Investigations
1st investigations to order
FBC
Test
All patients should have an FBC on initial presentation.[70][71]
Anaemia can be due to chronic inflammation, chronic blood loss, iron malabsorption, and/or malabsorption of vitamin B12 or folic acid.
Leukocytosis is associated with acute or chronic inflammation, abscess, or corticosteroid treatment.
Thrombocytosis is a useful marker of active inflammation.
Result
anaemia; leukocytosis; may be thrombocytosis
iron studies (serum iron, serum ferritin, total iron binding capacity [TIBC], transferrin saturation)
Test
Patients should undergo serum iron studies.[71][72]
Patients with inflammatory bowel disease who are malnourished or at risk of malnutrition should have relevant screening blood tests to assess for macronutrient and micronutrient deficiencies.[70]
Iron deficiency may be associated with gastrointestinal bleeding or malabsorption of iron.
Result
normal, or may demonstrate changes consistent with iron deficiency
serum vitamin B12
Test
B12 levels should be checked.[70]
Deficiency may be secondary to malabsorption. Patients with inflammatory bowel disease who are malnourished or at risk of malnutrition should have relevant screening blood tests to assess for macronutrient and micronutrient deficiencies.[70]
Deficiency most common in ileocaecal Crohn's disease and post-ileocaecal resection.
Result
may be normal or low
serum folate
Test
Serum folate levels should be checked.[70]
Deficiency may be secondary to malabsorption. Patients with inflammatory bowel disease who are malnourished or at risk of malnutrition should have relevant screening blood tests to assess for macronutrient and micronutrient deficiencies.[70]
Result
may be normal or low
comprehensive metabolic panel (CMP)
Test
All patients should have a CMP on initial presentation.
Hypomagnesaemia and hypophosphataemia can be caused by diarrhoea and hypoprothrombinaemia may reflect vitamin K deficiency.
Result
hypoalbuminaemia, hypocholesterolaemia, hypocalcaemia
CRP and erythrocyte sedimentation rate (ESR)
Test
All patients should have CRP and ESR on initial presentation.[70][71]
Inflammatory markers correlate closely with the activity of Crohn's disease (CD).[93]
In patients with CD with moderate to severe symptoms, elevated faecal calprotectin or serum CRP suggests endoscopic activity and endoscopic evaluation can be avoided.[66]
Result
elevated
stool testing
Test
Testing for Clostridium difficile toxin is indicated especially if history of recent antibiotic use, as C difficile infection is associated with increased short- and long-term mortality in patients with inflammatory bowel disease.[9][73]
Result
absence of infectious elements seen on microscopy or culture
Yersinia enterocolitica serology
Test
Important to exclude Y enterocolitica, a bowel pathogen that causes an acute ileitis.[74] May be ordered in the acute setting.
Result
negative
plain abdominal x-ray
Test
Plain abdominal x-rays may be part of the initial tests ordered in the acute setting. They are not diagnostic of Crohn's disease, but may be suggestive and help in assessing severity. Bowel loop distension and pneumoperitoneum may be visible.
Result
small bowel or colonic dilation; calcification; sacroiliitis; intra-abdominal abscesses
MRI abdomen/pelvis
Test
Patients who are able to tolerate oral contrast are candidates for CT enterography or magnetic resonance (MR) enterography.[75] MR enterography characteristics (sensitivity 77% to 82%, specificity 80% to 100%) are similar to those of CT enterography, but availability may be limited.[75]
MR imaging has also been shown to yield robust diagnostic accuracy in detecting fibrotic strictures, distinguishing between fibrotic and inflammatory strictures, and evaluating stricture severity in patients with Crohn's disease.[76]
Guidelines suggest that MR enterography should be the test of choice as it does not expose the patient to ionising radiation.[70][71][77][Figure caption and citation for the preceding image starts]: CT scan demonstrating thickening of the terminal ileum in a patient with Crohn's disease exacerbationProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends]. [Figure caption and citation for the preceding image starts]: CT scan demonstrating thickening of the terminal ileum in a patient with Crohn's disease exacerbationProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].
[Figure caption and citation for the preceding image starts]: CT scan demonstrating thickening of the terminal ileum in a patient with Crohn's disease exacerbationProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].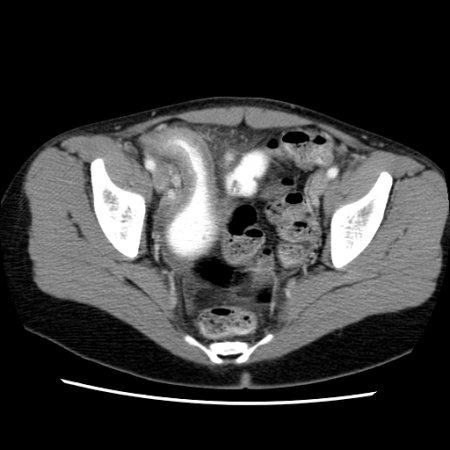
Result
skip lesions, bowel wall thickening, surrounding inflammation, abscess, fistulae
CT abdomen
Test
Patients who are able to tolerate oral contrast are candidates for CT enterography or magnetic resonance (MR) enterography.[75] CT enterography is sensitive (75% to 90%), and can assess for alternative diagnoses, and potential complications of Crohn's disease (e.g., obstruction, abscess, fistula).[75]
Guidelines suggest that MR enterography should be the test of choice as it does not expose the patient to ionising radiation.[70][71][77][Figure caption and citation for the preceding image starts]: CT scan demonstrating thickening of the terminal ileum in a patient with Crohn's disease exacerbationProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends]. [Figure caption and citation for the preceding image starts]: CT scan demonstrating thickening of the terminal ileum in a patient with Crohn's disease exacerbationProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].
[Figure caption and citation for the preceding image starts]: CT scan demonstrating thickening of the terminal ileum in a patient with Crohn's disease exacerbationProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].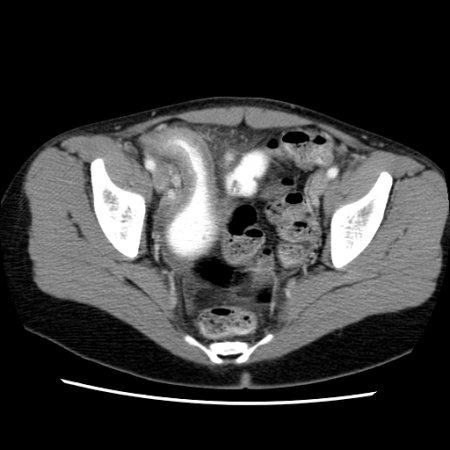
Result
skip lesions, bowel wall thickening, surrounding inflammation, abscess, fistulae
Investigations to consider
abdominal and pelvic ultrasonography
Test
Ultrasound of the abdomen and pelvis may be considered.[70][71][75]
Sensitivity and specificity range from 75% to 94% and 67% to 100%, respectively.[75] Ultrasound may facilitate detection of extramural complications, detection and evaluation of stenotic strictures, and monitoring of disease course.[71][79]
Obesity, overlying bowel gas, and guarding (in the acutely unwell patient) may preclude adequate compression of the ultrasound probe.[80]
An accuracy comparable to CT or MR modalities has been noted for visualisation of ileum when intestinal ultrasound is performed by trained practitioners.[80] Limitations of this technique include limited visualisation of the stomach, oesophagus, and rectum and inability for performing interventional procedure.[80]
Result
bowel wall thickening, surrounding inflammation, abscess; tubo-ovarian abscess
ileocolonoscopy
Test
Ileocolonoscopy and imaging studies are complementary in the diagnosis of Crohn's disease (CD).[70][71][75]
Mucosal changes suggestive of CD include mucosal nodularity, erythema, oedema, ulcerations, friability, stenosis, and the identification of fistulous tract opening.[71]
Lesions are discontinuous, with intermittent areas of normal-appearing bowel (skip lesions).[Figure caption and citation for the preceding image starts]: Endoscopic view of Crohn's ileitisProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].
Evidence of a normal rectum and isolated involvement of the terminal ileum support the diagnosis.
Result
aphthous ulcers, hyperaemia, oedema, cobblestoning, skip lesions
tissue biopsy
Test
Segmental colonic and ileal biopsies should be obtained to assess for microscopic evidence of Crohn's disease (CD).[70] The microscopic features that help distinguish ulcerative colitis and CD include granulomas, architectural change, and disease distribution.[81] Granulomatous inflammation is, however, reported in a minority of patients with CD (30% to 50%); it is not required for diagnosis.[71][81][Figure caption and citation for the preceding image starts]: Significant inflammation in the colonic wall, widening of submucosa, and dense lymphoid aggregates in the submucosaProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].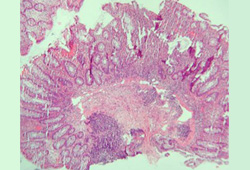 [Figure caption and citation for the preceding image starts]: Granulomas in a patient with Crohn's disease; note the aggregate of epithelioid histiocytesProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].
[Figure caption and citation for the preceding image starts]: Granulomas in a patient with Crohn's disease; note the aggregate of epithelioid histiocytesProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].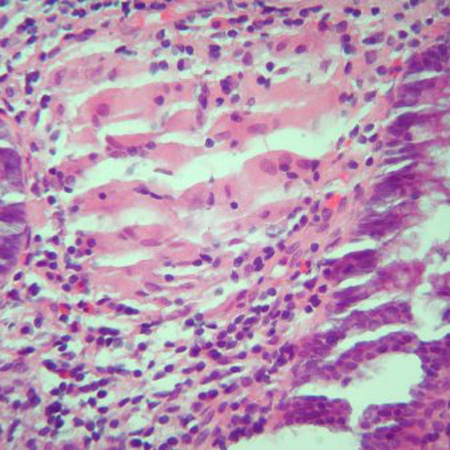 [Figure caption and citation for the preceding image starts]: Cryptitis and crypt abscess with morphological distortion of the crypts accompanied by inflammation and abundant lymphatic and plasma cellsProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].
[Figure caption and citation for the preceding image starts]: Cryptitis and crypt abscess with morphological distortion of the crypts accompanied by inflammation and abundant lymphatic and plasma cellsProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends]. [Figure caption and citation for the preceding image starts]: Cryptitis and crypt abscess with morphological distortion of the crypts accompanied by inflammation and abundant lymphatic and plasma cellsProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].
[Figure caption and citation for the preceding image starts]: Cryptitis and crypt abscess with morphological distortion of the crypts accompanied by inflammation and abundant lymphatic and plasma cellsProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].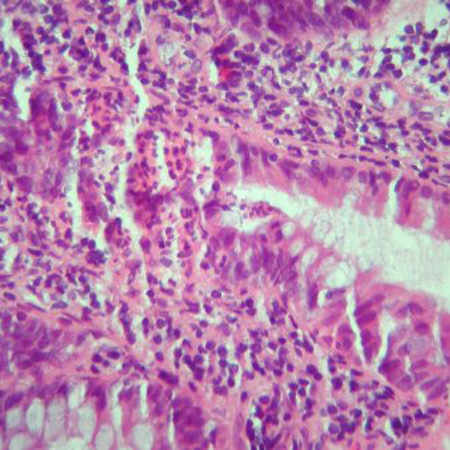
Biopsies of uninvolved mucosa help to identify the extent of histological disease.[71] If tuberculosis is being considered, tissue from ileocaecal biopsies can be tested for Mycobacterium tuberculosis.[69]
Result
mucosal bowel biopsies demonstrate transmural involvement with non-caseating granulomas
oesophagogastroduodenoscopy
Test
Oesophagogastroduodenoscopy (upper gastrointestinal [GI] endoscopy) is not routinely required as part of the diagnostic evaluation, but may be performed in patients with upper GI signs and symptoms.[70][71]
Oesophagogastroduodenoscopy with biopsy is helpful in differentiating Crohn's disease from peptic ulcer disease in patients with upper GI tract symptoms.
Result
aphthous ulcers; mucosal inflammation
wireless capsule endoscopy
Test
Can be used as an alternative to MR imaging to assess small bowel involvement. Visualises the small bowel and may detect suggestive lesions not visible by other small bowel studies. Capsule endoscopy can be used to monitor mucosal healing and postoperative recurrence in selected patients.[94] It is a safe and useful investigation in children.
Patency capsule evaluation is advised prior to endoscopy to reduce the risk of capsule retention if there is a possibility of strictures.[71] Capsule endoscopy is contraindicated in patients with small bowel strictures or stenosis.[95]
Result
aphthous ulcers; hyperaemia; oedema; cobblestoning; skip lesions
faecal calprotectin
Test
Non-invasive marker of bowel inflammation.[9][82][83] Faecal calprotectin is released into faeces when neutrophils gather at the site of any gastrointestinal tract inflammation.
In patients aged <60 years having lower gastrointestinal symptoms and normal initial work-up, faecal calprotectin testing can be performed to exclude causes of colonic inflammation. However, in patients aged >60 years with suspected colorectal cancer, faecal calprotectin testing should be interpreted with caution.[84]
Faecal calprotectin can help to differentiate inflammatory bowel disease from irritable bowel syndrome.[71] Faecal calprotectin is not specific for Crohn's disease (CD) and can be increased in the stool in other gut pathologies (e.g., infectious gastroenteritis, diverticulitis, or colorectal cancer) or in patients on non-steroidal anti-inflammatory drugs [NSAIDs] and aspirin).[71][84] This lack of specificity limits their diagnostic role.
Faecal calprotectin is widely used, particularly in the primary care setting, as a ‘rule out’ test where inflammatory bowel disease (IBD) is unlikely in the presence of a normal calprotectin.
In IBD it is used to monitor relapse in patients with quiescent IBD, and for detection and monitoring of disease activity in symptomatic patients, potentially avoiding invasive and resource-intensive endoscopic monitoring.[66][70][85][86][87] A faecal calprotectin value of <150 micrograms/g and normal CRP suggests no active inflammation in patients in symptomatic remission; endoscopic assessment can be avoided in such patients. However, elevated biomarker levels in these patients warrant an endoscopic evaluation.[66]
In patients with CD with moderate to severe symptoms, elevated faecal calprotectin or serum CRP suggests endoscopic activity and endoscopic evaluation can be avoided.[66]
Result
may be elevated
Emerging tests
serological markers
Test
Research is focused on anti-glycan antibodies (e.g., anti-Saccharomyces cerevisiae [ASCA], anti-laminaribiose [ALCA], anti-chitobioside [ACCA], anti-laminarin [anti-L], anti-chitin [anti-C]) and antibodies to microbial antigens (anti-outer membrane porin C [anti-OmpC], anti-Cbir1 flagellin, anti-I2, and p-ANCA).[71]
Anti-glycan antibodies are more prevalent in Crohn's disease (CD) than in ulcerative colitis, but have a low sensitivity.[71]
Routine use of serological markers of inflammatory bowel disease to establish the diagnosis of CD is not recommended.[71]
ASCA may be of prognostic value in children with CD.[96][97]
Result
positive anti-glycan antibodies
Use of this content is subject to our disclaimer