com
Primary hypothyroidism
Results in mild elevation of PRL levels (<2174 picomol/L [50 micrograms/L]) in 8% of cases.[19]Cortet-Rudelli C, Sapin R, Bonneville JF, et al. Etiological diagnosis of hyperprolactinemia. Ann Endocrinol (Paris). 2007 Jun;68(2-3):98-105.
http://www.ncbi.nlm.nih.gov/pubmed/17524347?tool=bestpractice.com
PRL levels normalise following thyroid hormone replacement therapy.
Among consecutive patients presenting with thyroid-related problems, PRL levels were elevated in 21% of patients with overt hypothyroidism and 8% of those with subclinical hypothyroidism.[20]Goel P, Kahkasha, Narang S, et al. Evaluation of serum prolactin level in patients of subclinical and overt hypothyroidism. J Clin Diagn Res. 2015 Jan;9(1):BC15-7.
https://www.jcdr.net/article_fulltext.asp?issn=0973-709x&year=2015&volume=9&issue=1&page=BC15&issn=0973-709x&id=5443
http://www.ncbi.nlm.nih.gov/pubmed/25737975?tool=bestpractice.com
Hypothyroidism is also associated with thyrotroph (as well as lactotroph) cell hyperplasia leading to significant pituitary enlargement. This can be radiologically confused with a prolactinoma.
Multiple endocrine neoplasia syndrome type I
Prolactinomas can present as a component of this syndrome in association with other endocrine tumours such as parathyroid tumours, enteropancreatic tumours (insulinomas, gastrinomas), or adrenal adenomas.[1]Casanueva FF, Molitch ME, Schlechte JA, et al. Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas. Clin Endocrinol (Oxf). 2006 Aug;65(2):265-73.
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2265.2006.02562.x
http://www.ncbi.nlm.nih.gov/pubmed/16886971?tool=bestpractice.com
Polycystic ovary syndrome (PCOS)
Hyperprolactinaemia, associated with PRL levels <2174 picomol/L (50 micrograms/L), is estimated to occur in 11% to 37% of women with PCOS, although the pathophysiological mechanism behind this link is poorly understood.[19]Cortet-Rudelli C, Sapin R, Bonneville JF, et al. Etiological diagnosis of hyperprolactinemia. Ann Endocrinol (Paris). 2007 Jun;68(2-3):98-105.
http://www.ncbi.nlm.nih.gov/pubmed/17524347?tool=bestpractice.com
[21]Kyritsi EM, Dimitriadis GK, Angelousi A, et al. The value of prolactin in predicting prolactinοma in hyperprolactinaemic polycystic ovarian syndrome. Eur J Clin Invest. 2018 Jul;48(7):e12961.
http://www.ncbi.nlm.nih.gov/pubmed/29845629?tool=bestpractice.com
[22]Davoudi Z, Araghi F, Vahedi M, et al. Prolactin Level in Polycystic Ovary Syndrome (PCOS): an approach to the diagnosis and management. Acta Biomed. 2021 Nov 3;92(5):e2021291.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8689332
http://www.ncbi.nlm.nih.gov/pubmed/34738596?tool=bestpractice.com
In one study of 122 women with PCOS and hyperprolactinaemia, around 60% had normal prolactin levels after polyethylene glycol precipitation, 27% were diagnosed with a pituitary adenoma, and 13% had idiopathic hyperprolactinaemia with a normal MRI scan.[22]Davoudi Z, Araghi F, Vahedi M, et al. Prolactin Level in Polycystic Ovary Syndrome (PCOS): an approach to the diagnosis and management. Acta Biomed. 2021 Nov 3;92(5):e2021291.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8689332
http://www.ncbi.nlm.nih.gov/pubmed/34738596?tool=bestpractice.com
PRL concentrations >85.2 micrograms/L in women with PCOS have been shown to be highly indicative of a prolactinoma (77% sensitivity, and 100% specificity).[21]Kyritsi EM, Dimitriadis GK, Angelousi A, et al. The value of prolactin in predicting prolactinοma in hyperprolactinaemic polycystic ovarian syndrome. Eur J Clin Invest. 2018 Jul;48(7):e12961.
http://www.ncbi.nlm.nih.gov/pubmed/29845629?tool=bestpractice.com
Chronic renal failure
Mild hyperprolactinaemia is seen in 30% of patients with chronic renal failure.[23]Saha MT, Saha HH, Niskanen LK, et al. Time course of serum prolactin and sex hormones following successful renal transplantation. Nephron. 2002;92(3):735-7.
http://www.ncbi.nlm.nih.gov/pubmed/12372970?tool=bestpractice.com
Cirrhosis
Causes a mild elevation in basal PRL in up to 20% of patients with cirrhosis.[1]Casanueva FF, Molitch ME, Schlechte JA, et al. Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas. Clin Endocrinol (Oxf). 2006 Aug;65(2):265-73.
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2265.2006.02562.x
http://www.ncbi.nlm.nih.gov/pubmed/16886971?tool=bestpractice.com
[2]Serri O, Chik CL, Ur E, et al. Diagnosis and management of hyperprolactinemia. CMAJ. 2003 Sep 16;169(6):575-81.
http://www.cmaj.ca/content/169/6/575.long
http://www.ncbi.nlm.nih.gov/pubmed/12975226?tool=bestpractice.com
[3]Mah PM, Webster J. Hyperprolactinemia: etiology, diagnosis, and management. Semin Reprod Med. 2002 Nov;20(4):365-74.
http://www.ncbi.nlm.nih.gov/pubmed/12536359?tool=bestpractice.com
Chest wall trauma or surgery
Leads to hyperprolactinaemia due to a reflex mediated through the mammary nerve.[1]Casanueva FF, Molitch ME, Schlechte JA, et al. Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas. Clin Endocrinol (Oxf). 2006 Aug;65(2):265-73.
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2265.2006.02562.x
http://www.ncbi.nlm.nih.gov/pubmed/16886971?tool=bestpractice.com
[2]Serri O, Chik CL, Ur E, et al. Diagnosis and management of hyperprolactinemia. CMAJ. 2003 Sep 16;169(6):575-81.
http://www.cmaj.ca/content/169/6/575.long
http://www.ncbi.nlm.nih.gov/pubmed/12975226?tool=bestpractice.com
[3]Mah PM, Webster J. Hyperprolactinemia: etiology, diagnosis, and management. Semin Reprod Med. 2002 Nov;20(4):365-74.
http://www.ncbi.nlm.nih.gov/pubmed/12536359?tool=bestpractice.com
This reflex is also the mechanism responsible for the hyperprolactinaemia associated with idiopathic granulomatous mastitis.[24]Pluguez-Turull CW, Nanyes JE, Quintero CJ, et al. Idiopathic granulomatous mastitis: manifestations at multimodality imaging and pitfalls. Radiographics. 2018 Mar-Apr;38(2):330-56.
http://www.ncbi.nlm.nih.gov/pubmed/29528819?tool=bestpractice.com
Ectopic hyperprolactinaemia
This condition is a paraneoplastic manifestation in which PRL is produced by tumours deriving from tissues other than the pituitary gland, such as ovarian or mesenchymal (perivascular epithelioid cell) tumours.[25]Kallenberg GA, Pesce CM, Norman B, et al. Ectopic hyperprolactinemia resulting from an ovarian teratoma. JAMA. 1990 May 9;263(18):2472-4.
http://www.ncbi.nlm.nih.gov/pubmed/2329635?tool=bestpractice.com
[26]Korytnaya E, Liu J, Camelo-Piragua S, et al. Ectopic prolactin secretion from a perivascular epithelioid cell tumor (PEComa). J Clin Endocrinol Metab. 2014 Nov;99(11):3960-4.
http://www.ncbi.nlm.nih.gov/pubmed/25127092?tool=bestpractice.com
Surgical resection of the causative tumour normalises PRL levels.
Pharmacological
Drug-induced hyperprolactinaemia is usually associated with PRL levels of <4348 picomol/L (100 micrograms/L).
Antipsychotics (phenothiazines, thioxanthenes, butyrophenones, and atypical antipsychotics) are the most common cause of drug-induced hyperprolactinaemia, with approximately 60% of women and 40% of men on these medicines (also known as neuroleptics) being affected.[27]Haddad PM, Wieck A. Antipsychotic-induced hyperprolactinemia: mechanisms, clinical features and management. Drugs. 2004;64(20):2291-314.
http://www.ncbi.nlm.nih.gov/pubmed/15456328?tool=bestpractice.com
Although the highest PRL elevations were noticed with the first-generation anti-psychotics, the second-generation ones can also cause hyperprolactinaemia. The highest rates have been reported with amisulpride, risperidone, and paliperidone (which raise PRL even at low doses), whereas aripiprazole and quetiapine have the most favourable profile. PRL elevations are usually observed at the initiation of treatment and are generally dose-dependent. Aripiprazole can even reduce PRL levels.[28]Peuskens J, Pani L, Detraux J, et al. The effects of novel and newly approved antipsychotics on serum prolactin levels: a comprehensive review. CNS Drugs. 2014 May;28(5):421-53.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4022988
http://www.ncbi.nlm.nih.gov/pubmed/24677189?tool=bestpractice.com
Other drugs implicated in the development of hyperprolactinaemia include:[29]Molitch ME. Medication-induced hyperprolactinemia. Mayo Clin Proc. 2005 Aug;80(8):1050-7.
https://www.mayoclinicproceedings.org/article/S0025-6196(11)61587-5/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/16092584?tool=bestpractice.com
[30]Teoh SK, Lex BW, Mendelson JH, et al. Hyperprolactinemia and macrocytosis in women with alcohol and polysubstance dependence. J Stud Alcohol. 1992 Mar;53(2):176-82.
http://www.ncbi.nlm.nih.gov/pubmed/1560669?tool=bestpractice.com
[31]Coker F, Taylor D. Antidepressant-induced hyperprolactinaemia: incidence, mechanisms and management. CNS Drugs. 2010 Jul;24(7):563-74.
http://www.ncbi.nlm.nih.gov/pubmed/20527996?tool=bestpractice.com
[32]Madhusoodanan S, Parida S, Jimenez C. Hyperprolactinemia associated with psychotropics: a review. Hum Psychopharmacol. 2010 Jun-Jul;25(4):281-97.
http://www.ncbi.nlm.nih.gov/pubmed/20521318?tool=bestpractice.com
[33]Sarkar DK. Hyperprolactinemia following chronic alcohol administration. Front Horm Res. 2010;38:32-41.
http://www.ncbi.nlm.nih.gov/pubmed/20616493?tool=bestpractice.com
Drugs that block dopamine receptors (metoclopramide, domperidone, risperidone, phenothiazines, tricyclic antidepressants, cimetidine)
Drugs that interfere with the synthesis or storage of dopamine (e.g., methyldopa, monoamine oxidase inhibitors [MAOIs])[29]Molitch ME. Medication-induced hyperprolactinemia. Mayo Clin Proc. 2005 Aug;80(8):1050-7.
https://www.mayoclinicproceedings.org/article/S0025-6196(11)61587-5/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/16092584?tool=bestpractice.com
Antidepressants (tricyclic and tetracyclic antidepressants, MAOIs, selective serotonin reuptake inhibitors, nefazodone, bupropion, venlafaxine)
Opiates and cocaine
Antihypertensives (e.g., verapamil, methyldopa)
Gastrointestinal drugs (metoclopramide, domperidone, histamine receptor [H2] blockers, protease inhibitors [conflicting data])
Oestrogen
Alcohol (excessive intake).
Physiological
Macroprolactinaemia
High levels of macroprolactin lead to reduced clearance rates of the PRL-IgG complex.
The prevalence of macroprolactinaemia in hyperprolactinaemic sera ranges from 15% to 46%.[1]Casanueva FF, Molitch ME, Schlechte JA, et al. Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas. Clin Endocrinol (Oxf). 2006 Aug;65(2):265-73.
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2265.2006.02562.x
http://www.ncbi.nlm.nih.gov/pubmed/16886971?tool=bestpractice.com
[6]Gibney J, Smith TP, McKenna TJ. Clinical relevance of macroprolactin. Clin Endocrinol (Oxf). 2005 Jun;62(6):633-43.
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2265.2005.02243.x
http://www.ncbi.nlm.nih.gov/pubmed/15943822?tool=bestpractice.com
[19]Cortet-Rudelli C, Sapin R, Bonneville JF, et al. Etiological diagnosis of hyperprolactinemia. Ann Endocrinol (Paris). 2007 Jun;68(2-3):98-105.
http://www.ncbi.nlm.nih.gov/pubmed/17524347?tool=bestpractice.com
It is thought to be more common in women with hyperprolactinaemia; however, it is unclear if this is a true difference.[34]Che Soh NAA, Yaacob NM, Omar J, et al. Global prevalence of macroprolactinemia among patients with hyperprolactinemia: a systematic review and meta-analysis. Int J Environ Res Public Health. 2020 Nov 6;17(21):8199.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7664288
http://www.ncbi.nlm.nih.gov/pubmed/33171973?tool=bestpractice.com
In the general population, the prevalence of macroprolactinaemia was previously reported as 0.2% in women and 0.02% in men; however, the overall prevalence is now estimated to be 3.7% with no sex difference.[34]Che Soh NAA, Yaacob NM, Omar J, et al. Global prevalence of macroprolactinemia among patients with hyperprolactinemia: a systematic review and meta-analysis. Int J Environ Res Public Health. 2020 Nov 6;17(21):8199.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7664288
http://www.ncbi.nlm.nih.gov/pubmed/33171973?tool=bestpractice.com
[35]Kasum M, Orešković S, Čehić E, et al. Laboratory and clinical significance of macroprolactinemia in women with hyperprolactinemia. Taiwan J Obstet Gynecol. 2017 Dec;56(6):719-24.
https://www.sciencedirect.com/science/article/pii/S1028455917302413?via%3Dihub
http://www.ncbi.nlm.nih.gov/pubmed/29241908?tool=bestpractice.com
Prevalent in idiopathic hyperprolactinaemia and has been reported in specific hyperprolactinaemia-related conditions such as antipsychotic-induced hyperprolactinaemia.[36]De Schepper J, Schiettecatte J, Velkeniers B, et al. Clinical and biological characterization of macroprolactinemia with and without prolactin-IgG complexes. Eur J Endocrinol. 2003 Sep;149(3):201-7.
https://eje.bioscientifica.com/view/journals/eje/149/3/201.xml
http://www.ncbi.nlm.nih.gov/pubmed/12943522?tool=bestpractice.com
Present in up to 40% of patients with systemic lupus erythematosus, possibly due to anti-PRL auto-antibodies.[37]Leanos A, Pascoe D, Fraga A, et al. Anti-prolactin autoantibodies in systemic lupus erythematosus patients with associated hyperprolactinemia. Lupus. 1998;7(6):398-403.
http://www.ncbi.nlm.nih.gov/pubmed/9736323?tool=bestpractice.com
Suspected when a hyperprolactinaemic patient lacks typical symptoms and/or radiographic evidence of a pituitary tumour. However, one isolated study of 106 participants found reports of amenorrhoea, galactorrhoea, and/or infertility in these patients.[38]Vallette-Kasic S, Morange-Ramos I, Selim A, et al. Macroprolactinemia revisited: a study on 106 patients. J Clin Endocrinol Metab. 2002 Feb;87(2):581-8.
https://academic.oup.com/jcem/article/87/2/581/2846759
http://www.ncbi.nlm.nih.gov/pubmed/11836289?tool=bestpractice.com
PRL levels are usually <4348 picomol/L (100 micrograms/L), with only 8.5% to 20.0% of patients having a PRL level 4348 picomol/L (100 micrograms/L).[19]Cortet-Rudelli C, Sapin R, Bonneville JF, et al. Etiological diagnosis of hyperprolactinemia. Ann Endocrinol (Paris). 2007 Jun;68(2-3):98-105.
http://www.ncbi.nlm.nih.gov/pubmed/17524347?tool=bestpractice.com
[38]Vallette-Kasic S, Morange-Ramos I, Selim A, et al. Macroprolactinemia revisited: a study on 106 patients. J Clin Endocrinol Metab. 2002 Feb;87(2):581-8.
https://academic.oup.com/jcem/article/87/2/581/2846759
http://www.ncbi.nlm.nih.gov/pubmed/11836289?tool=bestpractice.com
Physiological stress
Pregnancy, lactation, and nipple stimulation
In pregnancy, the rising oestrogen concentrations lead to high PRL levels via the direct stimulation of lactotroph cells. Increase in both the size and the number of lactotroph cells is observed during pregnancy. However, lactation is inhibited during pregnancy as a result of high levels of oestrogens and progesterone, the decline of which in the postnatal period allows lactation to occur.[39]Saleem M, Martin H, Coates P. Prolactin biology and laboratory measurement: an update on physiology and current analytical issues. Clin Biochem Rev. 2018 Feb;39(1):3-16.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6069739
http://www.ncbi.nlm.nih.gov/pubmed/30072818?tool=bestpractice.com
Nipple stimulation leads to hyperprolactinaemia due to a reflex mediated through the mammary nerve.
Other physiological causes include:
Exercise, food ingestion, sexual intercourse, sleep, and psychological stress.[39]Saleem M, Martin H, Coates P. Prolactin biology and laboratory measurement: an update on physiology and current analytical issues. Clin Biochem Rev. 2018 Feb;39(1):3-16.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6069739
http://www.ncbi.nlm.nih.gov/pubmed/30072818?tool=bestpractice.com
Idiopathic
Rarely, the underlying cause of hyperprolactinaemia (usually to levels of 4348 picomol/L [100 micrograms/L]) cannot be determined, and this condition is termed idiopathic hyperprolactinaemia.[1]Casanueva FF, Molitch ME, Schlechte JA, et al. Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas. Clin Endocrinol (Oxf). 2006 Aug;65(2):265-73.
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2265.2006.02562.x
http://www.ncbi.nlm.nih.gov/pubmed/16886971?tool=bestpractice.com
[2]Serri O, Chik CL, Ur E, et al. Diagnosis and management of hyperprolactinemia. CMAJ. 2003 Sep 16;169(6):575-81.
http://www.cmaj.ca/content/169/6/575.long
http://www.ncbi.nlm.nih.gov/pubmed/12975226?tool=bestpractice.com
[3]Mah PM, Webster J. Hyperprolactinemia: etiology, diagnosis, and management. Semin Reprod Med. 2002 Nov;20(4):365-74.
http://www.ncbi.nlm.nih.gov/pubmed/12536359?tool=bestpractice.com
Such patients may harbour microadenomas that are not detectable with computed tomography and magnetic resonance imaging scans.[40]Hattori N, Ishihara T, Ikekubo K, et al. Autoantibody to human prolactin in patients with idiopathic hyperprolactinemia. J Clin Endocrinol Metab. 1992 Nov;75(5):1226-9.
http://www.ncbi.nlm.nih.gov/pubmed/1430082?tool=bestpractice.com
Anti-PRL auto-antibodies, without the presence of autoimmune disease, have been detected in approximately 16% of cases of idiopathic hyperprolactinaemia.[40]Hattori N, Ishihara T, Ikekubo K, et al. Autoantibody to human prolactin in patients with idiopathic hyperprolactinemia. J Clin Endocrinol Metab. 1992 Nov;75(5):1226-9.
http://www.ncbi.nlm.nih.gov/pubmed/1430082?tool=bestpractice.com
[41]Hattori N, Ikekubo K, Ishihara T, et al. Effects of anti-prolactin autoantibodies on serum prolactin measurements. Eur J Endocrinol. 1994 May;130(5):434-7.
http://www.ncbi.nlm.nih.gov/pubmed/8180668?tool=bestpractice.com
 Macroprolactinomas present more frequently in men, possibly due to delayed diagnosis in this patient group.[3][13] Serum PRL levels usually parallel tumour size, and it is rare for a prolactinoma to expand significantly without a marked increase in PRL.
Macroprolactinomas present more frequently in men, possibly due to delayed diagnosis in this patient group.[3][13] Serum PRL levels usually parallel tumour size, and it is rare for a prolactinoma to expand significantly without a marked increase in PRL.