Approach
A history of dyspnoea, orthopnoea, paroxysmal nocturnal dyspnoea, or peripheral oedema is suggestive of mitral stenosis. Occasionally, a documented history of rheumatic fever may prompt the provider to seek a history probing for the typical symptoms.
Mitral stenosis is usually diagnosed when the characteristic diastolic murmur is heard on physical examination. This is a low-pitched, rumbling murmur that is best heard at the heart apex with the patient in the left lateral position. It may be accentuated by having the patient perform handgrip exercises.
Auscultation sounds: Mitral stenosis (severe)
Associated signs include an irregular pulse suggestive of atrial fibrillation, rales suggestive of left ventricular failure, and, in severe cases, signs of pulmonary hypertension (loud P2) and signs of right heart failure (peripheral oedema and ascites).
Investigations
Trans-thoracic echocardiography (TTE) showing typical valve deformities is the definitive test for diagnosis of mitral stenosis and should be performed on all patients with a diastolic murmur.[22][23][24][Figure caption and citation for the preceding image starts]: Short-axis view of left ventricle with flattening of the interventricular septum secondary to right ventricular pressure overloadFrom Siva A, Shah AM. Heart. 2005 Jan;91(1):e3. Used with permission [Citation ends].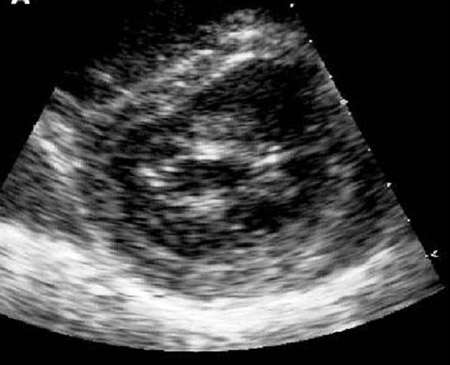 [Figure caption and citation for the preceding image starts]: Trans-thoracic echocardiogram: long-axis view of a rheumatic mitral valve showing classic doming of the leaflets in diastoleFrom Siva A, Shah AM. Heart. 2005 Jan;91(1):e3. Used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Trans-thoracic echocardiogram: long-axis view of a rheumatic mitral valve showing classic doming of the leaflets in diastoleFrom Siva A, Shah AM. Heart. 2005 Jan;91(1):e3. Used with permission [Citation ends].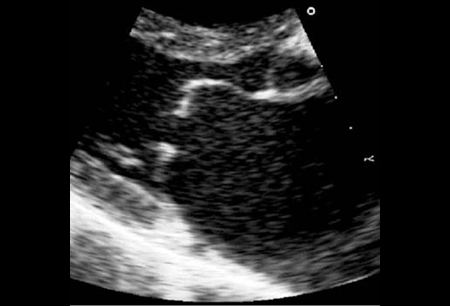
ECG and chest x-ray (CXR) should also be performed. They are non-specific for mitral stenosis but form a useful baseline of cardiac rhythm and function. ECG may reveal left atrial enlargement, right ventricular hypertrophy, and/or atrial fibrillation. CXR may show a double right heart border indicating an enlarged left atrium, a prominent pulmonary artery, and/or Kerley B lines.[Figure caption and citation for the preceding image starts]: Kerley B lines (horizontal lines in the left lower zone): a radiological change of pulmonary venous hypertensionFrom Harley HR. Br Heart J. 1961 Jan;23(1):75-87. Used with permission [Citation ends].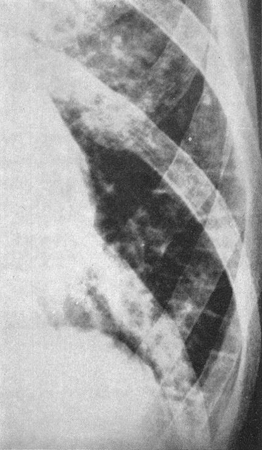
Trans-oesophageal echocardiography (TEE) is recommended if the diagnosis is unclear following TTE and also before anticipated valvotomy to examine for thrombus.[22][23] Additionally, the echocardiographic appearance of the valve in mitral annular calcification-related mitral stenosis is quite different from rheumatic mitral stenosis. The mitral leaflets are usually normal, although in some cases the basal parts of the leaflets may be calcified. There is dense calcification of the mitral annulus, encompassing part or all of the annulus. TEE may be especially helpful in assessing the extent and density of the annular calcification.[24]
Because of its invasive nature, cardiac catheterisation should be performed only in patients with echocardiogram results that are difficult to interpret and when mechanical correction is contemplated. Measurement of left atrial and left ventricular pressure and cardiac output are entered into the Gorlin formula used to calculate mitral valve area.[25][Figure caption and citation for the preceding image starts]: Gorlin formula. MVA, mitral valve area; CO, cardiac output; HR, heart rate; dfp, diastolic filling period (seconds); p1-p2, mean mitral gradient [Citation ends].
Dynamic exercise testing
For patients who fail to receive adequate relief from diuretics or when exercise-induced symptoms seem out of proportion to stenosis severity, haemodynamics should be measured at rest and with exercise either with echocardiography or cardiac catheterisation to determine if surgical intervention is required.
Use of this content is subject to our disclaimer
