Investigations
1st investigations to order
FBC
Test
A routine test. An elevated WBC count occurs in most infectious causes of encephalitis. Depressed WBC counts and pancytopenia can be seen in HIV and immunomodulating/immunosuppressive drug use.
A relative lymphocytosis may occur in viral encephalitis. Rickettsial and viral fevers are associated with leukopenia and thrombocytopenia.
Eosinophilia is seen in certain parasitic infections (Baylisascaris procyonis).
Result
often elevated WBC
peripheral blood smear
Test
It is preferable to collect blood for the smear at the time of a fever spike in cases of suspected malarial illness, to increase the likelihood of finding the trophozoites. This is essential in malarial-endemic areas. Cytoplasmic inclusions in monocytes are seen in ehrlichiosis.
Result
detection of Plasmodium falciparum and Ehrlichia
serum electrolytes
Test
A routine test. Hyponatraemia is seen in rickettsial infections and syndrome of inappropriate secretion of antidiuretic hormone (particularly in TB), and anti-voltage-gated potassium channel-associated encephalitis (anti-leucine-rich glioma-inactivated 1/contactin-associated protein-like 2 encephalitis).
Result
hyponatraemia
liver function tests
Test
Coxiella burnetii, Rickettsia, tick-borne disease, cytomegalovirus, Epstein-Barr virus.
Result
elevated
blood cultures
Test
Two sets of blood cultures should be obtained as part of the routine work-up of a febrile illness. Arboviral cultures are rarely performed and are available only through specialised reference laboratories.
Result
detection and confirmation of systemic bacterial and fungal infections
throat swab
Test
Antigen detection tests and PCR are performed on throat swabs to detect enterovirus, poliovirus, cytomegalovirus, adenovirus, mumps, measles, influenza, and parainfluenza.
Result
detection of viruses
nasopharyngeal aspirate
Test
Obtained in children (less commonly used in adults) with respiratory symptoms.
Result
detection of respiratory viruses; polymerase chain reaction confirmation for adenovirus or influenza virus
chest radiography
Test
Routinely performed as part of a febrile work-up. May detect Mycoplasma,Legionella, influenza, parainfluenza, tuberculosis, Coccidioides, Histoplasma, blastomycosis, Coxiella burnetii, or sarcoidosis.
Result
may detect a non-infectious or infectious cause (e.g., tuberculosis, sarcoidosis, malignancy)
CT brain
Test
Used more as a screening tool due to its widespread availability and ease of acquisition in an uncooperative patient. CT brain is indicated in patients with GCS<12, focal neurological deficits, continuous or uncontrolled seizures, and papilledema.[61]
Post-contrast CT scans (if obtained) can demonstrate diffuse meningeal enhancement, which is a frequent co-occurrence in encephalitis. Vessel imaging up to the vertex must be obtained in cases with systemic infection in order to assess for mycotic aneurysms.
Herpes simplex virus encephalitis: an initial CT scan soon after admission will show a suggestive abnormality in about 25% to 80% of patients with HSV encephalitis, though it is not, on its own, diagnostic.[62] Hypodense lesions and mild mass effect in temporal lobes, insula, haemorrhage, and enhancement may be seen.
HIV-1: normal/mild atrophy with hypodense white matter lesions. Opportunistic infections and complications of HIV infection have their own characteristic findings.
Acute disseminated encephalomyelitis (ADEM): normal in 40%; low-density, flocculent, asymmetrical, multifocal punctate or ring-enhancing lesions can be seen.
West Nile virus: hyperintensities in the deep brain structures, including basal ganglia and thalamus.
Amoebae: diffuse oedema.[Figure caption and citation for the preceding image starts]: Non-contrast head CT of a patient with HSV encephalitis: shows subtle hypodensities involving the left insular region. Some blurring of grey-white margins and sulcal effacement over the left temporal region is discernibleFrom the personal collection of Catalina C. Ionita, MD; used with permission [Citation ends].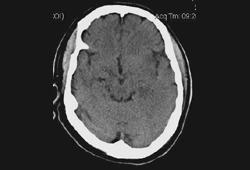
Result
frequently normal early in the clinical course of encephalitis, but may see more prominent changes
MRI brain
Test
Highly recommended (preferably initially) in suspected encephalitis and is invaluable in diagnosis.[48][63][64] However, MRI is less widely available compared with CT, and may require sedation for optimal image quality. MRI should include FLAIR, diffusion, T2*, and T1 sequences with and without gadolinium if possible.[48]
Early lesions in the form of signal abnormalities are seen in most cases.
Herpes simplex virus encephalitis: gyral oedema on T1, high signal on T2, FLAIR, and DWI (with increased diffusion on Apparent Diffusion Coefficient [ADC] maps) in temporal lobe and cingulate gyrus.
HIV: atrophy and non-specific white matter high signal on T2 and FLAIR. Opportunistic infections and complications of HIV infection have their own characteristic findings.
Polio and Coxsackie: T2 hyperintensities in the midbrain and anterior horn of the spinal cord.
Epstein-Barr virus: T2 hyperintensities in the basal ganglia, thalami, and cerebellum.
Varicella zoster virus: white and grey matter hyperintensities.
West Nile virus: Leptomeningeal periventricular enhancement.
Japanese encephalitis: T2 hyperintensities in bilateral thalami, brainstem, and cerebellum.
Acute disseminated encephalomyelitis (ADEM): multifocal, bilateral, asymmetrical, hyperintense lesions (ranging in size from <1 cm to multiple-centimetre confluent white matter abnormalities) of the white and grey matter on T2 and FLAIR.[18] Typically, lesions occur in the deep and subcortical white matter while sparing periventricular white matter, unlike multiple sclerosis.[18] Grey matter lesions can occur in ADEM, particularly in the thalami and basal ganglia.[18] Ring-enhancing lesions may be seen on post-contrast T1 images.
Rasmussen's encephalitis: T2 hyperintensities in cortex and white matter, cortical atrophy of the fronto-insular region, enlargement of lateral ventricle, and moderate atrophy of the caudate nucleus, all limited to one cerebral hemisphere.
Creutzfeldt-Jakob disease: T2/FLAIR hyperintensities and/or DWI changes in the globus pallidus, thalamus, and cortex (cortical ribboning).
Paraneoplastic limbic encephalitis: bilateral involvement of the medial temporal lobes and multifocal lesions on FLAIR and DWI.[Figure caption and citation for the preceding image starts]: The first 5 images are FLAIR images of patient with varicella zoster virus meningoencephalitis showing white and gray matter hyperintensities. The last image is T1 image with contrast showing parenchymal and diffuse leptomeningeal enhancementFrom the personal collection of Eric E. Kraus; used with permission [Citation ends].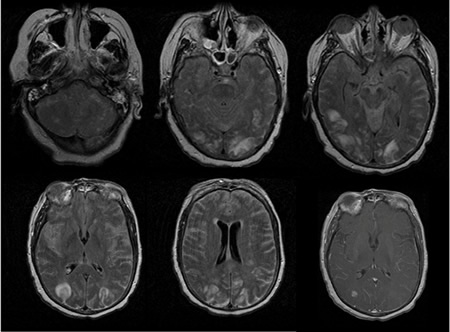 [Figure caption and citation for the preceding image starts]: Series of MRI images of brain of patient with acute disseminated encephalomyelitis: hyperintense lesions of fluid attenuated inversion recovery (FLAIR) involving the left cerebellar peduncleFrom the personal collection of Catalina C. Ionita, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Series of MRI images of brain of patient with acute disseminated encephalomyelitis: hyperintense lesions of fluid attenuated inversion recovery (FLAIR) involving the left cerebellar peduncleFrom the personal collection of Catalina C. Ionita, MD; used with permission [Citation ends].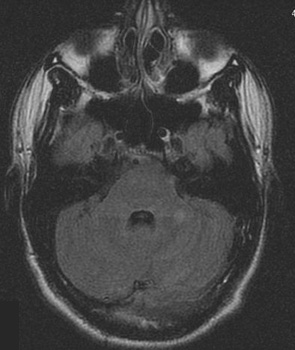 [Figure caption and citation for the preceding image starts]: Series of MRI images of brain of patient with acute disseminated encephalomyelitis: asymmetric 'fluffy' lesions over the bilateral ventricular horns and thalamiFrom the personal collection of Catalina C. Ionita, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Series of MRI images of brain of patient with acute disseminated encephalomyelitis: asymmetric 'fluffy' lesions over the bilateral ventricular horns and thalamiFrom the personal collection of Catalina C. Ionita, MD; used with permission [Citation ends].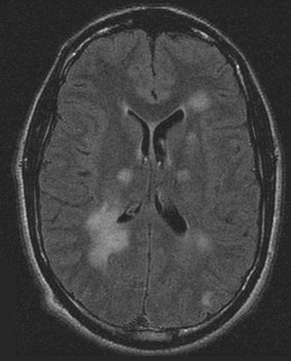 [Figure caption and citation for the preceding image starts]: Series of MRI images of brain of patient with acute disseminated encephalomyelitis: periventricular regionsFrom the personal collection of Catalina C. Ionita, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Series of MRI images of brain of patient with acute disseminated encephalomyelitis: periventricular regionsFrom the personal collection of Catalina C. Ionita, MD; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Series of MRI images of brain of patient with acute disseminated encephalomyelitis: centrum semiovaleFrom the personal collection of Catalina C. Ionita, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Series of MRI images of brain of patient with acute disseminated encephalomyelitis: centrum semiovaleFrom the personal collection of Catalina C. Ionita, MD; used with permission [Citation ends].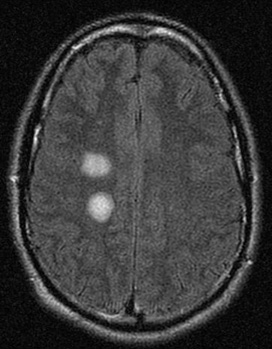 [Figure caption and citation for the preceding image starts]: Series of MRI images of brain of patient with acute disseminated encephalomyelitis: T1 post-gadolinium enhanced image shows ring enhancement around a lesion in the right centrum semiovale region and faint diffuse enhancement just above this areaFrom the personal collection of Catalina C. Ionita, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Series of MRI images of brain of patient with acute disseminated encephalomyelitis: T1 post-gadolinium enhanced image shows ring enhancement around a lesion in the right centrum semiovale region and faint diffuse enhancement just above this areaFrom the personal collection of Catalina C. Ionita, MD; used with permission [Citation ends].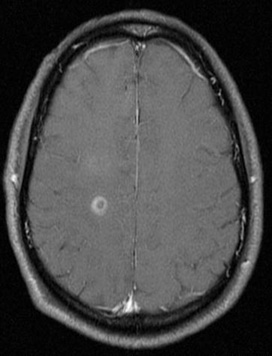 [Figure caption and citation for the preceding image starts]: Series of MRI images of brain of patient with acute disseminated encephalomyelitis: diffusion-weighted images from the same patient show high signal intensity in the same area, and this correlates with increased (bright on ADC maps) diffusionFrom the personal collection of Catalina C. Ionita, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Series of MRI images of brain of patient with acute disseminated encephalomyelitis: diffusion-weighted images from the same patient show high signal intensity in the same area, and this correlates with increased (bright on ADC maps) diffusionFrom the personal collection of Catalina C. Ionita, MD; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: MRI brain: the pulvinar sign (a term referencing bilateral pulvinar hyperintensity) in a patient with Creutzfeldt-Jakob disease on diffusion-weighted imagesFrom the personal collection of Leo H. Wang; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: MRI brain: the pulvinar sign (a term referencing bilateral pulvinar hyperintensity) in a patient with Creutzfeldt-Jakob disease on diffusion-weighted imagesFrom the personal collection of Leo H. Wang; used with permission [Citation ends].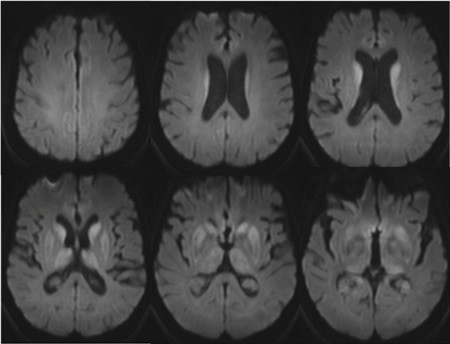 [Figure caption and citation for the preceding image starts]: MRI brain: cortical ribboning in a patient with Creutzfeldt-Jakob disease on diffusion-weighted imagesFrom the personal collection of Leo H. Wang; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: MRI brain: cortical ribboning in a patient with Creutzfeldt-Jakob disease on diffusion-weighted imagesFrom the personal collection of Leo H. Wang; used with permission [Citation ends].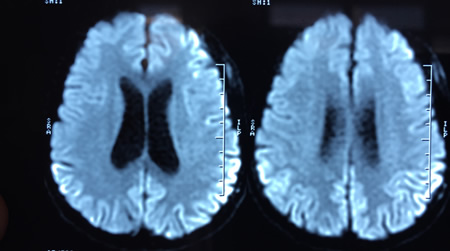
Result
depends on aetiology; often hyperintense lesions (T2 and fluid attenuated inversion recovery [FLAIR] sequences), increased diffusion on diffusion-weighted imaging (DWI) indicating oedema, contrast enhancement on T1 post-contrast sequences indicating blood-brain barrier breakdown; MRI is normal in up to a third of patients with autoimmune encephalitis.
electroencephalogram (EEG)
Test
EEG may be indicated to investigate seizures, status epilepticus, and altered consciousness.[13][48] Background slowing is an early and sensitive indicator of cerebral involvement but very non-specific, especially if the patient has required sedation.
Temporal lobe abnormalities are frequently seen in certain viral encephalitides, including HSV and VZV.
Repetitive sharp wave complexes over the temporal lobes or periodic lateralising epileptiform discharges can be seen in herpes simplex virus encephalitis.[65][66]
In subacute sclerosing panencephalitis, a typical generalised periodic EEG pattern repeating with intervals between 4 and 15 seconds, synchronous with the myoclonus of the patient, may be seen.[66][67]
In autoimmune encephalitis, EEG can provide evidence of focality when MRI is normal.[68] Common findings include slowing and epileptiform changes, but these are not specific.[68]
Creutzfeldt-Jakob disease findings: high-amplitude periodic (1 Hz) complexes. Extreme delta brush may be seen in anti-N-methyl-D-aspartate receptor encephalitis. This is characterised by rhythmic delta activity at 1 Hz to 3 Hz, with superimposed bursts of rhythmic 20 Hz to 30 Hz beta frequency activity 'riding' on each delta wave.[69]
Result
often shows background slowing
cerebrospinal fluid (CSF) analysis
Test
A lumbar puncture (LP) is recommended for patients with suspected encephalitis as long as there is no contraindication.[13] Contraindications to LP include mass effect causing potential herniation, coagulopathy, concern for lumbar spine abscess, or open skin lesion at the site of entry. Usually three or four tubes of cerebrospinal fluid (CSF) are collected by lumbar puncture for diagnostic studies. The first tube has the highest potential for contamination with skin flora and should not be sent to the microbiology laboratory for direct smears, culture, or molecular studies.[26] A minimum of 0.5 to 1.0 mL of CSF should be sent immediately after collection to the microbiology laboratory in a sterile container for bacterial testing.[26] Larger volumes (5-10 mL) increase the sensitivity of culture and are required for optimal identification of mycobacteria, fungi, or malignancy.[26] CSF should not be refrigerated.[26]
Opening pressure: usually elevated in bacterial, fungal, and TB meningoencephalitis, can be variable for other aetiologies.
Colour and clarity: variable, usually clear, can be mildly xanthochromic or blood-tinged in certain necrotising and haemorrhagic encephalitis (herpes simplex virus [HSV], acute haemorrhagic leukoencephalitis, listerial and primary amoebic meningoencephalitis).
Protein: normal or mildly elevated in most cases of viral encephalitis. Moderately elevated in bacterial infections, autoimmune diseases, limbic encephalitis, and acute disseminated encephalomyelitis. Markedly elevated in tuberculosis (TB) and sarcoidosis.
Glucose: normal to low normal in viral encephalitis except mumps, lymphocytic choriomeningitis virus, late stages of HSV-1. Low glucose levels are also seen in bacterial, fungal, parasitic, and neoplastic aetiologies.
Cell counts: in the absence of a traumatic tap, RBC count is usually normal. In cases of HSV (40%), acute haemorrhagic leukoencephalitis, listerial and primary amoebic meningoencephalitis, RBC >500/mm^3 can be seen. WBC usually elevated in most cases and suggestive of an inflammatory process of the brain parenchyma, meninges, or both (meningoencephalitis). May be normal early in disease course and in immunocompromised patients who cannot mount an inflammatory response.[70][71][72][73][74] In viral encephalitis an initial polymorphonuclear (PMN) predominance followed by a mononuclear shift in 24 to 48 hours (except in West Nile virus) is seen. Lymphocytosis (viruses, TB); atypical lymphocytes (Epstein-Barr virus, cytomegalovirus, rarely in HSV); PMN leukocytosis (bacterial infections, acute disseminated encephalomyelitis, acute haemorrhagic leukoencephalitis, amoebic infections, occasionally in some viruses such as West Nile virus). Eosinophilia (TB, fungal infection, Baylisascaris procyonis, Angiostrongylus cantonensis, Gnathostoma species).
CSF protein >1.0 g/L, or CSF glucose <2/3 peripheral glucose, or lymphocytic pleocytosis with subacute symptom onset suggests TB or fungal infection.
CSF protein >1.0 g/L or CSF glucose <2/3 peripheral glucose and neutrophilic predominance with acute symptom onset and recent antibiotic use suggests Streptococcus pneumoniae or Neisseria meningitidis.
Result
findings depend on aetiology; may have elevated WBC, normal/elevated protein, normal/low glucose, normal/elevated red blood cell (RBC); up to a third of patients with autoimmune encephalitis have normal CSF
CSF culture
Test
Culture: very useful in identifying aetiologies, particularly bacterial. Only useful for a few viruses (mumps, enterovirus, lymphocytic choriomeningitis virus). Viral cultures are rarely positive, and if negative do not exclude infection.[26]
Antigen testing: useful in rapidly identifying bacterial and fungal aetiologies of encephalitis.
Gram stain: detection of organisms in bacterial causes.
Acid-fast stain: tuberculosis.
India ink: Cryptococcus.
Result
findings depend on aetiology
CSF serology
Test
Serological indexing is required for definitive diagnosis, and compares CSF to serum-specific antibody levels in reference to total CSF, serum albumin, or total immunoglobulin. For viruses, a 4-fold rise in IgG from acute to convalescent specimens, or a single positive IgM, is also considered diagnostic.[75][76]
Result
findings depend on aetiology; more sensitive for detection of arboviruses, including West Nile virus
CSF polymerase chain reaction (PCR)
Test
CSF analysis should include PCR for common viral causes of encephalitis as a first-line screen and subsequent targeted PCRs for additional viruses based on the risk factors, exposure, and clinical picture.
Result
findings depend on aetiology; viruses (enterovirus, poliovirus, arboviruses, herpes simplex virus (HSV)-1, HSV-2, varicella zoster virus, cytomegalovirus, Epstein-Barr virus, lymphocytic choriomeningitis virus, adenovirus, measles, HIV, rabies); bacteria (Mycoplasma pneumoniae, tuberculosis); fungus (cryptococcus, aspergillosis)
Investigations to consider
stool enteroviral culture
Test
Obtained more frequently in children when gastrointestinal symptoms precede the development of encephalitis. Stool culture may also be used to detect poliovirus.
Result
detection of enterovirus
sputum culture
Test
Obtained in patients with a febrile illness and pulmonary symptoms or signs.
Result
detection of Mycoplasma, tuberculosis (acid-fast stain), and fungal infections
IgG and IgM antibodies (blood or CSF)
Test
Obtained when a viral cause for encephalitis is suspected. IgG and IgM antibodies directed against specific viral pathogens may be detected by serum or CSF studies.
Result
detection of IgG/IgM antibodies to enterovirus, poliovirus, arboviruses, varicella zoster virus, cytomegalovirus, Epstein-Barr virus, lymphocytic choriomeningitis virus, mumps, measles, HIV, rabies, and West Nile virus
PCR (blood)
Test
Obtained when a viral cause for encephalitis is suspected.
Result
detection of enterovirus, poliovirus, arboviruses, varicella zoster virus, cytomegalovirus, Epstein-Barr virus, and HIV
HIV serology/RNA test
Test
Reasonable to screen in all admitted patients, but should definitely be tested in people with risk factors for HIV infection. HIV may result in an acute encephalopathy with seroconversion. Quantitative viral RNA in plasma is used to confirm acute retroviral syndrome (i.e., symptomatic patients before the HIV antibody test is positive). HIV-associated encephalitis may also be due to an opportunistic infection.
Result
positive in cases of HIV infection
CSF biomarkers/prion protein assay
Test
Patients with suspected prion disease should have CSF testing. Real-time quaking-induced conversion assay (RT-QuIC) uses amplification technology to detect prion protein (PrPSc) and has higher detection sensitivity than biomarkers.[77]
Result
elevated 14-3-3 protein, elevated tau protein; detection of prion protein
paraneoplastic antibodies (blood and CSF)
Test
Obtained when an underlying cancer is found and/or suspected.
Result
paraneoplastic antibodies such as anti-N-methyl-D-aspartate receptor, anti-LGI1, anti-CASPR2, anti-Hu, anti-Yo, anti-Ri, anti-Tr, anti-CV2, anti-Ma, anti-amphiphysin may be found
abdominal/pelvic ultrasound
Test
Obtained when anti-N-methyl-D-aspartate receptor encephalitis is suspected. If malignancy screening is negative, repeating the assessment 3 to 6 months later should be considered in cases where the autoantibody found is strongly associated with malignancy.[1][52]
Result
detection of underlying ovarian teratoma
whole-body CT
Test
Performed later in the clinical course as part of the clinical work-up for suspected underlying cancers (e.g., lung, breast, or ovarian) that are associated with limbic or brainstem encephalitis. If malignancy screening is negative, repeating the assessment 3 to 6 months later should be considered in cases where the autoantibody found is strongly associated with malignancy.[1][52]
Result
detection of underlying cancers
whole-body PET scans
Test
Performed later in the clinical course as part of the clinical work-up for suspected underlying cancers (e.g., lung, breast, or ovarian) that are associated with limbic or brainstem encephalitis. If malignancy screening is negative, repeating the assessment 3 to 6 months later should be considered in cases where the autoantibody found is strongly associated with malignancy.[1][52]
Result
detection of underlying cancers
magnetic resonance spectroscopy
Test
Specialist centres only. Obtained in patients with a clinical diagnosis of encephalitis but in whom the aetiology is unknown, or if the diagnosis of encephalitis is suspected but cannot be differentiated from brain tumours.
Result
metabolic data aiding identification of aetiology
next-generation sequencing of CSF
Test
Specialist centres only. The use of personalised genomics to diagnose aetiological infectious agents.[78] As opposed to directed PCR amplification of a selected number of targets, technology is now available to detect organisms in an unbiased manner. Genetic material is isolated from organisms, and select DNA and RNA sequences can be amplified with universal primers. The sequence is then compared with publicly available sequences to identify the organism.
Result
detection and identification of organism
brain biopsy
Test
Currently the criterion standard for diagnosis. Not routinely performed as it is invasive, requires general anaesthesia, and is associated with some morbidity. With the increasing availability of MRI and PCR-based diagnostic methods, the need for brain biopsy is decreasing. It is still very useful in diagnostically challenging cases; stereotactic biopsy should be considered in patients with suspected encephalitis in whom no diagnosis has been made after the first week, especially if there are focal abnormalities on imaging and no clinical improvement.[13] If imaging shows nothing focal, an open biopsy, usually from the non-dominant frontal lobe, may be preferable.[13] Immunocytochemistry, in situ hybridisation, and PCR can be performed on biopsy/autopsy specimens, and have had a profound impact on the ability to diagnose the various aetiologies of encephalitis.
Classic encephalitic nodules are composed of a mixture of microglia, astrocytes, and lymphocytes around affected neurons, cytological features such as inclusion bodies (intranuclear in herpes simplex virus, varicella zoster virus, subacute sclerosing panencephalitis, and cytoplasmic Negri bodies in rabies), and cytomegalic cell changes (cytomegalovirus). In acute disseminated encephalomyelitis, multiple small demyelinated foci are arranged around small veins of the white matter, with infiltration by lymphocytes, macrophages, and microglia. In cryptococcal meningoencephalitis, the Cryptococcus can be seen. In HIV encephalitis, distinctive multinucleated giant cells can be seen; however, in CD8 encephalitis, intraparenchymal and perivascular CD8+ T-cells infiltrations are seen (while multi-nucleated giant cells are absent). In toxoplasmosis, the organism can be identified. Creutzfeldt-Jakob disease presents with spongiform changes.[Figure caption and citation for the preceding image starts]: Biopsy of brain from right temporal lobe: the classic H&E stain shows evidence of patchy but extensive inflammatory infiltrate of small mononuclear cells (lymphocytes) in the brain parenchyma, predominantly around the blood vessel walls. PCR studies of the biopsy sample were positive for EBV infectionFrom the personal collection of Catalina C. Ionita, MD; used with permission [Citation ends].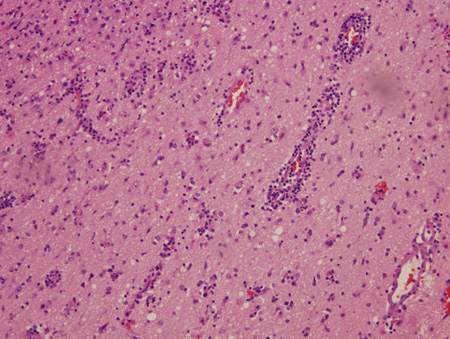 [Figure caption and citation for the preceding image starts]: Biopsy of brain from right temporal lobe: a close-up view of a blood vessel with its surrounding marked inflammatory infiltrate is also seen. PCR studies of the biopsy sample were positive for EBV infectionFrom the personal collection of Catalina C. Ionita, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Biopsy of brain from right temporal lobe: a close-up view of a blood vessel with its surrounding marked inflammatory infiltrate is also seen. PCR studies of the biopsy sample were positive for EBV infectionFrom the personal collection of Catalina C. Ionita, MD; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Biopsy from hippocampus of patient with rabies showing 2 neurons with eosinophilic Negri bodies (red arrows). These are found in areas, often with little inflammatory reaction. The blue arrows highlight microglial cellsFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Biopsy from hippocampus of patient with rabies showing 2 neurons with eosinophilic Negri bodies (red arrows). These are found in areas, often with little inflammatory reaction. The blue arrows highlight microglial cellsFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].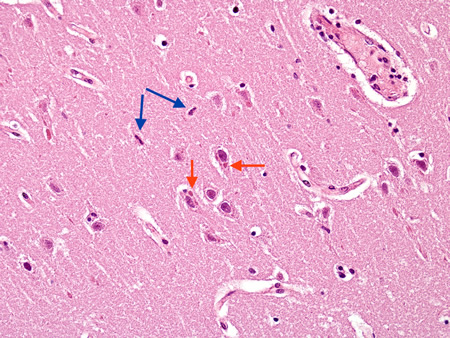 [Figure caption and citation for the preceding image starts]: Biopsy from hippocampus of patient with rabies showing neurons with eosinophilic Negri bodies (red arrow). The blue arrow highlights a collection of satelliting oligodendrocytesFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Biopsy from hippocampus of patient with rabies showing neurons with eosinophilic Negri bodies (red arrow). The blue arrow highlights a collection of satelliting oligodendrocytesFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].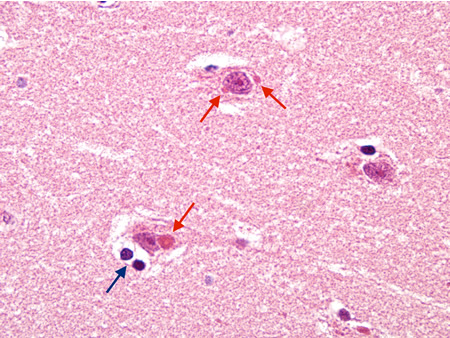 [Figure caption and citation for the preceding image starts]: Biopsy from hippocampus of patient with rabies showing a neuron with an eosinophilic cytoplasmic Negri body (red arrow). The blue arrow highlights a collection of microglial cells next to a blood vesselFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Biopsy from hippocampus of patient with rabies showing a neuron with an eosinophilic cytoplasmic Negri body (red arrow). The blue arrow highlights a collection of microglial cells next to a blood vesselFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].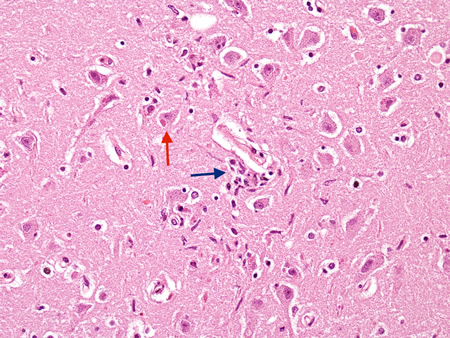 [Figure caption and citation for the preceding image starts]: Biopsy from the brainstem of an HIV patient with CMV encephalitis. The ependymal lining shows enlarged cells (arrows) with intranuclear inclusionsFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Biopsy from the brainstem of an HIV patient with CMV encephalitis. The ependymal lining shows enlarged cells (arrows) with intranuclear inclusionsFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].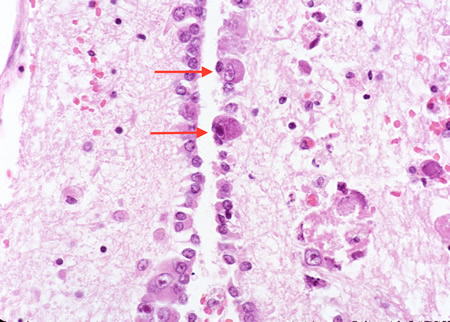 [Figure caption and citation for the preceding image starts]: Biopsy from cortex of neonate with CMV encephalitis showing enlarged cells (arrows) with intranuclear inclusions. The top arrow points to a neuron with two nuclei each with a nuclear inclusionFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Biopsy from cortex of neonate with CMV encephalitis showing enlarged cells (arrows) with intranuclear inclusions. The top arrow points to a neuron with two nuclei each with a nuclear inclusionFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].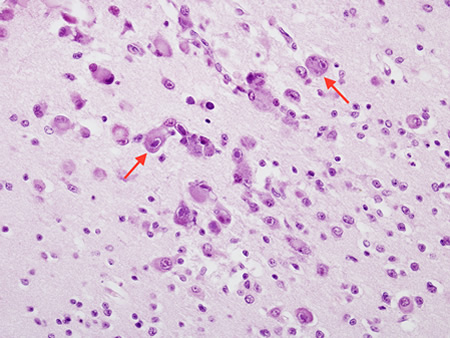 [Figure caption and citation for the preceding image starts]: Biopsy from brain of immunocompromised patient with cryptococcal meningitis at low magnification. The meninges are expanded (arrow), but the cortex is histologically relatively uninvolvedFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Biopsy from brain of immunocompromised patient with cryptococcal meningitis at low magnification. The meninges are expanded (arrow), but the cortex is histologically relatively uninvolvedFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].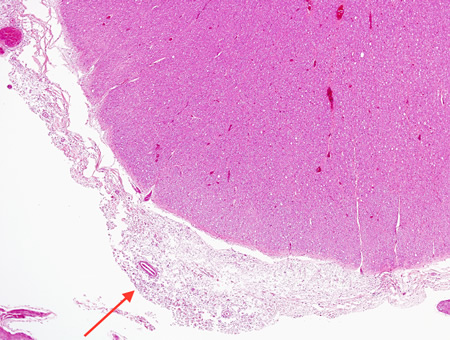 [Figure caption and citation for the preceding image starts]: Biopsy from brain of immunocompromised patient with cryptococcal meningitis showing the meninges with round translucent cryptococcal organism (red arrow) as well as a budding yeast (blue arrow)From the personal collection of Robert E. Schmidt; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Biopsy from brain of immunocompromised patient with cryptococcal meningitis showing the meninges with round translucent cryptococcal organism (red arrow) as well as a budding yeast (blue arrow)From the personal collection of Robert E. Schmidt; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Biopsy from brain of an immunocompetent patient with cryptococcal meningitis at low magnification showing the meninges with inflammation (red arrow)From the personal collection of Robert E. Schmidt; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Biopsy from brain of an immunocompetent patient with cryptococcal meningitis at low magnification showing the meninges with inflammation (red arrow)From the personal collection of Robert E. Schmidt; used with permission [Citation ends].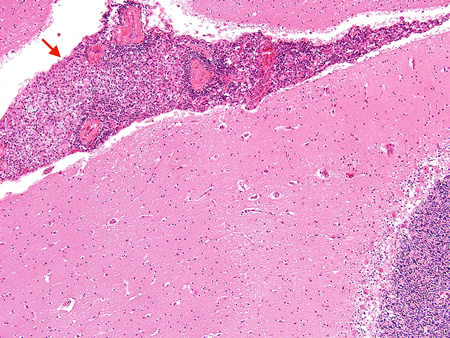 [Figure caption and citation for the preceding image starts]: Biopsy from brain of immunocompetent patient with cryptococcal meningitis showing the meninges with inflammatory cells and CryptococcusFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Biopsy from brain of immunocompetent patient with cryptococcal meningitis showing the meninges with inflammatory cells and CryptococcusFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].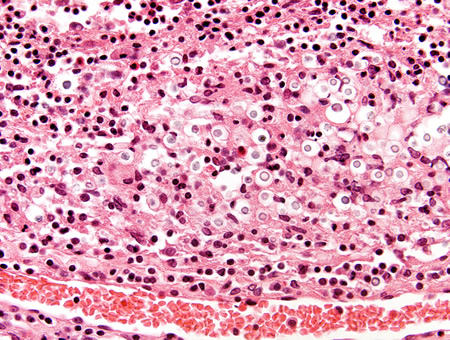 [Figure caption and citation for the preceding image starts]: Biopsy from meninges of patient with cryptococcal meningitis stained with mucicarmine, demonstrating fungal organisms, particularly in giant cellsFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Biopsy from meninges of patient with cryptococcal meningitis stained with mucicarmine, demonstrating fungal organisms, particularly in giant cellsFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].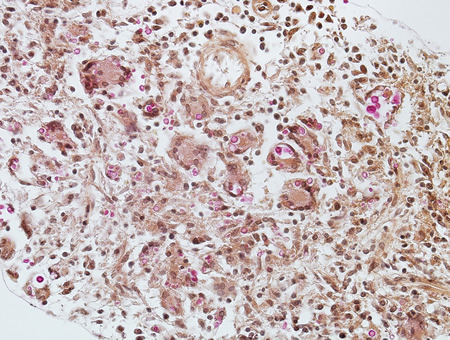 [Figure caption and citation for the preceding image starts]: Coronal slice of the brain of patient with cryptococcal meningoencephalitis showing classical appearance of “soap bubble” structures in the basal ganglia (arrows) resulting from the cryptococcal expansion of Virchow-Robbin spaces around the lenticulostriate vesselsFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Coronal slice of the brain of patient with cryptococcal meningoencephalitis showing classical appearance of “soap bubble” structures in the basal ganglia (arrows) resulting from the cryptococcal expansion of Virchow-Robbin spaces around the lenticulostriate vesselsFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].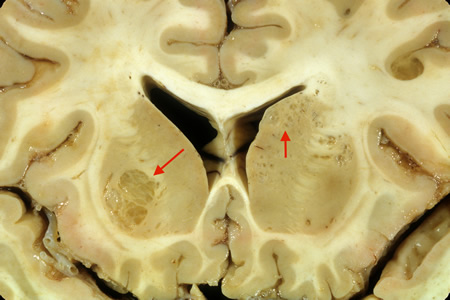 [Figure caption and citation for the preceding image starts]: Biopsy from basal ganglia of patient with cryptococcal meningoencephalitis showing cryptococcal (blue arrow) expansion of Virchow-Robbin spaces around a lenticulostriate vessel (red arrow)From the personal collection of Robert E. Schmidt; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Biopsy from basal ganglia of patient with cryptococcal meningoencephalitis showing cryptococcal (blue arrow) expansion of Virchow-Robbin spaces around a lenticulostriate vessel (red arrow)From the personal collection of Robert E. Schmidt; used with permission [Citation ends].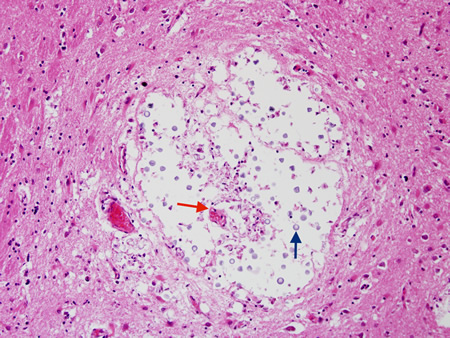 [Figure caption and citation for the preceding image starts]: Gross autopsy of brain of patient with cryptococcal meningitis showing the surface with a 'glazed' look. There is also a shunt presentFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Gross autopsy of brain of patient with cryptococcal meningitis showing the surface with a 'glazed' look. There is also a shunt presentFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Biopsy from brain of patient with subacute HIV leukoencephalitis showing the distinctive multinucleated cell (red arrow) in the white matter next to inflammatory cells in the Virchow-Robin spaceFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Biopsy from brain of patient with subacute HIV leukoencephalitis showing the distinctive multinucleated cell (red arrow) in the white matter next to inflammatory cells in the Virchow-Robin spaceFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].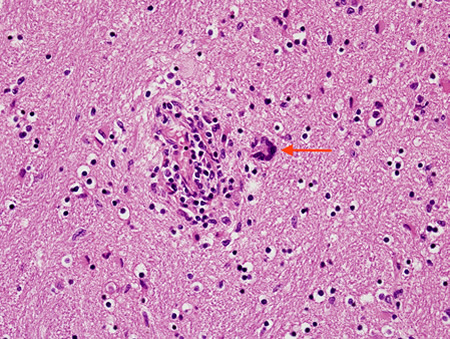 [Figure caption and citation for the preceding image starts]: Biopsy from brain of patient with subacute HIV leukoencephalitis showing the distinctive multinucleated cell (red arrow) in the white matterFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Biopsy from brain of patient with subacute HIV leukoencephalitis showing the distinctive multinucleated cell (red arrow) in the white matterFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].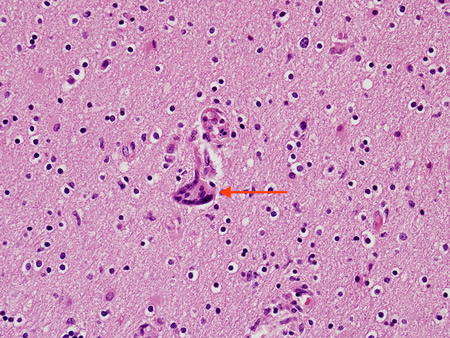 [Figure caption and citation for the preceding image starts]: Biopsy from brain of patient with subacute HIV encephalitis showing the distinctive multinucleated giant cell (red arrow), which contains the HIV virus. The multinucleated giant cells are from histiocyte/macrophage lineage. There is also associated astrocytosisFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Biopsy from brain of patient with subacute HIV encephalitis showing the distinctive multinucleated giant cell (red arrow), which contains the HIV virus. The multinucleated giant cells are from histiocyte/macrophage lineage. There is also associated astrocytosisFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].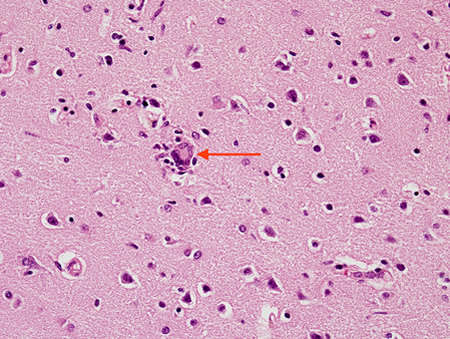 [Figure caption and citation for the preceding image starts]: Coronal slice of the brain of HIV patient in his 30s. He had subacute HIV encephalitis involving both the white matter and gray matter diffusely. The ventricles were enlarged reflecting white matter and cortical lossFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Coronal slice of the brain of HIV patient in his 30s. He had subacute HIV encephalitis involving both the white matter and gray matter diffusely. The ventricles were enlarged reflecting white matter and cortical lossFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].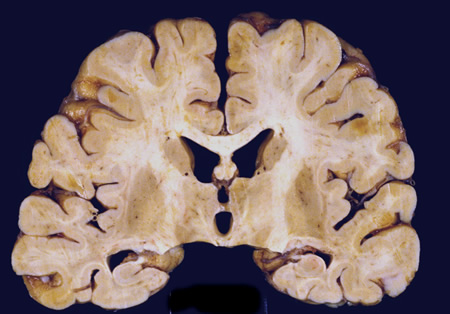 [Figure caption and citation for the preceding image starts]: Coronal slice of the brain of an HIV patient with toxoplasmosis, showing infection of the periventricular superior part of the left thalamusFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Coronal slice of the brain of an HIV patient with toxoplasmosis, showing infection of the periventricular superior part of the left thalamusFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].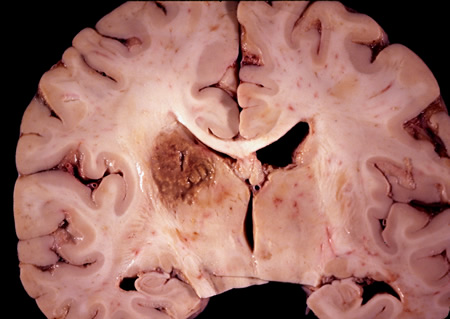 [Figure caption and citation for the preceding image starts]: Biopsy of the brain of an HIV patient with toxoplasmosis, showing encysted bradyzoites (red arrow) and tachyzoites (blue arrow)From the personal collection of Robert E. Schmidt; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Biopsy of the brain of an HIV patient with toxoplasmosis, showing encysted bradyzoites (red arrow) and tachyzoites (blue arrow)From the personal collection of Robert E. Schmidt; used with permission [Citation ends].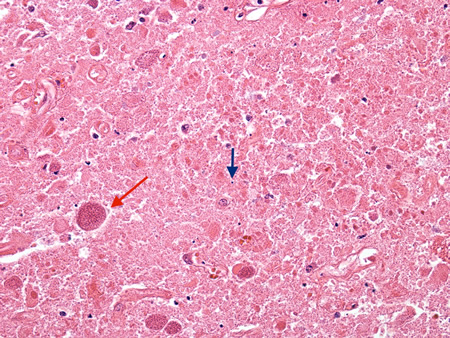 [Figure caption and citation for the preceding image starts]: Biopsy of HIV patient with toxoplasmosis, showing both pieces of cellular debris and tachyzoites. The tachyzoites are round, smooth and hard to identify without antibody staining (see next image)From the personal collection of Robert E. Schmidt; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Biopsy of HIV patient with toxoplasmosis, showing both pieces of cellular debris and tachyzoites. The tachyzoites are round, smooth and hard to identify without antibody staining (see next image)From the personal collection of Robert E. Schmidt; used with permission [Citation ends].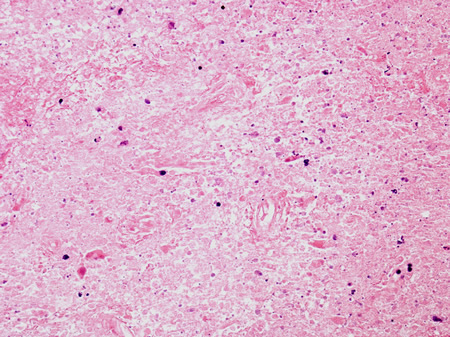 [Figure caption and citation for the preceding image starts]: Biopsy of HIV patient with toxoplasmosis, with the tachyzoites identified using immunohistochemistryFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Biopsy of HIV patient with toxoplasmosis, with the tachyzoites identified using immunohistochemistryFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].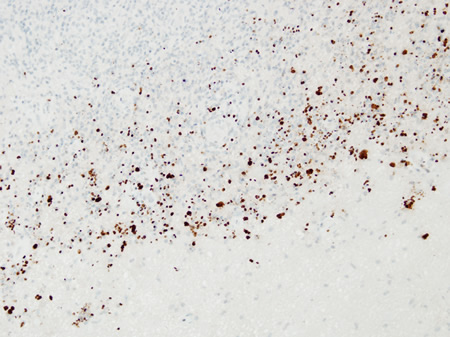 [Figure caption and citation for the preceding image starts]: Biopsy of the posterior thalamus of the patient with Creutzfeldt-Jakob Disease showing the spongiform changesFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Biopsy of the posterior thalamus of the patient with Creutzfeldt-Jakob Disease showing the spongiform changesFrom the personal collection of Robert E. Schmidt; used with permission [Citation ends].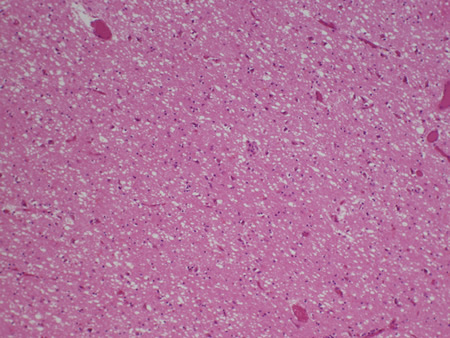
Result
damage to the brain parenchyma (usually nerve cell damage or loss, eventually demyelination), reactive gliosis, and inflammatory cellular infiltration
Use of this content is subject to our disclaimer