Patients with chest pain can be triaged according to whether the aetiology is traumatic or atraumatic. The evaluation of atraumatic chest pain requires an algorithmic approach that first excludes acute myocardial ischaemia before working through the various aetiologies of chest pain. It is important to check whether the patient still has pain, and if not, to find out when his or her last episode of pain occurred.[24]National Institute for Health and Care Excellence. Recent-onset chest pain of suspected cardiac origin: assessment and diagnosis. Nov 2016 [internet publication].
https://www.nice.org.uk/guidance/cg95
History
The character of chest pain can help differentiate between cardiac, respiratory, musculoskeletal, and other causes. The type, severity, location, and duration of pain; the presence of any radiation; and exacerbating or relieving factors may be helpful in pointing towards a diagnosis.[16]Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2021 Nov 30;144(22):e368-454.
https://www.ahajournals.org/doi/abs/10.1161/CIR.0000000000001029
http://www.ncbi.nlm.nih.gov/pubmed/34709879?tool=bestpractice.com
Clinical presentation alone cannot reliably determine acute coronary syndrome (ACS).[49]Swap CJ, Nagurney JT. Value and limitations of chest pain history in the evaluation of patients with suspected acute coronary syndromes. JAMA. 2005 Nov 23;294(20):2623-9.
http://jamanetwork.com/journals/jama/fullarticle/201900
http://www.ncbi.nlm.nih.gov/pubmed/16304077?tool=bestpractice.com
[50]Carlton EW, Than M, Cullen L, et al. 'Chest pain typicality' in suspected acute coronary syndromes and the impact of clinical experience. Am J Med. 2015 Oct;128(10):1109-16.e2.
http://www.amjmed.com/article/S0002-9343(15)00360-5/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/25912206?tool=bestpractice.com
Certain characteristics of chest pain can give clues to the origin.
Constricting pain may be due to cardiac ischaemia or oesophageal spasm.
Pain that lasts over 15 minutes and is dull, central, and crushing is a feature of ACS.
Pain that radiates to the jaw or upper extremities suggests a cardiac cause.[51]Fanaroff AC, Rymer JA, Goldstein SA, et al. Does this patient with chest pain have acute coronary syndrome? The rational clinical examination systematic review. JAMA. 2015 Nov 10;314(18):1955-65.
http://www.ncbi.nlm.nih.gov/pubmed/26547467?tool=bestpractice.com
Pain that is new in onset, or a change to the usual pattern in a patient with previously stable angina, including recurrent episodes occurring frequently with little or no exertion, or lasting longer than 15 minutes, suggests possible ACS.[24]National Institute for Health and Care Excellence. Recent-onset chest pain of suspected cardiac origin: assessment and diagnosis. Nov 2016 [internet publication].
https://www.nice.org.uk/guidance/cg95
Sharp pleuritic pain that catches on inspiration may originate from the pleura or pericardium and suggests pneumonia, pulmonary embolus, or pericarditis.
A sudden substernal tearing pain that radiates towards the back is the classic presentation of aortic dissection.
Precipitating and relieving factors can help distinguish between cardiac and gastrointestinal causes (e.g., GORD, peptic ulcer disease, oesophageal spasm). Cardiac pain is more likely to be brought on by exercise or emotion and is typically relieved with rest or nitrates. However, response to glyceryl trinitrate should not be used to make a diagnosis.[24]National Institute for Health and Care Excellence. Recent-onset chest pain of suspected cardiac origin: assessment and diagnosis. Nov 2016 [internet publication].
https://www.nice.org.uk/guidance/cg95
Pain brought on by food, lying down, hot drinks, or alcohol, and relieved by antacids suggests a gastrointestinal cause. Heartburn and acid regurgitation are typical symptoms of GORD.[52]Katz PO, Dunbar KB, Schnoll-Sussman FH, et al. ACG clinical guideline for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 2022 Jan 1;117(1):27-56.
https://www.doi.org/10.14309/ajg.0000000000001538
http://www.ncbi.nlm.nih.gov/pubmed/34807007?tool=bestpractice.com
Abdominal pathology, such as acute cholecystitis and pancreatitis, may also cause pain referred to the chest. Associated symptoms may help to narrow the diagnosis. Acute cholecystitis may cause symptoms of fever, nausea, vomiting, persistent severe right upper quadrant pain, and jaundice. Acute pancreatitis pain is typically sudden in onset, constant, may radiate to the back, and worsens with movement. The onset of pain is sudden and is associated with vomiting in 80% of cases.[53]Johnson CD, Besselink MG, Carter R. Acute pancreatitis. BMJ. 2014 Aug 12;349:g4859.
http://www.ncbi.nlm.nih.gov/pubmed/25116169?tool=bestpractice.com
Dyspnoea is an associated symptom in patients with cardiac ischaemia, pulmonary embolism (PE), pneumothorax, or pneumonia. Nausea, vomiting, and sweating may be seen in patients with ACS.
Some patients with ACS may present with atypical symptoms: pre-syncope/syncope, nausea and vomiting, or dyspnea in the absence of chest pain. This occurs more commonly in women, people with diabetes, and those aged 75 years or more.[16]Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2021 Nov 30;144(22):e368-454.
https://www.ahajournals.org/doi/abs/10.1161/CIR.0000000000001029
http://www.ncbi.nlm.nih.gov/pubmed/34709879?tool=bestpractice.com
[54]Brieger D, Eagle KA, Goodman SG, et al; GRACE Investigators. Acute coronary syndromes without chest pain, an underdiagnosed and undertreated high-risk group: insights from the Global Registry of Acute Coronary Events. Chest. 2004 Aug;126(2):461-9.
http://www.ncbi.nlm.nih.gov/pubmed/15302732?tool=bestpractice.com
[55]Rich MW. Epidemiology, clinical features, and prognosis of acute myocardial infarction in the elderly. Am J Geriatr Cardiol. 2006 Jan-Feb;15(1):7-11; quiz 12.
http://www.ncbi.nlm.nih.gov/pubmed/16415640?tool=bestpractice.com
[56]Bayer AJ, Chadha JS, Farag PR, et al. Changing presentation of myocardial infarction with increasing old age. J Am Geriatr Soc. 1986 Apr;34(4):263-6.
http://www.ncbi.nlm.nih.gov/pubmed/3950299?tool=bestpractice.com
[57]Jacoby RM, Nesto RW. Acute myocardial infarction in the diabetic patient: pathophysiology, clinical course and prognosis. J Am Coll Cardiol. 1992 Sep;20(3):736-44.
http://www.onlinejacc.org/content/20/3/736
http://www.ncbi.nlm.nih.gov/pubmed/1512357?tool=bestpractice.com
[58]McSweeney JC, Cody M, O'Sullivan P, et al. Women's early warning symptoms of acute myocardial infarction. Circulation. 2003 Nov 25;108(21):2619-23.
http://circ.ahajournals.org/content/108/21/2619.long
http://www.ncbi.nlm.nih.gov/pubmed/14597589?tool=bestpractice.com
[59]DeVon HA, Pettey CM, Vuckovic KM, et al. A review of the literature on cardiac symptoms in older and younger women. J Obstet Gynecol Neonatal Nurs. 2016 May-Jun;45(3):426-37.
http://www.ncbi.nlm.nih.gov/pubmed/26968243?tool=bestpractice.com
[60]Sörensen NA, Neumann JT, Ojeda F, et al. Relations of sex to diagnosis and outcomes in acute coronary syndrome. J Am Heart Assoc. 2018 Mar 10;7(6):e007297.
https://www.doi.org/10.1161/JAHA.117.007297
http://www.ncbi.nlm.nih.gov/pubmed/29525782?tool=bestpractice.com
Past medical history and specific cardiac risk factors, such as known cardiac disease, elevated cholesterol, hypertension, smoking, and family history, support a cardiac cause.[61]National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III): final report. Circulation. 2002 Dec 17;106(25):3143-421.
http://circ.ahajournals.org/content/106/25/3143.short
http://www.ncbi.nlm.nih.gov/pubmed/12485966?tool=bestpractice.com
In women, pre-eclampsia, gestational diabetes, polycystic ovary syndrome, early menopause and autoimmune diseases increase the risk of cardiovascular disease.[62]Young L, Cho L. Unique cardiovascular risk factors in women. Heart. 2019 Nov;105(21):1656-60.
https://www.doi.org/10.1136/heartjnl-2018-314268
http://www.ncbi.nlm.nih.gov/pubmed/31315936?tool=bestpractice.com
It is helpful to determine if the patient has had any previous investigations or treatment for chest pain.[24]National Institute for Health and Care Excellence. Recent-onset chest pain of suspected cardiac origin: assessment and diagnosis. Nov 2016 [internet publication].
https://www.nice.org.uk/guidance/cg95
A detailed drug history, prescribed and illicit, should be taken. Use of non-steroidal anti-inflammatory drugs may result in a gastric cause of pain due to gastritis, gastric ulcer, or duodenitis. Cocaine use makes cardiac ischaemia more likely.[16]Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2021 Nov 30;144(22):e368-454.
https://www.ahajournals.org/doi/abs/10.1161/CIR.0000000000001029
http://www.ncbi.nlm.nih.gov/pubmed/34709879?tool=bestpractice.com
[63]McCord J, Jneid H, Hollander JE, et al; American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology. Management of cocaine-associated chest pain and myocardial infarction: a scientific statement from the American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology. Circulation. 2008 Apr 8;117(14):1897-907.
http://circ.ahajournals.org/content/117/14/1897.full
http://www.ncbi.nlm.nih.gov/pubmed/18347214?tool=bestpractice.com
Physical examination
Physical examination can further narrow down the differential.
Patients with chest pain may present in acute shock, such as those with:
Findings revealed in the cardiac examination include abnormalities in pulse or heart sounds (e.g., new onset of aortic stenosis, mitral regurgitation, or worsening of existing murmur, pericardial friction rub), hypo- or hypertension, and signs of heart failure.
Cardiac examination is often normal in ACS.
Aortic dissection may cause a pulse deficit, indicated by reduced pulse force or volume, or clinical signs of hypoperfusion (e.g., cold, blue, mottled limb) affecting the extremities.[64]Um SW, Ohle R, Perry JJ. Bilateral blood pressure differential as a clinical marker for acute aortic dissection in the emergency department. Emerg Med J. 2018 Sep;35(9):556-8.
http://www.ncbi.nlm.nih.gov/pubmed/30021832?tool=bestpractice.com
This is particularly common in a proximal dissection affecting the aortic arch, and may be unilateral or bilateral. Interarm systolic blood pressure differences of more than 20 mmHg may be present with aortic dissection; however, this may also be an incidental finding in hypertensive individuals without aortic dissection.[65]Pesola GR, Pesola HR, Lin M, et al. The normal difference in bilateral indirect blood pressure recordings in hypertensive individuals. Acad Emerg Med. 2002 Apr;9(4):342-5.
https://onlinelibrary.wiley.com/doi/abs/10.1197/aemj.9.4.342
http://www.ncbi.nlm.nih.gov/pubmed/11927464?tool=bestpractice.com
[66]Bautz B, Schneider JI. High-risk chief complaints I: chest pain-the big three (an update). Emerg Med Clin North Am. 2020 May;38(2):453-98.
http://www.ncbi.nlm.nih.gov/pubmed/32336336?tool=bestpractice.com
Crepitations on auscultation in one or both bases suggest pneumonia or heart failure. Reduced breath sounds on one side can be caused by a pneumothorax, or focally due to a collapsed lobe.
Tenderness on palpation over the area of chest pain usually indicates a musculoskeletal cause, such as costochondritis. However, many patients with myocardial infarction also have chest wall pain on presentation.
Tenderness unilaterally, in a dermatomal distribution (with or without the typical rash), may be indicative of herpes zoster. The pain typically presents 2 to 3 days before the development of a rash in the affected dermatome. However, some patients present with pain for up to 28 days before development of a rash.[67]Gross GE, Eisert L, Doerr HW, et al. S2k guidelines for the diagnosis and treatment of herpes zoster and postherpetic neuralgia. J Dtsch Dermatol Ges. 2020 Jan;18(1):55-78.
https://onlinelibrary.wiley.com/doi/10.1111/ddg.14013
http://www.ncbi.nlm.nih.gov/pubmed/31951098?tool=bestpractice.com
Typically, the rash is vesicular on an erythematous base in a unilateral distribution of one dermatome.[Figure caption and citation for the preceding image starts]: Varicella zoster virusCourtesy of Daniel Eisen, MD; used with permission [Citation ends].
A gastrointestinal origin of chest pain is associated with a normal cardiac and respiratory examination, unless there is existing but stable comorbidity. An abnormal abdominal examination (tenderness, rebound, guarding) makes a gastrointestinal aetiology more likely. Possible disorders include: GORD, peptic ulcer disease, cholecystitis, pancreatitis, and gastritis. In acute cholecystitis, physical examination may reveal a right upper quadrant mass. A positive Murphy's sign (the examiner’s hand rests on the right costal margin and deep inspiration causes pain) has a specificity of 96% for acute cholecystitis.[68]Jain A, Mehta N, Secko M, et al. History, physical examination, laboratory testing, and emergency department ultrasonography for the diagnosis of acute cholecystitis. Acad Emerg Med. 2017 Mar;24(3):281-97.
https://www.doi.org/10.1111/acem.13132
http://www.ncbi.nlm.nih.gov/pubmed/27862628?tool=bestpractice.com
Features of a connective tissue disease such as Marfan's syndrome (tall stature, arachnodactyly, pectus excavatum, joint hypermobility, high-arched palate and narrow face) or type IV Ehlers-Danlos syndrome (translucent skin, easy bruising, small joint hypermobility) may be present in patients with aortic dissection.[39]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on clinical practice guidelines. Circulation. 2022 Dec 13;146(24):e334-482.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001106
http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com
Unilateral leg tenderness or swelling may indicate a deep vein thrombosis in patients with suspected PE.
Basic investigations
Basic observations include temperature, blood pressure, pulse, and respiratory rate. In addition, the following should be monitored, using clinical judgement on the frequency of monitoring required, until a firm diagnosis has been made.[24]National Institute for Health and Care Excellence. Recent-onset chest pain of suspected cardiac origin: assessment and diagnosis. Nov 2016 [internet publication].
https://www.nice.org.uk/guidance/cg95
Heart rhythm
Oxygen saturation by pulse oximetry
Repeated resting 12-lead ECGs
Any exacerbations of pain and/or other symptoms
Pain relief; checking that this is effective.
ECG
A 12-lead ECG is performed in most patients unless a non-cardiac diagnosis can be made with confidence (e.g., pneumothorax).[28]Writing Committee, Kontos MC, de Lemos JA, et al. 2022 ACC expert consensus decision pathway on the evaluation and disposition of acute chest pain in the emergency department: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2022 Nov 15;80(20):1925-60.
https://www.sciencedirect.com/science/article/pii/S0735109722066189?via%3Dihub
http://www.ncbi.nlm.nih.gov/pubmed/36241466?tool=bestpractice.com
The ECG should be done as soon as possible after presentation.
ST segment changes such as ST elevation or ST depression, QRS abnormalities, arrhythmias, or tachycardia or bradycardia are characteristic findings in cardiac causes. ST segment elevation, measured at the J point, >1 mm in contiguous leads, indicates ST-elevation myocardial infarction (STEMI). ST-wave depression or T wave inversion in contiguous leads may indicate coronary ischaemia. Patients with ACS may have normal or nearly normal ECGs; where there is concern for ACS, serial ECGs should be performed.[69]Stepinska J, Lettino M, Ahrens I, et al. Diagnosis and risk stratification of chest pain patients in the emergency department: focus on acute coronary syndromes. A position paper of the Acute Cardiovascular Care Association. Eur Heart J Acute Cardiovasc Care. 2020 Feb;9(1):76-89.
https://academic.oup.com/ehjacc/article/9/1/76/5933829?login=false
http://www.ncbi.nlm.nih.gov/pubmed/31958018?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: ECG showing changes of an acute inferior myocardial infarction with ST elevation in leads II, III, and aVFFrom the collection of Professor James Brown; used with permission [Citation ends].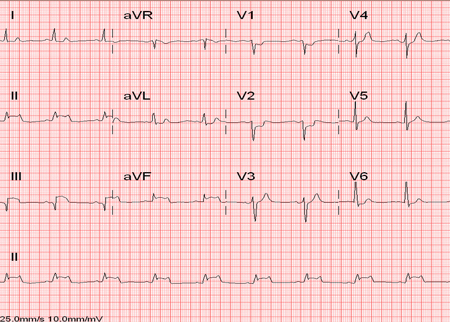 [Figure caption and citation for the preceding image starts]: ECG showing ST depressionFrom the personal collection of Dr Syed W. Yusuf and Dr Iyad N. Daher, Department of Cardiology, University of Texas, Houston, TX; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing ST depressionFrom the personal collection of Dr Syed W. Yusuf and Dr Iyad N. Daher, Department of Cardiology, University of Texas, Houston, TX; used with permission [Citation ends].
Pericarditis may be present with diffuse ST elevation or PR depression.[70]Adler Y, Charron P, Imazio M, et al; ESC Scientific Document Group. 2015 ESC guidelines for the diagnosis and management of pericardial diseases: the Task Force for the diagnosis and management of pericardial diseases of the European Society of Cardiology (ESC) endorsed by: the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2015 Nov 7;36(42):2921-64.
https://academic.oup.com/eurheartj/article/36/42/2921/2293375
http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
ECG findings that may be present in patients with PE include sinus tachycardia (most commonly) and S wave in lead I with Q wave and T wave inversion in lead III (S I, Q III, T III pattern).
Patients with pericardial tamponade may demonstrate electrical alternans (alternate-beat variation in the amplitude or axis of the QRS complex).
Chest x-ray
A chest x-ray can confirm respiratory disorders such as pneumothorax, pleural effusion, or pneumonia.
The chest x-ray is usually normal in ACS.
Chest x-ray can provide clues to another serious cardiac pathology, such as a widened mediastinum in aortic dissection, or a large globular heart in cardiac tamponade.[28]Writing Committee, Kontos MC, de Lemos JA, et al. 2022 ACC expert consensus decision pathway on the evaluation and disposition of acute chest pain in the emergency department: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2022 Nov 15;80(20):1925-60.
https://www.sciencedirect.com/science/article/pii/S0735109722066189?via%3Dihub
http://www.ncbi.nlm.nih.gov/pubmed/36241466?tool=bestpractice.com
[71]Expert Panel on Cardiac Imaging, Kicska GA, Hurwitz Koweek LM, et al. ACR Appropriateness Criteria® Suspected Acute Aortic Syndrome. J Am Coll Radiol. 2021 Nov;18(11s):S474-S481.
https://www.doi.org/10.1016/j.jacr.2021.09.004
http://www.ncbi.nlm.nih.gov/pubmed/34794601?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Chest x-ray showing a widened mediastinumFrom the collection of Professor James Brown; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Chest x-ray showing a large globular heart in a patient with pericardial tamponadeFrom the collection of Professor James Brown; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Chest x-ray showing a large globular heart in a patient with pericardial tamponadeFrom the collection of Professor James Brown; used with permission [Citation ends].
Blood tests
In patients with concern for ACS, the American College of Cardiology/American Heart Association (ACC/AHA) guidelines advocate high-sensitivity cardiac troponins as the preferred standard for establishing a biomarker diagnosis of acute myocardial infarction.[16]Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2021 Nov 30;144(22):e368-454.
https://www.ahajournals.org/doi/abs/10.1161/CIR.0000000000001029
http://www.ncbi.nlm.nih.gov/pubmed/34709879?tool=bestpractice.com
[28]Writing Committee, Kontos MC, de Lemos JA, et al. 2022 ACC expert consensus decision pathway on the evaluation and disposition of acute chest pain in the emergency department: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2022 Nov 15;80(20):1925-60.
https://www.sciencedirect.com/science/article/pii/S0735109722066189?via%3Dihub
http://www.ncbi.nlm.nih.gov/pubmed/36241466?tool=bestpractice.com
Cardiac biomarkers should be ordered on presentation; repeat measurements are made every 1-3 hours for high-sensitivity troponin assays.[16]Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2021 Nov 30;144(22):e368-454.
https://www.ahajournals.org/doi/abs/10.1161/CIR.0000000000001029
http://www.ncbi.nlm.nih.gov/pubmed/34709879?tool=bestpractice.com
High-sensitivity troponins may allow for earlier diagnosis of ACS.[72]Mueller C, Giannitsis E, Christ M, et al. Multicenter evaluation of a 0-hour/1-hour algorithm in the diagnosis of myocardial infarction with high-sensitivity cardiac troponin T. Ann Emerg Med. 2016 Jul;68(1):76-87.e4.
http://www.annemergmed.com/article/S0196-0644(15)01501-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/26794254?tool=bestpractice.com
Patients with a non-ischaemic ECG and a negative high-sensitivity troponin T, particularly if they have had pain for over 3 hours, have a very low risk of major adverse cardiac events (MACE).[69]Stepinska J, Lettino M, Ahrens I, et al. Diagnosis and risk stratification of chest pain patients in the emergency department: focus on acute coronary syndromes. A position paper of the Acute Cardiovascular Care Association. Eur Heart J Acute Cardiovasc Care. 2020 Feb;9(1):76-89.
https://academic.oup.com/ehjacc/article/9/1/76/5933829?login=false
http://www.ncbi.nlm.nih.gov/pubmed/31958018?tool=bestpractice.com
[73]National Institute for Health and Care Excellence. High-sensitivity troponin tests for the early rule out of NSTEMI. Aug 2020 [internet publication].
https://www.nice.org.uk/guidance/dg40
[74]Pickering JW, Than MP, Cullen L, et al. Rapid rule-out of acute myocardial infarction with a single high-sensitivity cardiac troponin T measurement below the limit of detection: a collaborative meta-analysis. Ann Intern Med. 2017 May 16;166(10):715-24.
http://eprints.whiterose.ac.uk/116205/1/Pickering%20Than%20MS%20AnnIntMed%20R1%20Clean%20Accepted.pdf
http://www.ncbi.nlm.nih.gov/pubmed/28418520?tool=bestpractice.com
Creatine kinase (CK) should only be used if troponin is unavailable. Biotin (vitamin B7) supplements may interfere with the results of some troponin assays, leading to falsely low results.[75]US Food and Drug Administration. Update: The FDA warns that biotin may interfere with lab tests: FDA safety communication. Nov 2019 [internet publication].
https://www.fda.gov/medical-devices/safety-communications/update-fda-warns-biotin-may-interfere-lab-tests-fda-safety-communication
In the UK, the National Institute for Health and Care Excellence recommends that high-sensitivity troponin tests should not be used in people in whom ACS is not suspected.[24]National Institute for Health and Care Excellence. Recent-onset chest pain of suspected cardiac origin: assessment and diagnosis. Nov 2016 [internet publication].
https://www.nice.org.uk/guidance/cg95
ACC/AHA guidelines state that urgent diagnostic testing for suspected coronary artery disease is not needed in low risk patients.[16]Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2021 Nov 30;144(22):e368-454.
https://www.ahajournals.org/doi/abs/10.1161/CIR.0000000000001029
http://www.ncbi.nlm.nih.gov/pubmed/34709879?tool=bestpractice.com
One cohort study of patients who presented to the emergency department with chest pain but no ACS found that any elevation of high-sensitivity troponin was associated with an increased risk of cardiovascular events and death over a mean follow-up of three years.[76]Roos A, Bandstein N, Lundbäck M,et al. Stable high-sensitivity cardiac troponin T levels and outcomes in patients with chest pain. J Am Coll Cardiol. 2017 Oct 31;70(18):2226-36.
http://www.onlinejacc.org/content/70/18/2226
http://www.ncbi.nlm.nih.gov/pubmed/29073949?tool=bestpractice.com
Another cohort study of patients who had troponin testing for any clinical reason found that any elevation of troponin was associated with a clinically significant increase in mortality, regardless of age.[77]Kaura A, Panoulas V, Glampson B, et al. Association of troponin level and age with mortality in 250 000 patients: cohort study across five UK acute care centres. BMJ. 2019 Nov 20;367:l6055.
https://www.doi.org/10.1136/bmj.l6055
http://www.ncbi.nlm.nih.gov/pubmed/31748235?tool=bestpractice.com
A full blood count should be considered to screen for anaemia and evidence of infection.
A renal profile is useful as a baseline test. Patients with impaired renal function frequently have elevated high-sensitivity troponin levels.[78]Gallacher PJ, Miller-Hodges E, Shah ASV, et al. Use of high-sensitivity cardiac troponin in patients with kidney impairment: a randomized clinical trial. JAMA Intern Med. 2021 Sep 1;181(9):1237-9.
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2780749
http://www.ncbi.nlm.nih.gov/pubmed/34096969?tool=bestpractice.com
[79]Hertzberg D, Holzmann MJ, Than M, et al. Acute kidney injury in patients presenting with chest pain to the emergency department, a descriptive study of the most common discharge diagnoses and mortality. Eur J Emerg Med. 2019 Aug;26(4):242-248.
https://www.doi.org/10.1097/MEJ.0000000000000552
http://www.ncbi.nlm.nih.gov/pubmed/29878922?tool=bestpractice.com
Patients with impaired renal function and elevated troponins are at increased risk for major cardiac events.[16]Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2021 Nov 30;144(22):e368-454.
https://www.ahajournals.org/doi/abs/10.1161/CIR.0000000000001029
http://www.ncbi.nlm.nih.gov/pubmed/34709879?tool=bestpractice.com
[80]Miller-Hodges E, Anand A, Shah ASV, et al. High-sensitivity cardiac troponin and the risk stratification of patients with renal impairment presenting with suspected acute coronary syndrome. Circulation. 2018 Jan 30;137(5):425-35.
https://www.ahajournals.org/doi/full/10.1161/CIRCULATIONAHA.117.030320
http://www.ncbi.nlm.nih.gov/pubmed/28978551?tool=bestpractice.com
Some of the differential diagnoses for chest pain can be excluded or confirmed after history, physical examination, and basic investigations have been carried out. These include STEMI, pneumothorax, pneumonia, pericarditis, and costochondritis.
Coronary angiography with percutaneous coronary intervention (PCI)
Coronary angiography with PCI is required urgently in patients with STEMI and in patients with NSTEMI who have high-risk features such as ongoing chest pain and dynamic ECG changes.[Figure caption and citation for the preceding image starts]: Angiogram showing occluded right arteryFrom the personal collection of Dr Mahi Ashwath; used with permission [Citation ends].
If PCI is unavailable or delayed more than 2 hours, then systemic fibrinolysis should be given for STEMI. Fibrinolytic therapy is not indicated in patients with NSTEMI.[23]Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014 Dec 23;130(25):e344-426.
http://circ.ahajournals.org/content/130/25/e344.long
http://www.ncbi.nlm.nih.gov/pubmed/25249585?tool=bestpractice.com
Risk stratification
The HEART score has been developed for risk stratification of patients in the emergency department. Patients with a low HEART score (0-3) have a low risk of MACE at 6 weeks. Patients with a high HEART score (7-10) are at significant risk for MACE.[51]Fanaroff AC, Rymer JA, Goldstein SA, et al. Does this patient with chest pain have acute coronary syndrome? The rational clinical examination systematic review. JAMA. 2015 Nov 10;314(18):1955-65.
http://www.ncbi.nlm.nih.gov/pubmed/26547467?tool=bestpractice.com
[81]Backus BE, Six AJ, Kelder JC, et al. A prospective validation of the HEART score for chest pain patients at the emergency department. Int J Cardiol. 2013 Oct 3;168(3):2153-8.
http://www.internationaljournalofcardiology.com/article/S0167-5273(13)00315-X/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/23465250?tool=bestpractice.com
[82]Poldervaart JM, Reitsma JB, Backus BE, et al. Effect of using the HEART score in patients with chest pain in the emergency department: a stepped-wedge, cluster randomized trial. Ann Intern Med. 2017 May 16;166(10):689-97.
http://www.ncbi.nlm.nih.gov/pubmed/28437795?tool=bestpractice.com
Systematic reviews and meta-analyses have found that the HEART score has a sensitivity of over 95% for predicting major adverse cardiac events.[83]Van Den Berg P, Body R. The HEART score for early rule out of acute coronary syndromes in the emergency department: a systematic review and meta-analysis. Eur Heart J Acute Cardiovasc Care. 2018 Mar;7(2):111-9.
http://www.ncbi.nlm.nih.gov/pubmed/28534694?tool=bestpractice.com
[84]Fernando SM, Tran A, Cheng W, et al. Prognostic accuracy of the HEART score for prediction of major adverse cardiac events in patients presenting with chest pain: a systematic review and meta-analysis. Acad Emerg Med. 2019 Feb;26(2):140-151.
https://www.doi.org/10.1111/acem.13649
http://www.ncbi.nlm.nih.gov/pubmed/30375097?tool=bestpractice.com
[85]Laureano-Phillips J, Robinson RD, Aryal S, et al. HEART score risk stratification of low-risk chest pain patients in the emergency department: a systematic review and meta-analysis. Ann Emerg Med. 2019 Aug;74(2):187-203.
https://www.doi.org/10.1016/j.annemergmed.2018.12.010
http://www.ncbi.nlm.nih.gov/pubmed/30718010?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Composition of the HEART score for chest pain patients in the emergency departmentSix AJ, et al. Neth Heart J. 2008;16:191-6; used with permission [Citation ends].
There are many other risk scores available. Guidelines vary in their recommendations on risk stratification in people presenting with acute chest pain to the accident and emergency department.[28]Writing Committee, Kontos MC, de Lemos JA, et al. 2022 ACC expert consensus decision pathway on the evaluation and disposition of acute chest pain in the emergency department: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2022 Nov 15;80(20):1925-60.
https://www.sciencedirect.com/science/article/pii/S0735109722066189?via%3Dihub
http://www.ncbi.nlm.nih.gov/pubmed/36241466?tool=bestpractice.com
[86]American College of Cardiology. The use of chest pain scores and high-sensitivity troponin for evaluating chest pain patients. May 2016 [internet publication].
http://www.acc.org/latest-in-cardiology/articles/2016/03/18/08/28/the-use-of-chest-pain-scores-and-high-sensitivity-troponin
[69]Stepinska J, Lettino M, Ahrens I, et al. Diagnosis and risk stratification of chest pain patients in the emergency department: focus on acute coronary syndromes. A position paper of the Acute Cardiovascular Care Association. Eur Heart J Acute Cardiovasc Care. 2020 Feb;9(1):76-89.
https://academic.oup.com/ehjacc/article/9/1/76/5933829?login=false
http://www.ncbi.nlm.nih.gov/pubmed/31958018?tool=bestpractice.com
Further investigations
Some patients need further investigations to confirm the suspected diagnosis.
Evaluating risk of angina and coronary artery disease
Once ACS, ventricular arrhythmias, and haemodynamic instability are excluded, patients with chest pain that is clinically considered to be ischaemic in origin can be stratified by their likelihood of having angina and risk for coronary artery disease (CAD).[87]American College of Radiology. ACR appropriateness criteria: chest pain - possible acute coronary syndrome. 2019 [internet publication].
https://acsearch.acr.org/docs/69403/Narrative
[88]Multimodality Writing Group for Chronic Coronary Disease, Winchester DE, Maron DJ, et al. ACC/AHA/ASE/ASNC/ASPC/HFSA/HRS/SCAI/SCCT/SCMR/STS 2023 Multimodality appropriate use criteria for the detection and risk assessment of chronic coronary disease. J Am Coll Cardiol. 2023 Jun 27;81(25):2445-67.[89]Morise AP, Haddad WJ, Beckner D. Development and validation of a clinical score to estimate the probability of coronary artery disease in men and women presenting with suspected coronary disease. Am J Med. 1997 Apr;102(4):350-6.
http://www.ncbi.nlm.nih.gov/pubmed/9217616?tool=bestpractice.com
[90]Pryor DB, Shaw L, McCants CB, et al. Value of the history and physical in identifying patients at increased risk for coronary artery disease. Ann Intern Med. 1993 Jan 15;118(2):81-90.
http://www.ncbi.nlm.nih.gov/pubmed/8416322?tool=bestpractice.com
[91]Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med. 1979 Jun 14;300(24):1350-8.
http://www.ncbi.nlm.nih.gov/pubmed/440357?tool=bestpractice.com
[92]Pryor DB, Harrell FE Jr., Lee KL, et al. Estimating the likelihood of significant coronary artery disease. Am J Med. 1983 Nov;75(5):771-80.
http://www.ncbi.nlm.nih.gov/pubmed/6638047?tool=bestpractice.com
Patients who are at intermediate to high pre-test risk of obstructive coronary artery disease will benefit the most from cardiac imaging and testing.[16]Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2021 Nov 30;144(22):e368-454.
https://www.ahajournals.org/doi/abs/10.1161/CIR.0000000000001029
http://www.ncbi.nlm.nih.gov/pubmed/34709879?tool=bestpractice.com
High pre-test probability of CAD (>90%): should be referred for coronary angiography.[93]Expert Panel on Cardiac Imaging, Akers SR, Panchal V, et al. ACR Appropriateness Criteria® Chronic Chest Pain-High Probability of Coronary Artery Disease. J Am Coll Radiol. 2017 May;14(5s):S71-S80.
https://www.doi.org/10.1016/j.jacr.2017.01.034
http://www.ncbi.nlm.nih.gov/pubmed/28473096?tool=bestpractice.com
Fractional flow reserve (FFR) CT is being increasingly used to clarify the functional significance of stenoses, particularly when intervention is being considered without prior functional testing. FFRCT is a non-invasive, post-processing image analysis technique that allows assessment of flow limitation across coronary stenoses by using data derived from routine diagnostic coronary computed tomography (CT) angiography studies.[94]Pontone G, Baggiano A, Andreini D, et al. Stress computed tomography perfusion versus fractional flow reserve CT derived in suspected coronary artery disease: the PERFECTION study. JACC Cardiovasc Imaging. 2019 Aug;12(8 pt 1):1487-97.
https://www.doi.org/10.1016/j.jcmg.2018.08.023
http://www.ncbi.nlm.nih.gov/pubmed/30343073?tool=bestpractice.com
[95]NHS England. 3D heart scans on the NHS to speed up disease diagnosis. May 2021 [internet publication].
https://www.england.nhs.uk/2021/05/3d-heart-scans-on-the-nhs-to-speed-up-disease-diagnosis
Intermediate pre-test probability of CAD (10-90%): should have stress testing with imaging (radionuclide, echocardiography, or magnetic resonance imaging) or coronary CT angiography.[16]Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2021 Nov 30;144(22):e368-454.
https://www.ahajournals.org/doi/abs/10.1161/CIR.0000000000001029
http://www.ncbi.nlm.nih.gov/pubmed/34709879?tool=bestpractice.com
Low pre-test probability of CAD (<10%): if the patient has an interpretable ECG (not left bundle branch block, pre-excitation [Wolff-Parkinson-White], or ventricular paced rhythm) and is able to exercise, he or she should have an exercise stress test. Otherwise the patient should have a stress test with imaging.[87]American College of Radiology. ACR appropriateness criteria: chest pain - possible acute coronary syndrome. 2019 [internet publication].
https://acsearch.acr.org/docs/69403/Narrative
Guidelines differ in their recommendations on use of risk stratification and further specific investigations so it's important to check local protocols.
Patients without symptoms of angina should be evaluated for alternative causes of chest pain.
Transthoracic echocardiography is a non-invasive way of assessing cardiac function. It is necessary if cardiac tamponade is suspected and is helpful in confirming a diagnosis of pulmonary hypertension, pericarditis, aortic stenosis, and mitral valve prolapse.[96]National Institute for Health and Care Excellence. Heart valve disease presenting in adults: investigation and management. Nov 2021 [internet publication].
https://www.nice.org.uk/guidance/ng208
Laboratory studies for suspected aortic pathology
CT angiography allows rapid imaging and detection of life-threatening aortic pathology (e.g., aortic dissection).[39]Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on clinical practice guidelines. Circulation. 2022 Dec 13;146(24):e334-482.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001106
http://www.ncbi.nlm.nih.gov/pubmed/36322642?tool=bestpractice.com
Magnetic resonance aortography has a sensitivity and specificity equivalent to CT. This imaging modality also provides information on aortic valve pathology and left ventricular function, but the images take longer to acquire so it is only suitable for haemodynamically stable patients.[97]Guichard JL, Hage FG. Guidelines in review: 2015 ACR/ACC/AHA/AATS/ACEP/ASNC/NASCI/SAEM/SCCT/SCMR/SCPC/SNMMI/STR/STS appropriate utilization of cardiovascular imaging in emergency department patients with chest pain: a joint document of the American College of Radiology Appropriateness Criteria Committee and the American College of Cardiology Appropriate Use Criteria Task Force. J Nucl Cardiol. 2016 Oct;23(5):1142-6.
http://www.ncbi.nlm.nih.gov/pubmed/27000877?tool=bestpractice.com
A trans-oesophageal echocardiogram is an alternative if a dissection-skilled operator is readily available.[71]Expert Panel on Cardiac Imaging, Kicska GA, Hurwitz Koweek LM, et al. ACR Appropriateness Criteria® Suspected Acute Aortic Syndrome. J Am Coll Radiol. 2021 Nov;18(11s):S474-S481.
https://www.doi.org/10.1016/j.jacr.2021.09.004
http://www.ncbi.nlm.nih.gov/pubmed/34794601?tool=bestpractice.com
Assessing probability of pulmonary embolism
If there is low clinical suspicion of PE, and the patient satisfies the Pulmonary Embolism Rule-Out Criteria (the PERC rule), the risk of PE is considered to be lower than the risk of testing.[98]Raja AS, Greenberg JO, Qaseem A, et al. Evaluation of patients with suspected acute pulmonary embolism: best practice advice from the Clinical Guidelines Committee of the American College of Physicians. Ann Intern Med. 2015 Nov 3;163(9):701-11.
http://annals.org/aim/article/2443959/evaluation-patients-suspected-acute-pulmonary-embolism-best-practice-advice-from
http://www.ncbi.nlm.nih.gov/pubmed/26414967?tool=bestpractice.com
[99]Penaloza A, Soulié C, Moumneh T, et al. Pulmonary embolism rule-out criteria (PERC) rule in European patients with low implicit clinical probability (PERCEPIC): a multicentre, prospective, observational study. Lancet Haematol. 2017 Dec;4(12):e615-21.
http://www.ncbi.nlm.nih.gov/pubmed/29150390?tool=bestpractice.com
[100]Freund Y, Cachanado M, Aubry A, et al; PROPER Investigator Group. Effect of the Pulmonary Embolism Rule-Out Criteria on subsequent thromboembolic events among low-risk emergency department patients: The PROPER randomized clinical trial. JAMA. 2018 Feb 13;319(6):559-66.
http://www.ncbi.nlm.nih.gov/pubmed/29450523?tool=bestpractice.com
[101]National Institute for Health and Care Excellence. Venous thromboembolic diseases: diagnosis, management and thrombophilia testing. Aug 2023 [internet publication].
https://www.nice.org.uk/guidance/ng158
If there is high clinical suspicion of PE, or the patient does not satisfy the PERC rule, the Wells (or Geneva) Score may be used to categorise the patient as:
‘PE likely’ (Wells Score >4); D-dimer testing is not recommended because a negative result will not remove the need for definitive laboratory (usually computed tomographic pulmonary angiography [CTPA] if available)[98]Raja AS, Greenberg JO, Qaseem A, et al. Evaluation of patients with suspected acute pulmonary embolism: best practice advice from the Clinical Guidelines Committee of the American College of Physicians. Ann Intern Med. 2015 Nov 3;163(9):701-11.
http://annals.org/aim/article/2443959/evaluation-patients-suspected-acute-pulmonary-embolism-best-practice-advice-from
http://www.ncbi.nlm.nih.gov/pubmed/26414967?tool=bestpractice.com
[101]National Institute for Health and Care Excellence. Venous thromboembolic diseases: diagnosis, management and thrombophilia testing. Aug 2023 [internet publication].
https://www.nice.org.uk/guidance/ng158
‘PE unlikely’ (Wells Score ≤4); D-dimer test is ordered.[101]National Institute for Health and Care Excellence. Venous thromboembolic diseases: diagnosis, management and thrombophilia testing. Aug 2023 [internet publication].
https://www.nice.org.uk/guidance/ng158
A normal plasma D-dimer level safely excludes PE in patients with an unlikely pre-test probability of PE and no further investigation is required.[98]Raja AS, Greenberg JO, Qaseem A, et al. Evaluation of patients with suspected acute pulmonary embolism: best practice advice from the Clinical Guidelines Committee of the American College of Physicians. Ann Intern Med. 2015 Nov 3;163(9):701-11.
http://annals.org/aim/article/2443959/evaluation-patients-suspected-acute-pulmonary-embolism-best-practice-advice-from
http://www.ncbi.nlm.nih.gov/pubmed/26414967?tool=bestpractice.com
D-dimer blood testing by enzyme-linked immunosorbent assay (ELISA) has a sensitivity and negative predictive value >95%, regardless of the calculated clinical probability, making it useful to rule out the presence of venous thromboembolism. However, specificity is much lower, with estimates from 23% to 63%. It is particularly useful in patients with a low clinical probability assessment.[102]Righini M, Perrier A, De Moerloose P, et al. D-dimer for venous thromboembolism diagnosis: 20 years later. J Thromb Haemost. 2008 Jul;6(7):1059-71.
http://onlinelibrary.wiley.com/doi/10.1111/j.1538-7836.2008.02981.x/full
http://www.ncbi.nlm.nih.gov/pubmed/18419743?tool=bestpractice.com
[103]Dunn KL, Wolf JP, Dorfman DM, et al. Normal D-dimer levels in emergency department patients suspected of acute pulmonary embolism. J Am Coll Cardiol. 2002 Oct 16;40(8):1475-8.
http://www.onlinejacc.org/content/40/8/1475
http://www.ncbi.nlm.nih.gov/pubmed/12392839?tool=bestpractice.com
[104]Crawford F, Andras A, Welch K, et al. D-dimer test for excluding the diagnosis of pulmonary embolism. Cochrane Database Syst Rev. 2016 Aug 5;2016(8):CD010864.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010864.pub2/full
http://www.ncbi.nlm.nih.gov/pubmed/27494075?tool=bestpractice.com
There is evidence to suggest that age-adjusted D-dimer cut-offs or D-dimer testing adjusted to clinical probability may be effective, but these approaches are not in widespread clinical use.[45]Konstantinides SV, Meyer G, Becattini C, et al. 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS): the Task Force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC). Eur Respir J. 2019 Oct 9;54(3):1901647.
https://erj.ersjournals.com/content/54/3/1901647.long
http://www.ncbi.nlm.nih.gov/pubmed/31473594?tool=bestpractice.com
[105]Stals MAM, Takada T, Kraaijpoel N, et al. Safety and efficiency of diagnostic strategies for ruling out pulmonary embolism in clinically relevant patient subgroups : a systematic review and individual-patient data meta-analysis. Ann Intern Med. 2022 Feb;175(2):244-55.
http://www.ncbi.nlm.nih.gov/pubmed/34904857?tool=bestpractice.com
Point of care chest ultrasound (POCUS)
Highly specific for diagnosing pneumothorax, pleural effusion and pericardial effusion in the accident and emergency department.[106]Buhumaid RE, St-Cyr Bourque J, Shokoohi H, et al. Integrating point-of-care ultrasound in the ED evaluation of patients presenting with chest pain and shortness of breath. Am J Emerg Med. 2019 Feb;37(2):298-303.
http://www.ncbi.nlm.nih.gov/pubmed/30413369?tool=bestpractice.com
When evaluating patients with dyspnoea, POCUS has demonstrated increased sensitivity compared with chest x-ray.[107]Lamsam L, Gharahbaghian L, Lobo V. Point-of-care ultrasonography for detecting the etiology of unexplained acute respiratory and chest complaints in the emergency department: a prospective analysis. Cureus. 2018 Aug 28;10(8):e3218.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6205892
http://www.ncbi.nlm.nih.gov/pubmed/30405993?tool=bestpractice.com
POCUS decreases time to appropriate treatment in medical patients.[108]Ben-Baruch Golan Y, Sadeh R, Mizrakli Y, et al. Early point-of-care ultrasound assessment for medical patients reduces time to appropriate treatment: a pilot randomized controlled trial. Ultrasound Med Biol. 2020 Aug;46(8):1908-15.
http://www.ncbi.nlm.nih.gov/pubmed/32430108?tool=bestpractice.com
POCUS has been reported to be significantly more sensitive for the diagnosis of heart failure, but not for that of COPD/asthma or pulmonary embolism, compared with standard evaluations for these conditions.[109]Zanobetti M, Scorpiniti M, Gigli C, et al. Point-of-care ultrasonography for evaluation of acute dyspnea in the ED. Chest. 2017 Jun;151(6):1295-301.
http://www.ncbi.nlm.nih.gov/pubmed/28212836?tool=bestpractice.com
Investigations for suspected gastric aetiology
If a gastric diagnosis is the more likely cause for chest pain, then investigations such as oesophagogastroduodenoscopy, oesophageal pH monitoring, oesophageal manometry, barium swallow, and Helicobacter pylori breath test can be considered. A therapeutic trial of proton-pump inhibitors can relieve symptoms in patients with GORD, once cardiac causes of the chest pain have been ruled out.[110]Wang WH, Huang JQ, Zheng GF, et al. Is proton pump inhibitor testing an effective approach to diagnose gastroesophageal reflux disease in patients with noncardiac chest pain?: a meta-analysis. Arch Intern Med. 2005 Jun 13;165(11):1222-8.
http://jamanetwork.com/journals/jamainternalmedicine/fullarticle/486601
http://www.ncbi.nlm.nih.gov/pubmed/15956000?tool=bestpractice.com
Further blood tests such as liver profile and either serum lipase or amylase may be necessary if acute cholecystitis or acute pancreatitis is suspected.[111]Tenner S, Baillie J, DeWitt J, et al. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013 Sep;108(9):1400-15; 1416.
https://journals.lww.com/ajg/fulltext/2013/09000/american_college_of_gastroenterology_guideline_.6.aspx
http://www.ncbi.nlm.nih.gov/pubmed/23896955?tool=bestpractice.com
These diagnoses may also require further imaging such as abdominal ultrasound and abdominal CT (for acute pancreatitis).[111]Tenner S, Baillie J, DeWitt J, et al. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013 Sep;108(9):1400-15; 1416.
https://journals.lww.com/ajg/fulltext/2013/09000/american_college_of_gastroenterology_guideline_.6.aspx
http://www.ncbi.nlm.nih.gov/pubmed/23896955?tool=bestpractice.com

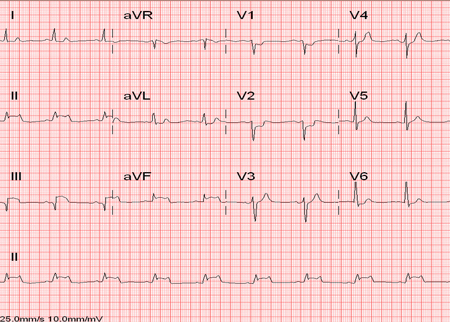 [Figure caption and citation for the preceding image starts]: ECG showing ST depressionFrom the personal collection of Dr Syed W. Yusuf and Dr Iyad N. Daher, Department of Cardiology, University of Texas, Houston, TX; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing ST depressionFrom the personal collection of Dr Syed W. Yusuf and Dr Iyad N. Daher, Department of Cardiology, University of Texas, Houston, TX; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Chest x-ray showing a large globular heart in a patient with pericardial tamponadeFrom the collection of Professor James Brown; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Chest x-ray showing a large globular heart in a patient with pericardial tamponadeFrom the collection of Professor James Brown; used with permission [Citation ends].