Summary
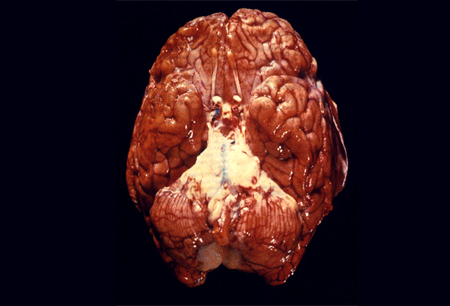
Definition
History and exam
Key diagnostic factors
- headache
- neck stiffness
- fever
- altered mental status
- vomiting
- confusion
- photophobia
- seizures
- presence of risk factors
Other diagnostic factors
- focal neurological signs
- abnormal eye movement
- facial palsy
- balance problems/hearing impairment
- rash
- papilloedema
- Kernig's sign
- Brudzinski's sign
Risk factors
- advanced age
- crowding
- exposure to pathogens
- immunocompromising conditions
- cranial anatomical defects/ventriculoperitoneal shunt
- cochlear implants
- sickle cell disease
- contiguous infection
- genetic predisposition
Diagnostic investigations
1st investigations to order
- blood culture
- serum pneumococcal and meningococcal PCR
- blood glucose
- FBC and differential
- serum urea, creatinine, and electrolytes
- venous blood gas
- LFTs
- coagulation screen (prothrombin time, INR, activated PTT, fibrinogen, fibrin degradation products)
- serum HIV
- serum procalcitonin (PCT)
- serum CRP if PCT not available
- cerebrospinal fluid (CSF) protein
- CSF lactate
- CSF glucose
- CSF microscopy, Gram stain, culture, and sensitivities
- CSF cell count
- CSF polymerase chain reaction (PCR) for pneumococcus
Investigations to consider
- neuroimaging
- CSF PCR for tuberculosis
- CSF PCR for herpes simplex virus (HSV) 1 and 2 and varicella zoster virus
- CSF, stool, and throat swab PCR for enterovirus
Treatment algorithm
Contributors
Expert advisers
Alexander Alexiou, MBBS, BSc, DCH, FRCEM, Dip IMC RCSEd
Emergency Medicine Consultant
Barts Health NHS Trust
Physician Response Unit Consultant
London’s Air Ambulance
Royal London Hospital
London
UK
Disclosures
AA declares that he has no competing interests.
Annie Chapman, MBChB, BSc
ST4 Emergency Medicine Doctor
Royal London Hospital
Physician Response Unit Clinical Fellow
London
UK
Disclosures
AC declares that she has no competing interests.
Acknowledgements
BMJ Best Practice would like to gratefully acknowledge the previous team of expert contributors, whose work is retained in parts of the content:
A. Marceline Tutu van Furth, MD, PhD, MBA
Professor in Pediatric Infectious Diseases
Vrije Universiteit Medical Center
Amsterdam
The Netherlands
Disclosures: AMTvF declares that she has no competing interests.
Omaima El Tahir, MD
PhD Candidate
Pediatric Infectious Diseases and Immunogenetics
Vrije Universiteit Medical Center
Amsterdam
The Netherlands
Disclosures: OET declares that she has no competing interests.
Peer reviewers
Robert Taylor, MBChB, MRCP(UK), MRCP(London), DipMedTox, DipTher PGDME, FHEA FRCEM
Acute Hospital Sub Dean (Cornwall)
Honorary Clinical Senior Lecturer
Consultant Emergency Physician
The Knowledge Spa
Royal Cornwall Hospital
Truro
UK
Disclosures
RT declares that he has no competing interests.
Use of this content is subject to our disclaimer