Investigations
1st investigations to order
CXR
Test
Invasive aspergillosis (IA): a CXR may be useful in high-risk patients with pulmonary symptoms. However, it may be completely normal. Findings are highly non-specific. If IA is suspected, high-resolution CT scan of the chest is indicated. Plain x-rays of sinuses are not useful in the diagnosis of IA.
Chronic pulmonary aspergillosis: CXR is the initial imaging method, but CT scan can provide better definition and location of findings.[3]
Result
invasive aspergillosis: nodules, consolidation, non-specific infiltrates, pleural-based lesions and cavities; may be normal; chronic pulmonary aspergillosis: one or more lung cavities with or without aspergilloma, infiltrates, nodules, pleural thickening, parenchymal damage, and fibrosis; aspergilloma: upper lobe mobile intracavitary mass with an air-crescent in the periphery
high-resolution chest CT scan
Test
Invasive aspergillosis (IA): in high-risk patients (e.g., patients with leukaemia and neutropenia, stem cell recipients, solid organ transplant recipients, patients with chronic granulomatous disease (CGD) or other primary immunodeficiency, patients with chronic lung disease receiving corticosteroids, patients receiving immunosuppressive drugs) with clinical features suggestive of pulmonary IA, CT scan is the principal radiological test. No radiographic contrast is required. Specific findings are well studied only in patients with leukaemia and in stem cell recipients.
Chronic pulmonary aspergillosis: a CT scan provides a better yield than a CXR.
Result
invasive aspergillosis: specific: nodules (1 cm or more in size) with or without halo sign or air-crescent sign; non-specific: micronodules, infiltrates, ground-glass opacities, pleural effusions; chronic pulmonary aspergillosis: one or more lung cavities with or without aspergilloma, infiltrates, nodules, pleural thickening, parenchymal damage, and fibrosis; aspergilloma: upper-lobe cavitary mass with intracavitary contents with adjacent pleural thickening
high-resolution sinuses CT scan
Test
Invasive aspergillosis: suggestive of aggressive infection.
Aspergilloma: paranasal sinuses may reveal space-occupying lesions without bone erosion.
Result
opacity/mass within the sinus cavity, bone erosion of the surrounding sinus walls
high-resolution brain CT scan
Test
Invasive aspergillosis: suggestive of aggressive invasive infection.
Result
focal lesions
MRI sinuses
Test
In sinus invasive aspergillosis disease, MRI scan helps to identify exact location, number of lesions, surrounding oedema, and adjacent bony erosion if any.
Result
sinus opacity and/or bone erosion
MRI brain
Test
Invasive aspergillosis (IA): in cerebral IA disease, MRI scan helps to identify exact location and number of lesions, and surrounding oedema.
Result
space-occupying lesions with surrounding oedema, abscesses, haemorrhage
serum Aspergillus galactomannan (GM) antigen by enzyme immunoassay (EIA)
Test
In suspected cases of invasive aspergillosis, the serum GM by EIA may be helpful. When serially performed, the sensitivity and specificity of this test are high, particularly in patients with acute leukaemia or in stem cell transplant recipients. In other populations, the sensitivity has a wide variability or is not well established.
A positive result in a high-risk patient with compatible clinical/radiological findings is suggestive of the diagnosis, thus eliminating the need for an invasive diagnostic procedure such as open lung biopsy.
False-positive results may be due to intake of food containing GM (used as a stabiliser in ice cream, cream cheese, fruit preparations, and salad dressings), other fungal infections (e.g., histoplasmosis, cryptococcosis, and blastomycosis), and use of antibiotics such as piperacillin-tazobactam.
False-negative results may be seen in focal infections or in patients receiving mould-active antifungal drugs.
Serial monitoring of serum GM results may be helpful in early diagnosis, thus diminishing the need for antifungal prophylaxis. Treatment progress may also be assessed with serial GM testing. This test is not widely available in all hospital laboratories.
Result
2 positive results of optical index ratio 0.5 or greater in the same blood sample
sputum culture
Test
Sputum is usually absent in patients with invasive aspergillosis. When present, sputum may show Aspergillus on cultures.
Presence of the organism in sputum needs cautious interpretation, dependent on patient's immune status. In immunocompetent patients, recovery of Aspergillus may represent colonisation, not invasion. In immunocompromised patients, Aspergillus in sputum may indicate infection. Sputum examination may have higher yield in post-bronchoscopy specimens. Overall, the sputum yield is low.
In chronic pulmonary aspergillosis, culture positivity rates vary widely and results should be interpreted with caution.[3][89] Testing multiple samples increases the probability of a positive test, but the majority of patients have negative sputum cultures.[2]
Result
Aspergillus species
sputum smear
Test
Sputum is usually absent in patients with invasive aspergillosis.
Presence of the organism in sputum needs cautious interpretation, dependent on the patient's immune status.
This test is usually negative in patients with aspergilloma.
Result
positive for hyphal elements
Investigations to consider
BAL Aspergillus galactomannan (GM) antigen
Test
BAL fluid Aspergillus GM test is reliable for early diagnosis of IA and has a higher sensitivity than in blood (85% to 90% compared with 40% to 47%).[90][91] Data are mostly from patients with suspected pulmonary aspergillosis who have underlying haematological malignancies.
BAL fluid Aspergillus GM test can be used for diagnosis of chronic pulmonary aspergillosis, but specificity and sensitivity is lower than Aspergillus antibody tests.[3]
Result
positive in BAL when optical density index ≥1.5
bronchoscopy with bronchoalveolar lavage (BAL) fungal stain
Test
BAL fluid may be positive when tested for fungi with Gomori's methenamine silver (GMS) staining. However, the yield is low (25% to 40%). In focal disease of the lung, the yield may be lower. In seriously ill patients with dyspnoea, or in patients with severe thrombocytopenia, the procedure is risky and difficult to perform.
Result
positive for hyphal elements
bronchoscopy with BAL fungal culture
Test
BAL fluid may be positive when tested for fungi with appropriate culture. However, the yield is low, in the range of 25% to 40%. In focal disease of the lung, the yield may be lower. In seriously ill patients with dyspnoea, or in patients with severe thrombocytopenia, the procedure is fraught with risks, and thus is difficult to perform.
Result
Aspergillus species
polymerase chain reaction
Test
Polymerase chain reaction (PCR) diagnosis, based on amplification of Aspergillus-specific fungal genes (usually ribosomal DNA), has shown considerable promise.
PCR-based test results may be falsely positive because of the ubiquitous presence of Aspergillus conidia.
Combining the PCR-based test with other non-invasive non-culture-based diagnostic methods (i.e., serum GM test and serum beta-D-glucan assay) is an important area for early diagnosis of invasive aspergillosis.
PCR testing of respiratory secretions can be used for diagnosis of chronic pulmonary aspergillosis; sensitivity is lower than antibody testing, but higher than culture.[2][87]
Result
positive
serum (1-3)-beta-D-glucan
Test
This test is positive in cases of invasive infections due to fungi that contain beta-glucan in the cell walls. Zygomycetes and Cryptococcus do not contain beta-glucan, while most other fungi do. Thus, unlike serum GM, this test is not specific for Aspergillus.
Neutropenic patients and stem cell recipients are the most well-studied populations; data in other populations are lacking. Sensitivity and specificity varies widely across studies.[85]
False-positive results are common in the presence of glucan-contaminated blood collection tubes, gauze, membrane filters, albumin, and intravenous immunoglobulin.
Result
positive: 80 picograms/mL or greater; negative: <60 picograms/mL
serum Aspergillus IgG
Test
In patients with imaging and history suggestive of chronic pulmonary aspergillosis (CPA), diagnosis can be confirmed with serum Aspergillus IgG or precipitins.[3]
Aspergillus IgG antibody test is the most sensitive test for CPA.[2] Serum IgG antibodies to Aspergillus or precipitins are positive in most patients with CPA.
False-negative cases may be seen in patients receiving corticosteroid therapy or in those with aspergilloma due to species other than A fumigatus.[86]
Result
serum IgG antibodies to Aspergillus
tissue biopsy
Test
Invasive aspergillosis: most definitive method of diagnosis. Ideal, but invasive. Tissue biopsy may be obtained by transbronchial approach, CT-guided needle aspiration (for peripheral lesions), video-assisted thoracoscopic surgery (VATS) biopsy, or open lung biopsy. Specimen obtained by transbronchial or CT-guided approach is generally suboptimal and may be associated with complications such as uncontrolled bleeding or pneumothorax. VATS is the preferred method, as biopsy is obtained under direct vision and is less invasive compared with open lung biopsy.
Thrombocytopenia is common in leukaemia and stem cell recipients, making invasive procedures hazardous. Often a biopsy procedure cannot be performed in view of platelet transfusion-refractory thrombocytopenia or severe illness, thus leading the clinicians to make empirical treatment choices. Other biopsy sites may include skin, sinus tissue, brain, or, uncommonly, bone, heart, pericardium, or abdominal organs. [Figure caption and citation for the preceding image starts]: Gomori's methenamine silver (GMS) stain of lung tissue showing dichotomously branching, septate hyphae of AspergillusFrom the collection of Dr P. Chandrasekar; used with permission [Citation ends].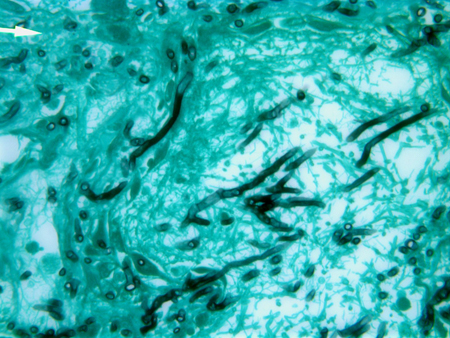
Chronic pulmonary aspergillosis: in certain cases microscopic examination of tissue obtained by biopsy is necessary for diagnosis. If biopsy shows that hyphae are invading the lung parenchyma, then acute or subacute invasive aspergillosis is diagnosed.[3]
Aspergillus nodules are diagnosed after excision biopsy. Single nodules that are completely excised may not need any further treatment.[3][4]
Result
invasive aspergillosis: acute angular branching, filamentous, septate hyphae with angio-invasion, inflammatory infiltrate, and tissue necrosis; chronic pulmonary aspergillosis: inflammatory cells, fibrosis, granulomata, and hyphae; aspergilloma: masses of fungal mycelia, inflammatory cells, tissue debris, fibrin, and mucus
tissue fungal culture
Test
Specimens obtained by biopsy must be sent in saline for microbiological culture and in formalin for pathology. Sampling errors may occur during biopsy; thus, tissue specimens may be fungal stain- and/or culture-negative.
The appearance of colony and the morphology of conidia/conidiophores help in species identification.
Result
Aspergillus species
tissue fungal stain
Test
Specimens obtained by biopsy must be sent in saline for microbiological culture and in formalin for pathology. Sampling errors may occur during biopsy; thus, tissue specimens may be fungal stain- and/or culture-negative.
Result
positive for hyphal elements
Use of this content is subject to our disclaimer