Approach
Diagnosis is based on clinical presentation and confirming laboratory results.
History and examination
The physician should obtain a detailed medical history specifying the date of onset and evolution of signs and symptoms. Special consideration should be given to obtaining any history related to either comorbidities potentially associated with bullous pemphigoid (such as neurological and cardiovascular diseases) or the potential therapy to be used.[28]
Evaluation should begin by examining the patient's skin, from head to toe. The patient should provide a description of lesions from onset until presentation to the doctor. If the patient presents in the early, prodromal, non-bullous phase, pruritus of variable intensity may be accompanied by eczematous or urticarial lesions for weeks or months.[29] In the bullous stage, characteristic, tense vesicles or bullae develop on apparently normal or erythematous skin of the pre-existing eczematous or urticarial eruption.
Blisters typically are found on the flexor surfaces of the arms and legs, axillae, groin, and abdomen.[5] The blisters may be several centimetres in diameter and contain a clear serous fluid that may become bloody after several days. If the blisters burst, eroded, crusty areas slowly heal to leave post-inflammatory hyperpigmentation with occasional milia. The lesions are usually symmetrical and favour the flexural aspects of the extremities, lower torso, and abdomen.
It is important to examine the oral mucosa, as oral lesions are present in up to 30% of patients.[4]
Laboratory evaluation
To diagnose bullous pemphigoid, a skin biopsy should be performed, preferably excising an entire blister with some adjacent unaffected tissue. A newly formed blister should be biopsied as intact as possible, taking care not to damage the tissue. The adjacent normal tissue should be biopsied, taking care not to damage the tissue. In the prodromal, non-bullous phase or in an atypical case, light microscopy findings may be less specific and non-diagnostic. The test may be repeated if suspicion is high and results are negative. A positive result shows a sub-epidermal blister with dermal inflammatory cell infiltrate rich in eosinophils.[Figure caption and citation for the preceding image starts]: Light microscopy: sub-epidermal blisterFrom the collection of Dr Vesna Petronic-Rosic [Citation ends]. [Figure caption and citation for the preceding image starts]: Fibrin network is present in the blister cavity while the dermal infiltrate contains many eosinophilsFrom the collection of Dr Vesna Petronic-Rosic [Citation ends].
[Figure caption and citation for the preceding image starts]: Fibrin network is present in the blister cavity while the dermal infiltrate contains many eosinophilsFrom the collection of Dr Vesna Petronic-Rosic [Citation ends].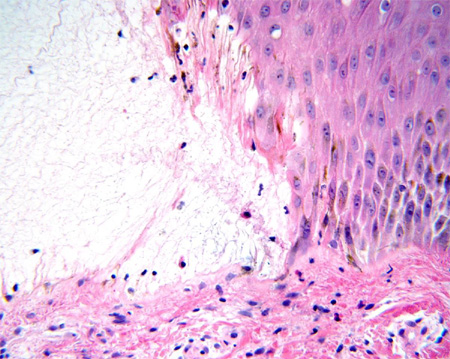 [Figure caption and citation for the preceding image starts]: Fibrin and eosinophils are present in the blister cavityFrom the collection of Dr Vesna Petronic-Rosic [Citation ends].
[Figure caption and citation for the preceding image starts]: Fibrin and eosinophils are present in the blister cavityFrom the collection of Dr Vesna Petronic-Rosic [Citation ends].
Direct immunofluorescence testing on the adjacent normal skin sample should also be performed, as this is the best available test.[30] The tissue must either be frozen immediately or placed in Michel's media and transported to the appropriate laboratory. Careful handling of the specimen is essential to ensure that results are accurate. This test is positive if a linear band of IgG and/or C3 (and rarely other Ig classes) appears along the basement membrane zone.[Figure caption and citation for the preceding image starts]: Linear band of IgG at the basement membrane zoneFrom the collection of Dr Vesna Petronic-Rosic [Citation ends].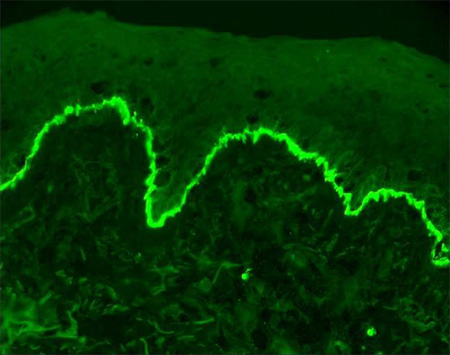 If a true-negative result is received, the ELISA test may be performed. This test identifies the specific bullous pemphigoid antigens.[31] Kits are available, but many medical centres still do not carry them.
If a true-negative result is received, the ELISA test may be performed. This test identifies the specific bullous pemphigoid antigens.[31] Kits are available, but many medical centres still do not carry them.
If a positive direct immunofluorescence result is attained, indirect immunofluorescence testing using patient serum is performed. Antibodies to bullous pemphigoid antigens indicate a positive result.[30] Only specialised laboratories analyse the results, so specimens must be handled carefully in transport. It is important to note the patient's previous treatment, as immunosuppressive therapy may falsely lower the antibodies.
Emerging tests
Immunoblotting and immunoprecipitation can be used to detect reactivity with BP230 and BP180.[9] The sensitivity of immunoblotting varies. In 75% of patients, a reaction occurs with the BP230 antigen, while in 50% of patients, a reaction occurs with the BP180 antigen.[32] Unlike immunoblotting, immunoprecipitation is performed with native, rather than denatured, protein and is more sensitive.
The fluorescence overlay antigen mapping technique facilitates differential diagnosis of the acquired subepidermal bullous skin disorders, but it is not routinely available.[33]
Use of this content is subject to our disclaimer