Case history
Case history #1
A 65-year-old man has a history of prior anterior wall myocardial infarction that occurred 2 years ago, complicated by severe left ventricular systolic dysfunction. While walking to the shops, he suddenly became aware of palpitations, diaphoresis, dizziness, and a sense of overwhelming malaise. One minute later, he turned grey, lost consciousness, and collapsed onto the floor. An ECG revealed sustained monomorphic ventricular tachycardia at 150 bpm. Cardiopulmonary resuscitation was initiated and the patient was cardioverted to sinus rhythm with a 200-J biphasic shock delivered from an external defibrillator. The patient regained consciousness. There was no antecedent chest discomfort and cardiac enzymes were negative after the event. Serum electrolytes were also normal. He received an implantable cardioverter/defibrillator the next day. [Figure caption and citation for the preceding image starts]: Sustained (monomorphic) ventricular tachycardiaFrom the collection of Prof Sei Iwai; used with permission [Citation ends].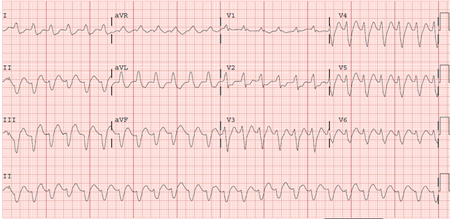
Case history #2
A 30-year-old woman presented to her general practitioner complaining of recurrent palpitations during exercise. She had previously been healthy and was on no medications. She described a long history of 'skipped heart beats'. Her doctor arranged a treadmill exercise test, which demonstrated good effort tolerance and no evidence of ischaemia. During early recovery she developed sustained ventricular tachycardia with a left bundle branch block, inferior axis morphology. Cardiac magnetic resonance imaging was performed that demonstrated normal biventricular function without evidence of myocardial scar or fatty infiltration. Electrophysiological testing was notable for inducible adenosine-sensitive ventricular tachycardia (with identical morphology to the clinical tachycardia) that was successfully ablated in a focal area in the right ventricular outflow tract. [Figure caption and citation for the preceding image starts]: Right ventricular outflow tract tachycardiaFrom the collection of Prof Sei Iwai; used with permission [Citation ends].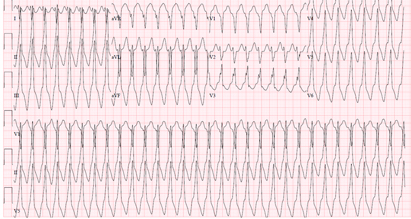
Other presentations
Ventricular arrhythmias may present with a diverse spectrum of symptoms, including palpitations, chest pain, and/or syncope, or may be asymptomatic. The type of symptom associated with the arrhythmia depends on its duration, its rate, and whether or not it is associated with abnormal perfusion to the heart or brain. Short-lived arrhythmias frequently are asymptomatic or manifest as brief palpitations, whereas longer and more rapid arrhythmias are frequently associated with presyncope or syncope. Sudden cardiac death is the most severe manifestation of ventricular arrhythmias; victims of sudden cardiac arrest rarely survive without cardiopulmonary resuscitation and prompt electrical defibrillation.
Use of this content is subject to our disclaimer