Investigations
1st investigations to order
ECG
Test
Perform an immediate ECG in any patient with an irregular pulse, whether symptomatic or not, who you suspect has acute AF.[1][3][32] Take an entire 12-lead ECG recording.[1][3] A single-lead ECG tracing of ≥30 seconds is also diagnostic.[1]
ECG is the gold-standard for diagnosis of AF.[1] An irregular pulse on palpation alone is characteristic, but not diagnostic, of AF.
[Figure caption and citation for the preceding image starts]: Atrial fibrillationFrom the collections of Arti N. Shah and Bharat K. Kantharia [Citation ends].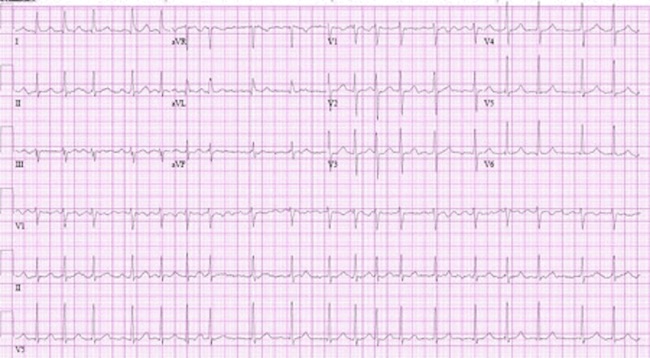
Practical tip
Don’t trust the computer. Computerised ECG interpretation is prone to error, particularly in patients who are continuously or intermittently paced.[54][55] Ensure any automated interpretation is verified in person by a skilled reader of ECGs. Ventricular/atrial ectopics are key differentials for an irregularly irregular pulse.
As well as informing diagnosis, use ECG to screen for:
Conduction defects
If there is AF and atrioventricular conduction block, a slow regular ventricular escape rhythm is usually present with no distinct P waves
Ischaemia or structural heart disease
ST–T-wave changes may be present; caused by rate-related ischaemia, digoxin therapy, or structural heart disease such as hypertrophic obstructive cardiomyopathy
Underlying structural heart disease
Primary electrical disorders such as Brugada pattern or a pre-excitation syndrome such as Wolff-Parkinson-White syndrome. See Wolff-Parkinson-White syndrome.
Practical tip
It’s easy to miss patients with AF and complete heart block. Look out for the key ECG features:[56]
No distinct P-waves; just fibrillary waves of AF
Regular ventricular rhythm
The wider the QRS of the ventricular escape rhythm the less reliable the escape mechanism.
These patients will often need a pacemaker (if they are not taking rate-limiting drugs).
How to record an ECG. Demonstrates placement of chest and limb electrodes.
Result
No discernible or distinct P wave activity (chaotic baseline) AND irregularly irregular ventricular rate (R-R intervals; where atrioventricular conduction is not impaired)
Conduction defects: if there is AF and atrioventricular conduction block, a slow regular ventricular escape rhythm is usually present with no distinct P waves
Ischaemia or structural heart disease: ST–T-wave changes may be present; caused by rate-related ischaemia, digoxin therapy, or structural heart disease such as hypertrophic obstructive cardiomyopathy
Brugada pattern: (right bundle-branch block with ST-segment elevation in the V1-3 leads)
FBC
Test
Request FBC in all patients.[1][32]
Use to detect non-cardiac factors precipitating AF (e.g., anaemia and infection).
Send blood samples as soon as possible. Do not delay management by waiting for these test results; start treatment straight away (urgent cardioversion may be required).
Result
normal range but can be elevated or reduced
clotting profile
Test
Always request a clotting profile.[32]
Take as a baseline to identify any patient with an underlying coagulation defect and inform management with anticoagulants.
Send blood samples as soon as possible. Do not delay management by waiting for these test results; start treatment straight away (urgent cardioversion may be required).
Result
baseline values
electrolytes, urea, and creatinine
Test
Request in all patients to exclude renal impairment, hypokalaemia, hyperkalaemia, and hypomagnesaemia.[1][32]
Chronic kidney disease is a general cardiac risk factor and a specific risk factor for AF.[57]
Estimate creatinine clearance using the Cockroft-Gault equation; this will help inform anticoagulant dosing. [ Creatinine Clearance Estimate by Cockcroft-Gault Equation Opens in new window ]
Send blood samples as soon as possible. Do not delay management by waiting for these test results; start treatment straight away (urgent cardioversion may be required).
Result
may show electrolyte abnormalities; high or low potassium, or low magnesium; baseline values
thyroid function
Test
Request thyroid function testing for all patients.[1][32]
Use to exclude thyrotoxicosis.
Send blood samples as soon as possible. Do not delay management by waiting for these test results; start treatment straight away (urgent cardioversion may be required).
Result
suppressed thyroid-stimulating hormone (with elevated free T4 and/or T3) in thyrotoxicosis
CXR
Test
Request a CXR as routine for all cardiac presentations, particularly if you suspect lung pathology.
Result
may show cardiomegaly (in particular, left atrial enlargement); signs of heart failure; other precipitating pathology, such as pneumonia
transthoracic echocardiography (TTE)
Test
In line with guidelines from the European Society of Cardiology, request TTE in all patients to check for:[1]
Left ventricular size and function
Left atrium size
Valvular disease
Right ventricular size and function.
Bear in mind that guidelines from the National Institute for Health and Care Excellence in the UK recommend only requesting a TTE in specific circumstances, particularly for people with AF:
For whom a baseline echocardiogram is important for long-term management[3]
In practice, this will be where there is no obvious reversible non-cardiac cause that is unlikely to have other cardiac consequences (e.g., infection or thyrotoxicosis)
For whom you are considering a rhythm-control strategy that includes cardioversion (electrical or pharmacological)[3]
In whom there is a high risk of, or you suspect, underlying structural/functional heart disease (such as heart failure or heart murmur) that influences their subsequent management (e.g., choice of anti-arrhythmic drug)[3]
In whom refinement of clinical risk stratification for antithrombotic therapy is needed.[3]
Practical tip
Perform a transthoracic echocardiogram within 48 hours of admission in people presenting with new suspected heart failure in the absence of a recent echocardiogram.[40] In practice, refer confirmed heart failure to a specialist.
Result
may show dilated left atrium; valvular disease; low left ventricular ejection fraction; diastolic dysfunction
Investigations to consider
cardiac troponin
Test
Request cardiac troponin in selected patients.[1] High-sensitivity cardiac troponin T may be elevated due to prolonged tachycardia or post DC cardioversion but not at the levels usually seen with myocardial infarction and acute coronary syndromes.
Result
may be elevated
ABG
Test
Use to exclude hypoxia.
Result
may show hypoxia
CRP
Test
Request for selected patients.[1]
Result
may be elevated
B-natriuretic peptide (BNP)/N-terminal prohormone B-natriuretic peptide (NT-pro-BNP)
Test
Request for selected patients.[1]
Result
may be elevated in heart failure
LFTs
Test
Use to exclude the presence of a multisystem disorder affecting the liver.[32]
Also use to guide choice of appropriate anti-arrhythmic drugs and to monitor anti-arrhythmic therapy. For example, amiodarone is contraindicated in the presence of liver dysfunction; amiodarone treatment should be discontinued when LFTs show abnormalities.
Result
baseline values
erythrocyte sedimentation rate
Test
Request for selected patients.[1]
Result
may be elevated
transoesophageal echocardiogram (TOE)
Test
Discuss arranging a TOE, if available, with a cardiologist in people with atrial fibrillation when:[1][3]
TTE demonstrates an abnormality (such as valvular heart disease) that warrants further specific assessment
TTE is technically difficult and/or of questionable quality and there is a need to exclude cardiac abnormalities
You are considering TOE-guided cardioversion.
Practical tip
TOE may not be readily available in the usual settings of care (e.g., accident and emergency department or general practice office). Therefore, in practice, base management decisions on the likely duration of arrhythmia rather than the presence or absence of intracardiac clot on echocardiographic imaging.
[Figure caption and citation for the preceding image starts]: Transoesophageal echocardiogram showing left atrial appendage clot. LA, left atrium; LAA, left atrial appendage; LV, left ventricleFrom the collection of Dr Bharat Kantharia [Citation ends].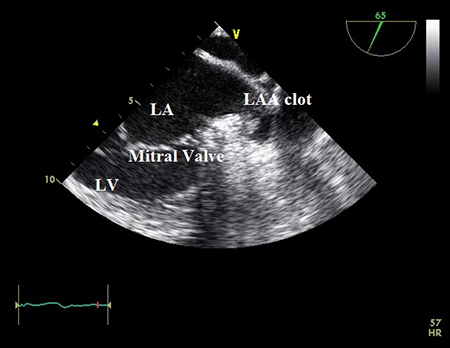
Result
may show presence of atrial thrombus; may detect valvular heart disease
inpatient telemetry or 24-hour holter monitor
coronary angiography (CT or conventional) or stress testing
Test
Request if you suspect significant coronary artery disease from the patient’s history and risk factor profile.[1]
Result
detection of structural abnormalities or coronary artery disease; detection of left atrial appendage clot
late gadolinium contrast-enhanced cardiac MR (CMR)
Test
Consider, based on individual patient presentations.[1] For example, if you suspect structural heart disease or cardiomyopathic process after TOE/TTE, late gadolinium contrast-enhanced CMR can help guide management decisions.
Result
detection of structural heart disease or cardiomyopathic process; detection of left atrial appendage clot (must be specifically pre-specified)
brain CT
Test
Consider brain imaging for some patients.[1] In patients with AF and signs of cerebral ischaemia or stroke, imaging the brain can help detect stroke and guide management decisions regarding acute management and long-term anticoagulation.
Result
detection of stroke; baseline values
brain MRI
Test
Consider brain imaging for some patients.[1] In patients with AF and signs of cerebral ischaemia or stroke, imaging the brain can help detect stroke and guide management decisions regarding acute management and long-term anticoagulation.
Result
detection of stroke; baseline values
computed tomographic pulmonary angiography (CTPA)
Test
Request if AF is secondary to pulmonary embolism (PE). CTPA is the preferred investigation for definitive confirmation of PE in most patients.[60][61] See Pulmonary embolism.
Result
PE is confirmed by direct visualisation of thrombus in a pulmonary artery; appears as a partial or complete intraluminal filling defect
Use of this content is subject to our disclaimer
