Approach
A complete history and physical examination are paramount in establishing a diagnosis of osteomalacia, with confirmatory laboratory and radiological tests.
Due to the non-specific symptoms and signs of osteomalacia, a high index of clinical suspicion is required for a diagnosis. In mild disease, patients are commonly asymptomatic. They may present radiologically, as osteopenia or pseudofractures, or with electrolyte abnormalities.
History
Key risk factors for osteomalacia obtainable from the history include the patient's age (more common in older patients), poor dietary intake of calcium and/or vitamin D, a history of limited sunlight exposure, sunscreen use, GI malabsorption, anticonvulsant use, and liver or renal impairment. Patients who are disabled or live in cold climates/high latitudes are at higher risk. It is also important to enquire about a family history of osteomalacia or rickets.
In mild or early disease, patients may be completely asymptomatic. Patients may complain of easy fatigability and malaise. They may also note diffuse bone pain and tenderness, difficulty rising from a sitting position, and a waddling gait.
Physical examination
The physical examination is remarkable for bone tenderness to percussion, poorly localised bony tenderness, and proximal muscle weakness. Pain in the hips may result in a waddling gait.
Laboratory evaluation
The laboratory evaluation of a patient with suspected osteomalacia should begin with measurement of the plasma concentrations of calcium, phosphate, creatinine, and alkaline phosphatase, as well as PTH and a 25-hydroxyvitamin D test.
Severe 25-hydroxyvitamin D deficiency <25 nanomol/L (10 nanogram/mL) can lead to hypocalcaemia, secondary hypophosphataemia, secondary hyperparathyroidism and an elevated alkaline phosphatase, which accounts for the majority of cases of osteomalacia. A 25-hydroxyvitamin D concentration of <25 nanomol/L (<10 nanogram/mL) is the threshold regarded internationally as defining the risk of osteomalacia.[17][47] A 24-hour urinary calcium measurement is useful in confirming vitamin D-deficient states as a cause of the osteomalacia.
If vitamin D deficiency is excluded, other causes of osteomalacia should be considered. The alkaline phosphatase level is usually elevated in all forms of osteomalacia, with the exception of hypophosphatasia.
The measurement of serum 1,25-dihydroxyvitamin D levels is not very helpful in differentiating the various causes of nutritional rickets or osteomalacia, because values may be low, normal, or elevated.[48]
In cases of renal phosphate wasting but normal calcium and alkaline phosphatase levels, a 24-hour urine phosphate with calculation of the fractional excretion of filtered phosphate needs to be determined, to confirm or rule out urinary wasting. In patients with hypophosphataemia and a normal anion gap acidosis, renal tubular acidosis type 2 needs to be considered.
Radiological evaluation
Bone x-rays are recommended to help display characteristic findings.
Long-standing secondary hyperparathyroidism, which is reversible with treatment of the underlying disorder, may be identified on x-ray. Osteosclerosis (increased bone density) may occur in patients with chronic kidney disease-mineral bone disorder (CKD-MBD).[49]
A dual-energy x-ray absorptiometry (DXA) scan is performed to confirm the low bone mass and aids in tracking the disease progression or remission. Osteomalacia presents as osteoporosis on DXA in up to 70% of cases, and therefore DXA cannot distinguish these disease entities.[50][Figure caption and citation for the preceding image starts]: Radiograph of the femoral shaft in a patient with osteomalacia demonstrating a 'pseudofracture' (also known as Looser's zone) on the medial aspect of the mid-femoral shaftFrom the collection of Bridget Sinnott, MD; used with permission [Citation ends].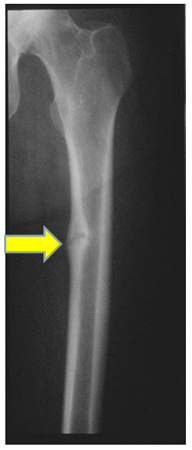
Biopsy
Bone biopsy with double tetracycline labelling is the definitive confirmatory test, but is rarely necessary. It is performed in complicated cases such as CKD-MBD or inherited disorders of bone metabolism.[Figure caption and citation for the preceding image starts]: Photomicrography of a normal transilial bone biopsy demonstrating mineralised osteoid (shown in purple)From the collection of Bridget Sinnott, MD; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Photomicrography of a transilial bone biopsy in a patient with osteomalacia demonstrating unmineralised osteoid (shown in purple). The width of the osteoid seams is substantially increasedFrom the collection of Bridget Sinnott, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Photomicrography of a transilial bone biopsy in a patient with osteomalacia demonstrating unmineralised osteoid (shown in purple). The width of the osteoid seams is substantially increasedFrom the collection of Bridget Sinnott, MD; used with permission [Citation ends].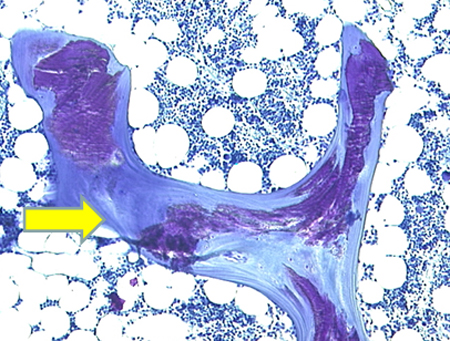
Use of this content is subject to our disclaimer