Recommendations
Urgent
Consider bacterial meningitis in adults with any of:[16][25]
Headache
Neck stiffness
Fever
Altered consciousness.
Recognise cardiorespiratory arrest, suspected sepsis, meningococcal disease (not covered here), and shock.[16]
These problems take priority over ‘uncomplicated’ bacterial meningitis
Follow local protocols for management
See Sepsis in adults, Meningococcal disease, and Shock.
If you suspect non-meningococcal bacterial meningitis, within 1 hour of arrival at hospital:
Assess illness severity using a validated scoring system, such as the National Early Warning Score 2 (NEWS2).[16][26] See Management Recommendations.
Arrange urgent review by a ward-based doctor or acute team nurse to assess acutely ill patients if there is an aggregate score of 5/6 (or a score of 3 in any single physiological parameter)
Call the critical care team urgently if the patient has a score of 7 or more
Do not be falsely reassured if the early warning score is lower than these parameters, because patients with meningitis can deteriorate rapidly
Seek advice from a senior clinical decision-maker (registrar or consultant) on the initial management of acute bacterial meningitis, as well as a microbiologist or infectious diseases consultant[16]
Take blood cultures, even if antibiotics have been given in the community[16]
Do a lumbar puncture (LP) to obtain cerebrospinal fluid (CSF), even if antibiotics have been given in the community[16]
Inform the lab of an urgent CSF sample, which will need confirmation of receipt and urgent processing. Tell the laboratory if the patient has received antibiotics.
Delay lumbar puncture, but DO give antibiotics if you suspect bacterial meningitis and the patient has:[16]
Shock
Sepsis or rapidly progressing rash
Severe respiratory or cardiac compromise
Confirmed/known bleeding or high risk of bleeding
Raised intracranial pressure, indicated by:
Focal neurological signs
Papilloedema
Continuous or uncontrolled seizures
Glasgow Coma Scale score ≤12. [ Glasgow Coma Scale Opens in new window ]
Perform cranial imaging before lumbar puncture if there is a risk of cerebral herniation due to conditions such as brain abscess, subdural empyema, or large cerebral infarction.[25][28][29]
This has been a controversial area.[16][30][31] Delaying LP for a computed tomography (CT) scan can cause delays in antibiotic administration, which may lead to an increase in mortality.[32][33]
In practice, most patients will have LP without the need for prior neuroimaging.[16]
The following signs suggest risk of cerebral herniation secondary to raised intracranial pressure:
Papilloedema[16]
Focal neurological deficits (excluding nerve palsies)[16][25]
Altered mental status[16][25] [ Glasgow Coma Scale Opens in new window ]
Severe immunocompromise.[25]
Regardless of decisions about pre-LP neuroimaging, delay or do NOT perform LP in the following situations:[16][25]
Respiratory or cardiac compromise
Signs of severe sepsis or a rapidly evolving rash
Infection at the site of the LP
A coagulopathy.
Key Recommendations
Initial assessment
Assess the patient using an ABCDE approach, noting in particular:[16]
Airway – signs of obstruction
Breathing – respiratory rate, oxygen saturation
Circulation – pulse, capillary refill time, urine output, blood pressure
Disability – Glasgow Coma Scale (GCS) [ Glasgow Coma Scale Opens in new window ] , focal neurological signs, seizures, papilloedema, capillary glucose
Exposure – petechial or purpuric rash (see Meningococcal disease).
Investigations
As well as taking blood for culture, take blood for:[16]
Full blood count
Urea and electrolytes, creatinine, glucose, lactate, coagulation screen, liver function tests
Polymerase chain reaction (PCR) for pneumococcus and meningococcus
Blood gases
Serum procalcitonin if available, or C-reactive protein if procalcitonin is unavailable.
Observe the cerebrospinal fluid (CSF) sample for clues to the diagnosis (see table below) and request the following investigations:[16]
Glucose (at same time as blood glucose taken)
Protein
Microscopy, culture, and sensitivities
Cell count
Lactate (if prior antibiotics have not been given)
PCR for pneumococcus and meningococcus, enterovirus, herpes simplex varicella zoster, and Mycobacterium tuberculosis.
Classic cerebrospinal fluid features of the different causes of meningitis[16] (reproduced with permission) | |||||
Normal | Bacterial | Viral | Tuberculosis | Fungal | |
Opening pressure (cm CSF) | 12 to 20 | Raised | Normal/mildly raised | Raised | Raised |
Appearance | Clear | Turbid, cloudy, purulent | Clear | Clear or cloudy | Clear or cloudy |
CSF WBC count (cells/uL) | <5 | Raised (typically >100)a | Raised (typically 5 to 1000)a | Raised (typically 5 to 500)a | Raised (typically 5 to 500)a |
Predominant cell type | n/a | Neutrophilsb | Lymphocytesc | Lymphocytesd | Lymphocytes |
CSF protein (g/L) | <0.4 | Raised | Mildly raised | Markedly raised | Raised |
CSF glucose (mmol) | 2.6 to 4.5 | Very low | Normal/slightly low | Very low | Low |
CSF/plasma glucose ratio | >0.66 | Very low | Normal/slightly low | Very low | Low |
Local laboratory ranges for biochemical tests should be consulted and may vary from those quoted here. A traumatic lumbar puncture will affect the results by falsely elevating the white cells due to excessive red cells. A common correction factor used is 1:1000. aOccasionally the CSF WBC count is normal (especially in immunodeficiency or tuberculous meningitis). bMay be lymphocytic if antibiotics given before lumbar puncture (partially treated bacterial meningitis), or with certain bacteria (e.g., Listeria monocytogenes). cMay be neutrophilic in enteroviral meningitis (especially early in disease). dMay be neutrophils early in the course of disease. | |||||
Do not obtain a nasal swab for pneumococcal disease.[16]
Do not order neuroimaging unless you need to detect alternative pathology (e.g., abscess, subdural empyema, or large cerebral infarction) if there are signs of risk of cerebral herniation.[16]
Early recognition is essential. The most common features of bacterial meningitis in adults are:[25]
Headache
Present in 87% of adults with bacterial meningitis[17]
Neck stiffness
Fever
Present in 77% of adults with bacterial meningitis[17]
Altered mental status
The classic triad of fever, neck stiffness, and altered mental status occurs in only 41% to 51% of patients.[25][35][36] However, in one study, 95% had at least two of the four symptoms of headache, fever, neck stiffness, and altered mental status.[17]
Do not exclude the diagnosis of meningitis just because classic symptoms are absent.
Assess the patient using an ABCDE approach, noting in particular:[16]
Airway – signs of obstruction
Breathing – respiratory rate, oxygen saturation
Circulation – pulse, capillary refill time, urine output, blood pressure
Disability – Glasgow Coma Scale (GCS) score, [ Glasgow Coma Scale Opens in new window ] focal neurological signs, seizures, papilloedema, capillary glucose
Exposure – petechial or purpuric rash (see Meningococcal disease).
Recognise cardiorespiratory arrest, suspected sepsis, meningococcal disease (systemic meningococcal sepsis with or without meningococcal meningitis – not covered here), and shock.[16]
These problems take priority over ‘uncomplicated’ bacterial meningitis.
Follow local protocols for management.
See Sepsis in adults, Meningococcal disease, and Shock.
Practical tip
Think 'Could this be sepsis?' based on acute deterioration in a patient in whom there is clinical evidence or strong suspicion of infection.[26][37][38]
Use a systematic approach, alongside your clinical judgement, for assessment; urgently consult a senior clinical decision-maker (e.g., ST4 level doctor in the UK) if you suspect sepsis.[37][38][39][40]
Refer to local guidelines for the recommended approach at your institution for assessment and management of the patient with suspected sepsis.
Practical tip
Meningococcal meningitis cannot be reliably clinically differentiated from bacterial meningitis caused by other bacteria before obtaining Gram stain results.[41]
A petechial rash occurs in 20% to 52% of patients with meningitis and indicates meningococcal infection in more than 90% of these patients.[17]
If the patient has a purpuric or petechial rash, hypotension, and altered mental state with or without symptoms of meningitis, consider meningococcal disease.[16] See Meningococcal disease.
If you suspect non-meningococcal bacterial meningitis, within 1 hour of arrival at hospital:
Assess illness severity using a validated scoring system, such as the National Early Warning Score 2 (NEWS2)[16][26]
Arrange urgent review by a ward-based doctor or an acute team nurse to assess acutely ill patients if there is an aggregate score of 5/6 (or a score of 3 in any single physiological parameter)
Call the critical care team urgently if the patient has a score of 7 or more
Do not be falsely reassured if the early warning score is lower than these parameters, because patients with meningitis can deteriorate rapidly
Seek advice from a senior clinical decision-maker (registrar or consultant) on the initial management of acute bacterial meningitis, as well as a microbiologist or infectious diseases consultant[16]
Be aware that the sensitivities of Brudzinski's sign and Kernig's sign (classically associated with meningitis) are so low that they are not helpful in diagnosing bacterial meningitis
The sensitivity of various signs in predicting raised white blood cell count in cerebrospinal fluid (as a marker for bacterial infection) is:[25][29]
Neck stiffness – 31%
Brudzinski's sign – 9%
Kernig's sign – 11%.
[Figure caption and citation for the preceding image starts]: National Early Warning Score 2 (NEWS2) is an early warning score produced by the Royal College of Physicians in the UK. It is based on the assessment of six individual parameters, which are assigned a score of between 0 and 3: respiratory rate, oxygen saturations, temperature, blood pressure, heart rate, and level of consciousness. There are different scales for oxygen saturation levels based on a patient’s physiological target (with scale 2 being used for patients at risk of hypercapnic respiratory failure). The score is then aggregated to give a final total score; the higher the score, the higher the risk of clinical deteriorationReproduced from: Royal College of Physicians. National Early Warning Score (NEWS) 2: Standardising the assessment of acute-illness severity in the NHS. Updated report of a working party. London: RCP, 2017. [Citation ends].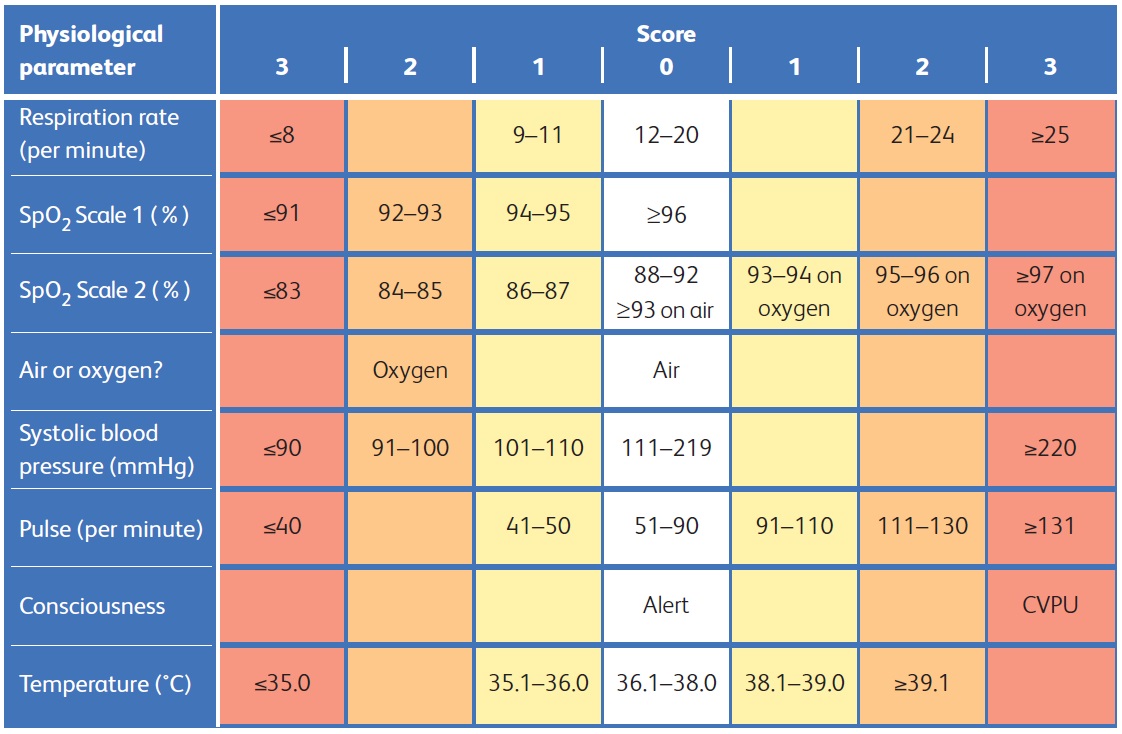
Practical tip
Tuberculous meningitis is a medical emergency, but diagnosis can be challenging. Early recognition and prompt treatment improve survival.[42][43] Features include:
1 to 2 weeks prodrome with low-grade fever, malaise, weight loss, and gradual onset of headache
Progresses to worsening headache, vomiting, confusion, and coma
Neck stiffness
III, IV, and VI cranial nerve palsies
Urinary retention
Focal neurological signs such as monoplegia, hemiplegia, and paraplegia.
About 50% of patients with bacterial meningitis have predisposing conditions, so ask about risk factors including the following.
Advanced age
Older people are more commonly affected because of impaired or waning immunity.[2]
Crowding
Ideal for bacterial transmission. Outbreaks have been reported in US college dormitories and in training camps for military recruits.[1]
Exposure to pathogens
Immunocompromising conditions
About 50% of patients with bacterial meningitis have a predisposing condition.
Includes chronic conditions such as diabetes, alcohol misuse, or eculizumab therapy.[16]
One third of patients with predisposing conditions have an immunodeficiency.[17]
Congenital immunodeficiencies, such as complement deficiencies, X-linked agammaglobulinaemia, IgG subclass deficiency, or interleukin 1 receptor-associated kinase 4 deficiency, have been associated with bacterial meningitis.[20]
Asplenia or hyposplenia increases the risk of overwhelming bacterial infections with encapsulated bacteria, particularly S pneumoniae and Haemophilus influenzae.[20]
HIV infection makes people susceptible to bacterial meningitis, particularly if they develop AIDS.
Malignancy:
Patients with leukaemia and lymphoma are susceptible to bacterial meningitis.[18]
Cranial anatomical defects, ventriculoperitoneal shunt
Cochlear implants
Recipients of cochlear implants are at higher risk of bacterial meningitis than the general population.[1]
Sickle cell disease
Patients are more likely to get meningitis due to impaired splenic function and impaired complement cascade among other mechanisms.[21]
Contiguous infection
Infections such as sinusitis, pneumonia, mastoiditis, and otitis media increase the risk of meningitis.[1]
Check for signs of raised intracranial pressure, including:
Focal neurological signs
May include dilated non-reactive pupil, abnormalities of ocular motility, abnormal visual fields, gaze palsy, arm or leg drift
Abnormal eye movement
Suggests cranial nerve palsy (III, IV, VI)
Papilloedema
An enlarged blind spot may be identified when you examine the visual fields
Facial palsy
Cranial nerve VII may be damaged due to inflammation
Balance problems or hearing impairment
Cranial nerve VIII may be damaged due to inflammation.
Note other features of meningitis including:
Vomiting
Confusion
May be the only sign in older people
Photophobia
Well-recognised symptom of bacterial meningitis[16]
Seizures
Petechial or purpuric rash
May be present with any type of bacterial meningitis
Typically associated with meningococcal meningitis
A petechial rash is identified in 20% to 52% of patients and indicates meningococcal infection in more than 90% of patients[17]
Kernig's sign
Brudzinski's sign
Blood tests
Take blood for culture within 1 hour of arrival at hospital and ideally prior to giving antibiotics to identify the causative organism and target treatment accordingly.[16]
Taking blood for culture should not delay administration of antibiotics.[16]
Take blood cultures, even if antibiotics have been given in the community.[16] It is good practice to tell the laboratory that the patient has received antibiotics.
The results of blood cultures may be influenced by previous antibiotics, however.[44]
Take blood for polymerase chain reaction (PCR) for specific bacteria.
This is especially important if antibiotics have been given prior to taking blood or performing a lumbar puncture, as PCR will remain positive for several days after antibiotics have been started.[16][45][46]
PCR amplification of bacterial DNA from blood is more sensitive and specific than traditional microbiological techniques. It is useful in distinguishing bacterial from viral meningitis.
Patients with severe bacterial meningitis often have metabolic abnormalities.[16] Always request:
Serum glucose – may show hypoglycaemia or hyperglycaemia[16]
Full blood count – may show raised white blood cell count, low red blood cell count, and low platelet count[16]
Patients with rapidly progressive infections may initially have a normal white blood cell count
Neutropenia can occur in severe infections
Serum urea, creatinine, electrolytes – may show acidosis, hypokalaemia, hypocalcaemia, and hypomagnesaemia
Low sodium may point towards tuberculous meningitis
Venous blood gas – mainly to measure lactate concentration
Liver function tests – may be raised, showing metabolic abnormalities[16]
Coagulation screen – may show evidence of disseminated intravascular coagulation such as prolonged thrombin time, elevated fibrin degradation products or D-dimer, or low fibrinogen or antithrombin levels.
Seek consent and test all patients with meningitis for HIV as a screen for predisposition to meningitis.[16]
HIV infection is associated with a higher incidence of bacterial meningitis and a corresponding higher mortality than in the general population.[16]
Up to 24% of patients with acute HIV seroconversion illness present with meningitis, but HIV antibody tests may be negative in this early phase of the illness.[16][49][50]
Measure serum procalcitonin (PCT) if available as it may help differentiate bacterial from other inflammatory causes.[16] However, it cannot help determine the site of the infection.[16][25]
PCT may be raised or normal in bacterial meningitis.
In adults, a serum PCT of ≥0.74 ng/mL has a sensitivity of 95% (95% CI 82.2% to 99.3%) and a specificity of 100% (95% CI 88.7% to 100%) for differentiating between bacterial and viral meningitis.[16][51]
If PCT is unavailable, check serum C-reactive protein (CRP) concentrations.[16] CRP is likely to be high in the presence of bacterial infection.
If the cerebrospinal fluid Gram stain is negative and the differential diagnosis is between bacterial and viral meningitis, a normal serum CRP concentration excludes bacterial meningitis with around 99% certainty.[52]
Cerebrospinal fluid
Do a lumbar puncture (LP) to obtain cerebrospinal fluid (CSF) within 1 hour of arrival at hospital unless there are indications for neuroimaging or contraindications (see below).[16] Do not delay starting antibiotics for LP.
The need for a rapid LP has to be weighed against the desire to start antimicrobial treatment urgently.[16]
Carry out LP even if the patient has started antibiotics, preferably within 4 hours of starting treatment.[16]
Some guidelines recommend giving antibiotics after LP (where LP is indicated and as long as LP is not delayed) to allow the best chance of definitive diagnosis.[16] The culture rate can drop off rapidly after 4 hours, making it difficult to identify the causative organism (but prompt molecular tests will still identify the causative organism even after antibiotics have been started).
At least 15 mL of CSF is required for investigations.[16][27] Inform the lab of an urgent CSF sample, which will need confirmation of receipt and urgent processing.
Biochemical measurements can indicate the likely cause of bacterial meningitis, but are not always definitive. Interpret results within the clinical context.
How to perform a diagnostic lumbar puncture in adults. Includes a discussion of patient positioning, choice of needle, and measurement of opening and closing pressure.
Measure opening pressure (if patient is horizontal).[16]
Request the following to be performed on the CSF sample.
CSF microscopy, Gram stain, culture, and sensitivities[16]
Gram stain rapidly and accurately identifies the causative bacteria in 60% to 90% of patients with community-acquired meningitis.[59] It has a sensitivity of 50% to 99% and a specificity of 97% to 100%.[16][17] This means that if bacteria are present in the CSF, you can be certain of the diagnosis, but a lack of bacteria on the Gram stain does not exclude the diagnosis of bacterial meningitis.
The likelihood of a positive Gram stain result depends on the specific pathogen: the Gram stain is positive in 90% in cases of pneumococcal meningitis, 70% to 90% in cases of meningococcal meningitis, 50% in cases of Haemophilus influenzae meningitis, and 25% to 35% in Listeria monocytogenes meningitis.[25][60][61]
CSF culture is diagnostic in 70% to 85% of patients.[44] However, even if culture is negative due to antibiotic administration, bacteria may be identifiable in the CSF for up to 48 hours after intravenous antibiotics.[16][Figure caption and citation for the preceding image starts]: Gram-stained Streptococcus species bacteriaCDC Public Health Image Library [Citation ends].
 [Figure caption and citation for the preceding image starts]: Staphylococcus aureusCDC/Matthew J. Arduino, DRPH [Citation ends].
[Figure caption and citation for the preceding image starts]: Staphylococcus aureusCDC/Matthew J. Arduino, DRPH [Citation ends]. [Figure caption and citation for the preceding image starts]: Escherichia coliCDC/Janice Haney Carr [Citation ends].
[Figure caption and citation for the preceding image starts]: Escherichia coliCDC/Janice Haney Carr [Citation ends].
CSF cell count
CSF biochemistry
CSF protein[16]
Bacterial meningitis tends to have a higher CSF protein than viral meningitis.[63]
CSF glucose[16]
The CSF glucose is low in bacterial meningitis, but the concentration is affected by the concomitant plasma glucose.[64] Therefore, blood glucose should be checked at the same time as the LP to allow interpretation of the CSF glucose. Normally CSF glucose is about two-thirds of the plasma glucose.[16] A CSF glucose concentration of <2.5 mmol/L (<45 mg/dL) or <40% of simultaneously measured serum glucose in bacterial meningitis is likely to indicate a bacterial meningitis.[17]
CSF lactate[16]
CSF PCR for pneumococcus (and meningococcus – see Meningococcal disease)[16]
PCR is useful in distinguishing bacterial from viral meningitis.
It is helpful in diagnosing bacterial meningitis in patients who have been pre-treated with antibiotics.[45]
CSF PCR has been reported to have a sensitivity of 79% to 100% for Streptococcus pneumoniae, and 67% to 100% for H influenzae.[25][29]
The value of L monocytogenes PCR is currently unclear.[25][29]
About 5% to 26% of cases of meningitis are caused by bacteria other than S pneumoniae, Neisseria meningitidis, or H influenzae and are not routinely detected by PCR.[25][29]
CSF PCR for tuberculosis (TB) if you have a high clinical suspicion for TB meningitis.[16]
Evidence: CSF lactate
CSF lactate differentiates bacterial from viral meningitis more accurately than CSF glucose, CSF/plasma glucose ratio, CSF protein, or CSF total number of leukocytes. If measured prior to starting antibiotics, CSF lactate has a high negative predictive value to rule out bacterial meningitis and provides reassurance to stop or withhold antibiotics.
One meta-analysis of 25 studies performed in 16 countries and including 783 patients with bacterial meningitis and 909 patients with viral meningitis found that CSF lactate had excellent accuracy in predicting bacterial meningitis. In a head-to-head meta-analysis of these 25 studies, the diagnostic accuracy of the CSF lactate concentration cut-off of >35 mg/dL was higher than that of CSF glucose, CSF/plasma glucose ratio, CSF protein, or CSF total number of leukocytes.[65]
A second meta-analysis included 33 studies. The pooled test characteristics of CSF lactate were sensitivity 0.93 (95% CI 0.89 to 0.96), specificity 0.96 (95% CI 0.93 to 0.98), likelihood ratio positive 22.9 (95% CI 12.6 to 41.9), likelihood ratio negative 0.07 (95% CI 0.05 to 0.12), and diagnostic odds ratio 313 (95% CI 141 to 698), and suggested a CSF lactate of 35 mg/dL could be the optimal cut-off value for distinguishing bacterial meningitis from aseptic meningitis. The sensitivity of CSF lactate concentration was reduced by about 50% in patients who received antibiotic treatment before lumbar puncture, compared with those not receiving antibiotic pre-treatment.[66]
Classic cerebrospinal fluid features of the different causes of meningitis[16] (reproduced with permission) | |||||
Normal | Bacterial | Viral | Tuberculosis | Fungal | |
Opening pressure (cm CSF) | 12 to 20 | Raised | Normal/mildly raised | Raised | Raised |
Appearance | Clear | Turbid, cloudy, purulent | Clear | Clear or cloudy | Clear or cloudy |
CSF WBC count (cells/uL) | <5 | Raised (typically >100)a | Raised (typically 5 to 1000)a | Raised (typically 5 to 500)a | Raised (typically 5 to 500)a |
Predominant cell type | n/a | Neutrophilsb | Lymphocytesc | Lymphocytesd | Lymphocytes |
CSF protein (g/L) | <0.4 | Raised | Mildly raised | Markedly raised | Raised |
CSF glucose (mmol) | 2.6 to 4.5 | Very low | Normal/slightly low | Very low | Low |
CSF/plasma glucose ratio | >0.66 | Very low | Normal/slightly low | Very low | Low |
Local laboratory ranges for biochemical tests should be consulted and may vary from those quoted here. A traumatic lumbar puncture will affect the results by falsely elevating the white cells due to excessive red cells. A common correction factor used is 1:1000. aOccasionally the CSF WBC count is normal (especially in immunodeficiency or tuberculous meningitis). bMay be lymphocytic if antibiotics given before lumbar puncture (partially treated bacterial meningitis), or with certain bacteria (e.g., Listeria monocytogenes). cMay be neutrophilic in enteroviral meningitis (especially early in disease). dMay be neutrophils early in the course of disease. | |||||
Do NOT perform lumbar puncture if there is infection at the lumbar puncture site.[16] This is an absolute contraindication.
Delay lumbar puncture but DO give antibiotics if you suspect bacterial meningitis and the patient has any of the following relative contraindications:[16]
Shock[68]
Suspected sepsis or rapidly progressing rash
Severe respiratory or cardiac compromise
Confirmed/known bleeding or high risk of bleeding
Signs of raised intracranial pressure, such as:
Focal neurological signs
Papilloedema
Continuous or uncontrolled seizures
Glasgow Coma Scale (GCS) score ≤12. [ Glasgow Coma Scale Opens in new window ]
Specific GCS levels indicating a need to delay lumbar puncture or to obtain cranial imaging are debated. Seek senior advice if you are uncertain about either of these situations.
Review the decision to delay lumbar puncture at 12 hours and regularly thereafter.[16]
Debate: Glasgow coma scale (GCS) thresholds for neuroimaging prior to lumbar puncture
Guidelines acknowledge the uncertainty remaining about the ideal GCS score to indicate a requirement for neuroimaging prior to lumbar puncture.
The exact GCS score recommended by guidelines to indicate the requirement for a computed tomographic scan prior to lumbar puncture ranges from <8 (the European Federation of Neurological Societies) to <13 (the Association of British Neurologists and British Infection Association).[69][70]
Some guidelines are non-specific, stating ‘abnormal level of consciousness’.[71] This means obtunded/not alert or unresponsive.[28]
The UK joint specialist societies guideline recommends that a lumbar puncture can be performed without prior neuroimaging if the GCS score is >12, and may be safe at lower levels.[69][70] The European Society of Clinical Microbiology and Infectious Diseases guideline recommends neuroimaging if the GCS score is <10.[25]
A decision about whether to obtain neuroimaging prior to lumbar puncture will depend on your local protocols and resources, as well as the clinical picture in individual patients.
Wait 4 hours after the lumbar puncture before starting prophylactic subcutaneous low molecular weight heparin should an individual patient require anticoagulation.
Be aware that specific recommendations exist for lumbar puncture in patients on anticoagulants.[16] UK joint specialist societies guideline: when should a lumbar puncture be performed in patients who are on anticoagulants? Opens in new window
Cranial computed tomography
Perform cranial imaging before lumbar puncture if there is a risk of cerebral herniation due to conditions such as brain abscess, subdural empyema, or large cerebral infarction.[25][28][29]
This has been a controversial area.[16][30][31] Delaying LP for a CT scan can cause delays in antibiotic administration, which may lead to an increase in mortality.[32][33]
In practice, most patients will have LP without the need for prior neuroimaging.[16]
The following signs suggest risk of cerebral herniation secondary to raised intracranial pressure:
Papilloedema[16]
Focal neurological deficits (excluding nerve palsies)[16][25]
Altered mental status[16][25] [ Glasgow Coma Scale Opens in new window ]
Severe immunocompromise.[25]
Regardless of decisions about pre-LP neuroimaging, delay or do NOT perform LP in the following situations:[16][25]
Respiratory or cardiac compromise
Signs of severe sepsis or a rapidly evolving rash
Infection at the site of the LP
A coagulopathy.
Specific GCS levels indicating a need to delay lumbar puncture or to obtain cranial imaging are debated. Seek senior advice if you are uncertain about either of these situations.
Computed tomography (CT) scan may identify a tumour, a brain abscess, or meningitis-associated complications such as brain infarction, generalised cerebral oedema, or hydrocephalus.[25][72]
CT scan will not pick up raised intracranial pressure per se.
Neuroimaging is not indicated unless you suspect alternative pathology (i.e., because there are signs indicating risk of cerebral herniation).[16]
In practice, magnetic resonance imaging should be done only if pathology is suspected that is not evident on CT.
Evidence: Whether to scan
Neuroimaging (CT of the head) prior to lumbar puncture may delay this procedure and the administration of antibiotics, increasing the risk of mortality from meningitis. However, it can expose or rule out contraindications to lumbar puncture, potentially reducing the risk of brain herniation.
Because prompt diagnosis and intravenous antibiotic treatment are key to survival, the 2016 UK joint specialist societies guideline recommends that patients with suspected meningitis (with no signs of shock or sepsis) should have a lumbar puncture, where it is safe to do so, before starting antibiotics to allow the best chance of a definitive diagnosis.[16]
The UK joint specialist societies guideline makes a strong recommendation that, where it is safe to do so, a lumbar puncture should be performed within 1 hour of arrival at hospital, based on very low-quality evidence (assessed using GRADE).
However, the guideline states that it is not safe to perform a lumbar puncture without first doing neuroimaging if there are signs of significant brain swelling and a shift of compartments (due to the risk of brain herniation post lumbar puncture), including:
Focal neurological signs
Papilloedema
Continuous or uncontrolled seizures
Glasgow Coma Scale (GCS) score ≤12 (although the guideline authors state there is some uncertainty over the exact GCS level).
The UK joint specialist societies guideline recommends (based on guideline working group consensus) that regardless of consideration about neuroimaging, lumbar puncture is delayed/avoided with:[16]
Respiratory or cardiac compromise
Signs of sepsis or a rapidly evolving rash
Infection at the site of the lumbar puncture
A coagulopathy
Focal neurological deficits (excluding cranial nerve palsies)
New-onset seizures
Severely altered mental status (GCS score <10)
Severely immunocompromised state.
If neuroimaging shows no signs of risk of cerebral herniation, perform a lumbar puncture as soon as possible unless:[16]
An alternative diagnosis is established
The patient has:
Repeated seizures
Deteriorating GCS [ Glasgow Coma Scale Opens in new window ]
Severe cardiac/respiratory compromise.
Other microbiological tests
Do not obtain a nasal swab for pneumococcal disease.[16]
It is not clear whether nasal strains are definitely related to that which caused the meningitis.
Additional tests for viral meningitis
In the UK, the commonest viral causes of meningitis are enteroviruses and herpes viruses.[16] If tests are negative for bacterial aetiology but you still suspect meningitis, confirm the diagnosis with:[16]
CSF, stool, and throat swab PCR for enterovirus
CSF PCR for herpes simplex virus (HSV) 1 and 2 and varicella zoster virus.
How to perform a diagnostic lumbar puncture in adults. Includes a discussion of patient positioning, choice of needle, and measurement of opening and closing pressure.
Use of this content is subject to our disclaimer
