Differentials
Common
Cystitis
History
rapid onset, history of previous urinary tract infection (UTI), sexual activity/spermicide/diaphragm use (higher risk in women), post-menopausal status (women), history of benign prostatic hypertrophy (men), instrumentation, urinary frequency/urgency, cloudy or malodorous urine, haematuria
Exam
suprapubic discomfort, absence of costovertebral tenderness
1st investigation
Other investigations
- pregnancy test:
positive or negative
More - renal ultrasound:
in uncomplicated cases, should be normal; in complicated or recurrent cases may show abnormalities such as dilation of the renal pelvis or ureters, or distension of thick-walled bladder; renal abscess: area of radiolucency to the renal parenchyma with local hypoperfusion on colour Doppler; perinephric abscess: hypoechoic fluid
More
Urethritis
History
gradual onset (over days), most common in young patients, sexual activity, urinary frequency/urgency, urethral discharge (common in men, rare in women), post-coital or intermenstrual bleeding
Exam
variable (watery or thick) discharge, suprapubic discomfort (may be present if associated with pelvic inflammatory disease in women)
1st investigation
- urine dipstick:
leukocyte esterase-positive; positive for red blood cells
More - nucleic acid amplification test:
positive for Chlamydia trachomatis, Neisseria gonorrhoeae, or mycoplasma genitalium
More - Gram stain of urethral discharge:
gram-negative diplococci within polymorphonuclear leukocytes confirm N gonorrhoeae infection
More
Other investigations
- urethral or vaginal culture:
positive for C trachomatis or N gonorrhoeae
More - serum rapid plasma reagent or VDRL:
excludes syphilis
- HIV serology:
excludes HIV in high-risk groups
Pyelonephritis
History
fever, rigors, myalgia, headache, nausea, vomiting, flank pain, urinary frequency/urgency, diabetes, immunosuppression, history of anatomical abnormality
Exam
fever, costovertebral angle tenderness, deep right or left upper quadrant tenderness
1st investigation
- urine dipstick:
nitrite- and/or leukocyte esterase-positive; positive for red blood cells
More - urine microscopy:
leukocytes and/or bacteria
- urine culture:
>10⁵ colony-forming units/mL
Other investigations
- renal ultrasound:
abnormalities such as dilation of the renal pelvis or ureters, or distension of thick-walled bladder; renal abscess: area of radiolucency to the renal parenchyma with local hypoperfusion on colour Doppler; perinephric abscess: hypoechoic fluid
More - CT renal tract:
excludes hydronephrosis, abscess, and renal calculi
More
Vulvovaginitis (including bacterial vaginosis)
History
external irritation, premenstrual exacerbation (cyclical), recent sexual history, insidious onset (weeks to months), vaginal discharge or pruritus, dyspareunia
Exam
inflamed vaginal mucosa or cervix, cervical motion tenderness; inflamed, red vagina with satellite vaginal pustules (candidal)
1st investigation
Other investigations
Balanitis/balanoposthitis
History
may have history of sexually transmitted infection (STI), diabetes, or dermatological conditions such as eczema, psoriasis, or lichen sclerosus
Exam
inflammation and erythema of glans penis (balanitis) or glans penis and prepuce (balanoposthitis); may be associated with itching, soreness, discharge
1st investigation
- clinical diagnosis:
diagnosis is usually made based on history and examination
Other investigations
- swab for microscopy and culture:
may be positive for Candida albicans, streptococci, or anaerobes
- nucleic acid amplification test:
may be positive for Chlamydia trachomatis or Neisseria gonorrhoeae
Acute prostatitis
History
perineal or rectal pain, urinary frequency/urgency, diminished urinary stream
Exam
tender or boggy prostate, may have fever
1st investigation
Other investigations
Benign prostatic hyperplasia
History
poor urinary flow, nocturia; urinary hesitancy, intermittency, dribbling, frequency/urgency; haematuria
Exam
enlarged smooth prostate
1st investigation
Other investigations
- urodynamic study:
abnormal bladder pressure, abnormal bladder voiding
Urolithiasis
History
sudden onset of colicky flank/groin pain, nausea, vomiting, pain radiates to testicle and tip of penis (men) or vagina/vulva (women), urinary frequency/urgency, stone in the bladder or urethra can cause a ball-valve effect, inability to get comfortable (ureteric calculi), haematuria
Exam
costovertebral angle tenderness
1st investigation
- urine dipstick:
may be leukocyte esterase-positive; positive for red blood cells
- low-dose non-contrast CT:
renal or ureteric calculi
More
Other investigations
- renal ultrasound:
acoustic shadowing
More
Local irritants
History
history of use of scented soaps, vaginal sprays, vaginal douches, bubble baths, sanitary products
Exam
usually normal
1st investigation
- clinical diagnosis:
diagnosis is made based on history and examination
Other investigations
Uncommon
Genital herpes simplex virus (HSV)
History
gradual onset, sexual activity, fever, headache, myalgia, vulvar pain, vaginal discharge (possible)
Exam
grouped painful vesicles (usually on cervix or pubic area, but may be vaginal), tender inguinal adenopathy
1st investigation
Other investigations
Epididymo-orchitis
History
painful and/or swollen testicle, developing over the course of a few days, may have risk factors for STI; bladder outlet obstruction, urinary tract infection, recent instrumentation of the urinary tract, and immunosuppression are associated with infection with enteric organism
Exam
erythema, generalised swelling or tenderness of epididymis or testicle
1st investigation
- urine dipstick:
nitrite- and/or leukocyte esterase-positive
More - urine microscopy:
may be positive for leukocytes and/or bacteria
- urine culture:
may be positive (>10⁵ colony-forming units/mL)
- nucleic acid amplification test:
may be positive for Chlamydia trachomatis, Neisseria gonorrhoeae, or mycoplasma genitalium
Other investigations
- scrotal ultrasound:
evidence of abscess, hyperaemia, or malignancy
More
Cervicitis
History
dyspareunia, intermenstrual or post-coital bleeding, urinary frequency
Exam
cervical motion tenderness; possible vaginal discharge
1st investigation
- nucleic acid amplification test:
positive for Chlamydia trachomatis, Neisseria gonorrhoeae, or mycoplasma genitalium
More - Thayer-Martin agar cervical culture:
growth of pathogen
Other investigations
Schistosomiasis
History
travel history to endemic area and exposure to fresh water, urinary frequency/urgency, terminal haematuria
Exam
rash, fever, lymphadenopathy, genital ulcer
1st investigation
Other investigations
Tuberculosis
History
chronic, intermittent, and non-specific symptoms; urinary hesitancy/frequency/urgency
Exam
tender testicle or epididymis
1st investigation
- urine dipstick:
leukocyte esterase-positive; positive for red blood cells
- chest x-ray:
consolidation, pulmonary infiltrates, mediastinal or hilar lymphadenopathy, upper zone fibrosis
More - sputum acid-fast bacilli smear and culture:
presence of acid-fast bacilli (Ziehl-Neelsen stain) in specimen
More - nucleic acid amplification tests (NAAT):
positive for M tuberculosis
More
Other investigations
- CT urography (intravenous contrast):
calcifications, cavitations, or signs of obstruction suggest tuberculosis
- lateral flow urine lipoarabinomannan (LF-LAM) assay:
positive
More
Urethral stricture/stenosis
History
history of previous instrumentation or trauma, nocturia; urinary hesitancy, intermittency, dribbling, frequency/urgency, poor flow
Exam
usually normal
1st investigation
- uroflowmetry:
typical plateau pattern noted
More
Instrumentation or catheterisation
History
urethral instrumentation, catheterisation, or surgery; haematuria
Exam
usually normal
1st investigation
- urine dipstick:
positive for red blood cells and sometimes leukocytes; diagnosis is often clinical and symptoms resolve rapidly
Other investigations
Sexual abuse
History
disclosure of previous or current sexual abuse, enhanced awareness of dysuria
Exam
may be normal, signs of genital trauma
1st investigation
- nucleic acid amplification test:
may be positive for Chlamydia trachomatis, Neisseria gonorrhoeae, or mycoplasma genitalium
More - HIV serology:
may be positive
More - serum rapid plasma reagin test:
may be positive for syphilis
More - serum VDRL test:
may be positive for syphilis
More - viral culture of lesion:
may be positive for herpes simplex
More - herpes simplex virus polymerase chain reaction (HSV PCR):
may be positive for herpes simplex
More
Other investigations
Athletics
History
horse riding or bicycling, haematuria
Exam
usually normal
1st investigation
- urine dipstick:
positive for red blood cells and sometimes leukocytes; diagnosis is often clinical and symptoms resolve rapidly
Other investigations
Interstitial cystitis
History
most common in middle-aged women, often long-standing symptoms, suprapubic and pelvic pain/pressure/discomfort, daytime and night-time urinary frequency/urgency, haematuria
Exam
suprapubic discomfort
1st investigation
- urine dipstick:
normal; may be positive for red blood cells
More - urine microscopy:
normal
- urine culture:
normal
Other investigations
- cystoscopy:
glomerulations, submucosal petechiae, mucosal tears, presence of Hunner's ulcers, contracted bladder wall with low anaesthetic bladder capacity; petechial haemorrhage in 4 quadrants on second fill; elevated mast cell count in the lamina propria on biopsy
Atrophic vaginitis
History
post-menopausal women, external irritation/pruritus, dyspareunia, itch, vaginal discharge, vaginal bleeding, lack of oestrogen replacement
Exam
inflammation and patchy erythema; pale, smooth, and shiny atrophic epithelium, petechiae, increased friability
1st investigation
- clinical diagnosis:
diagnosis is made based on history and examination
Other investigations
Spondyloarthropathies
History
urinary frequency/urgency, arthralgia, back pain, eye irritation, diarrhoea
Exam
joint tenderness, conjunctivitis, oral mucosal ulcerations, penile lesion (circinate balanitis), psoriatic lesions
1st investigation
- pathergy testing:
formation of pustule within 48 hours
- HLA-B51:
may be present
Other investigations
Non-infectious prostatitis
History
history of previous acute prostatitis, perineal pain, testicular or penile tip pain, back pain, lower urinary tract symptoms
Exam
may have normal examination or tender prostate
1st investigation
- urine dipstick:
nitrite- and/or leukocyte esterase-negative
More
Other investigations
- Stamey test:
absence of bacteria
More
Primary prostate pain syndrome
History
persistent pelvic pain of at least 3 months’ duration centred around the prostate, pain may also occur in other pelvic areas outside the prostate including in the rectum and/or the perineum, penis, testicles, abdomen, lower back and inguinal region, associated lower urinary tract signs and symptoms, and/or signs and symptoms of sexual dysfunction, such as dysuria urinary frequency, urinary urgency +/-urge incontinence, poor stream, nocturia or pain on or after ejaculation in the absence of proven infection, or other obvious local pathology
Exam
digital rectal examination: to assess for pain on palpation and to exclude prostate abnormalities, to examine the rectum for abnormalities as well as pelvic floor muscle for tenderness and ability to contract or relax
1st investigation
- clinical diagnosis:
diagnosis is made based on history and examination
More
Other investigations
Ketamine bladder
History
ketamine use, urinary frequency/urgency, haematuria
Exam
suprapubic pain may be present
1st investigation
- urine microscopy:
normal; may be evidence of pyuria and red blood cells
- urine culture:
normal
- cystoscopy:
inflammation and ulceration of bladder; bladder may have thick wall with a small capacity
Other investigations
Urinary fistula
History
inflammatory bowel disease (e.g., Crohn's disease), diverticulitis, malignancy, recurrent urinary tract infection, or pelvic radiotherapy; passing debris in urine, incontinence, pneumaturia
Exam
suprapubic discomfort
1st investigation
- urine dipstick:
nitrite- and/or leukocyte esterase-positive; positive for red blood cells
- urine microscopy:
leukocytes and/or bacteria
- urine culture:
>10⁵ colony-forming units/mL
- cystoscopy:
allows direct visualisation of fistula
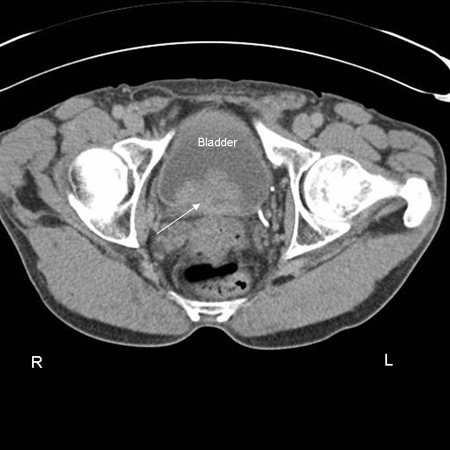
- CT abdomen/pelvis with and without contrast:
presence of fistula
- MRI abdomen/pelvis:
helps establish extent of fistula and underlying pathology
Other investigations
- colonoscopy:
identifies abnormal gastrointestinal pathology
More
Prostate cancer
History
haematuria, urinary frequency/urgency, lower urinary tract symptoms, back pain
Exam
prostate examination may be normal; firm, nodular, or irregular prostate
1st investigation
- prostate-specific antigen (PSA):
elevated
More
Bladder cancer
History
haematuria, urinary frequency/urgency, smoking or exposure to chemicals (e.g., aromatic amines), family history
Exam
usually normal
1st investigation
Other investigations
Renal cancer
Cervical cancer
History
haematuria; intermenstrual, post-coital, or post-menopausal bleeding; menorrhagia; urinary frequency/urgency; pelvic pain, dyspareunia; vaginal discharge; more common in patients who have HIV
Exam
vaginal or pelvic mass; mass might be directly visualised with speculum, or cervical bleeding may occur
1st investigation
- colposcopy:
abnormal
More
Other investigations
- CT whole body:
detection of nodal involvement and metastases
Urethral cancer
History
may be asymptomatic and insidious, lower urinary tract symptoms, haematuria, urethral discharge, urethral pain
Exam
may be normal, penile/vaginal lesions, fistulae, lymphadenopathy, bloody discharge at meatus
1st investigation
- cystoscopy:
lesion(s) in urethra visualised
Other investigations
Penile cancer
History
haematuria, urinary frequency/urgency
Exam
penile lesion
1st investigation
- biopsy:
evidence of squamous cell carcinoma
Other investigations
- MRI whole body:
staging investigation; may show nodal involvement
Drugs or herbs
History
history of use of dopamine, cantharidin, ticarcillin, penicillin-G, cyclophosphamide
Exam
usually normal
1st investigation
- clinical diagnosis:
diagnosis is made based on history and examination
Other investigations
Use of this content is subject to our disclaimer
 ]
]