The key to diagnosis of hypertensive emergency is a rapid but thorough evaluation. The main areas of focus should be the neurological, cardiovascular, and renal systems. Emergency treatment should be initiated while conducting a full diagnostic appraisal.
History
Any prior history of hypertension and previous treatment (including treatment adherence) should be identified.[7]Bress AP, Anderson TS, Flack JM, et al. The management of elevated blood pressure in the acute care setting: a scientific statement from the American Heart Association. Hypertension. 2024 Aug;81(8):e94-106.
https://www.ahajournals.org/doi/full/10.1161/HYP.0000000000000238
http://www.ncbi.nlm.nih.gov/pubmed/38804130?tool=bestpractice.com
[18]Kulkarni S, Glover M, Kapil V, et al. Management of hypertensive crisis: British and Irish Hypertension Society Position document. J Hum Hypertens. 2023 Oct;37(10):863-79.
https://www.nature.com/articles/s41371-022-00776-9
http://www.ncbi.nlm.nih.gov/pubmed/36418425?tool=bestpractice.com
Prior or existing history of neurological, cardiac, and renal impairment should also be determined.
Clinical features that may identify specific organ compromise include:[18]Kulkarni S, Glover M, Kapil V, et al. Management of hypertensive crisis: British and Irish Hypertension Society Position document. J Hum Hypertens. 2023 Oct;37(10):863-79.
https://www.nature.com/articles/s41371-022-00776-9
http://www.ncbi.nlm.nih.gov/pubmed/36418425?tool=bestpractice.com
[24]Lip GY, Beevers M, Beevers G. The failure of malignant hypertension to decline: a survey of 24 years' experience in a multiracial population in England. J Hypertens. 1994 Nov;12(11):1297-305.
http://www.ncbi.nlm.nih.gov/pubmed/7868878?tool=bestpractice.com
[40]Zampaglione B, Pascale C, Marchisio M, et al. Hypertensive urgencies and emergencies: prevalence and clinical presentation. Hypertension. 1996 Jan;27(1):144-7.
http://hyper.ahajournals.org/cgi/content/full/27/1/144
http://www.ncbi.nlm.nih.gov/pubmed/8591878?tool=bestpractice.com
[54]Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension Global Hypertension practice guidelines. Hypertension. 2020 Jun;75(6):1334-57.
https://www.ahajournals.org/doi/full/10.1161/HYPERTENSIONAHA.120.15026
http://www.ncbi.nlm.nih.gov/pubmed/32370572?tool=bestpractice.com
Neurological compromise: for example, blurry vision, dizziness, headache, seizures, change in mental status from baseline, dysphagia, loss of sensation, paraesthesia, or loss of movement
Cardiac compromise: for example, chest pain, shortness of breath, diaphoresis, orthopnoea, paroxysmal nocturnal dyspnoea, palpitations, or oedema
Renal compromise: for example, decrease in urine output.
When appropriate, use of street drugs, particularly sympathomimetics (cocaine, amphetamines, phenylpropanolamine, phencyclidine, ecstasy, LSD) should be investigated.[7]Bress AP, Anderson TS, Flack JM, et al. The management of elevated blood pressure in the acute care setting: a scientific statement from the American Heart Association. Hypertension. 2024 Aug;81(8):e94-106.
https://www.ahajournals.org/doi/full/10.1161/HYP.0000000000000238
http://www.ncbi.nlm.nih.gov/pubmed/38804130?tool=bestpractice.com
[18]Kulkarni S, Glover M, Kapil V, et al. Management of hypertensive crisis: British and Irish Hypertension Society Position document. J Hum Hypertens. 2023 Oct;37(10):863-79.
https://www.nature.com/articles/s41371-022-00776-9
http://www.ncbi.nlm.nih.gov/pubmed/36418425?tool=bestpractice.com
A diagnosis of pre-eclampsia or eclampsia should be considered in pregnant patients.[48]American College of Obstetricians and Gynecologists. Practice bulletin no. 222: gestational hypertension and preeclampsia. Jun 2020 [internet publication].
https://journals.lww.com/greenjournal/abstract/2020/06000/gestational_hypertension_and_preeclampsia__acog.44.aspx
http://www.ncbi.nlm.nih.gov/pubmed/32443077?tool=bestpractice.com
[55]American College of Obstetricians and Gynecologists. Clinical practice guideline no. 3: headaches in pregnancy and postpartum. May 2022 [internet publication].
https://journals.lww.com/greenjournal/abstract/2022/05000/headaches_in_pregnancy_and_postpartum__acog.37.aspx
http://www.ncbi.nlm.nih.gov/pubmed/35576364?tool=bestpractice.com
Commonly described features of pre-eclampsia headache include severe bilateral frontal headache and blurry vision, which may progress to bilateral cortical blindness.[55]American College of Obstetricians and Gynecologists. Clinical practice guideline no. 3: headaches in pregnancy and postpartum. May 2022 [internet publication].
https://journals.lww.com/greenjournal/abstract/2022/05000/headaches_in_pregnancy_and_postpartum__acog.37.aspx
http://www.ncbi.nlm.nih.gov/pubmed/35576364?tool=bestpractice.com
[56]Gold KJ, Barnes C, Lalley J, et al. Case report: late-onset eclampsia presents as bilateral cortical blindness. Am Fam Physician. 2005 Mar 1;71(5):856, 858, 861.
https://www.aafp.org/pubs/afp/issues/2005/0301/p856a.html
http://www.ncbi.nlm.nih.gov/pubmed/15768615?tool=bestpractice.com
The headache typically develops in temporal relation to the onset of pre-eclampsia, or substantially worsens or improves in parallel with worsening or improvement of pre-eclampsia.[55]American College of Obstetricians and Gynecologists. Clinical practice guideline no. 3: headaches in pregnancy and postpartum. May 2022 [internet publication].
https://journals.lww.com/greenjournal/abstract/2022/05000/headaches_in_pregnancy_and_postpartum__acog.37.aspx
http://www.ncbi.nlm.nih.gov/pubmed/35576364?tool=bestpractice.com
In the setting of pre-eclampsia and headache, it is important to consider alternative secondary aetiologies (e.g., reversible cerebral vasoconstriction syndrome, posterior reversible encephalopathy syndrome, or infection) if accompanied by an altered level of consciousness, vomiting, or fever.[55]American College of Obstetricians and Gynecologists. Clinical practice guideline no. 3: headaches in pregnancy and postpartum. May 2022 [internet publication].
https://journals.lww.com/greenjournal/abstract/2022/05000/headaches_in_pregnancy_and_postpartum__acog.37.aspx
http://www.ncbi.nlm.nih.gov/pubmed/35576364?tool=bestpractice.com
Physical examination
An appropriately sized cuff should be used for blood pressure (BP) readings, so that the bladder encircles 80% of the arm.[1]Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018 May 15;71(19):e127-248.
https://www.sciencedirect.com/science/article/pii/S0735109717415191?via%3Dihub
http://www.ncbi.nlm.nih.gov/pubmed/29146535?tool=bestpractice.com
[57]Mancia G, Kreutz R, Brunström M, et al. 2023 ESH Guidelines for the management of arterial hypertension the Task Force for the management of arterial hypertension of the European Society of Hypertension: endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J Hypertens. 2023;41(12):1874-2071.
https://journals.lww.com/jhypertension/fulltext/2023/12000/2023_esh_guidelines_for_the_management_of_arterial.2.aspx
http://www.ncbi.nlm.nih.gov/pubmed/37345492?tool=bestpractice.com
The arm should be supported at heart level during recordings. Using too large a cuff could result in an underestimation of BP; conversely, too small a cuff could lead to over-estimation. It should be noted if a larger- or smaller-than-normal cuff size is used.[1]Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018 May 15;71(19):e127-248.
https://www.sciencedirect.com/science/article/pii/S0735109717415191?via%3Dihub
http://www.ncbi.nlm.nih.gov/pubmed/29146535?tool=bestpractice.com
BP readings should be taken from both arms.[7]Bress AP, Anderson TS, Flack JM, et al. The management of elevated blood pressure in the acute care setting: a scientific statement from the American Heart Association. Hypertension. 2024 Aug;81(8):e94-106.
https://www.ahajournals.org/doi/full/10.1161/HYP.0000000000000238
http://www.ncbi.nlm.nih.gov/pubmed/38804130?tool=bestpractice.com
[54]Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension Global Hypertension practice guidelines. Hypertension. 2020 Jun;75(6):1334-57.
https://www.ahajournals.org/doi/full/10.1161/HYPERTENSIONAHA.120.15026
http://www.ncbi.nlm.nih.gov/pubmed/32370572?tool=bestpractice.com
Readings should be repeated after 5 minutes to confirm. If there is a more than 20 mmHg pressure difference between arms, aortic dissection should be considered.[58]Bossone E, Rampoldi V, Nienaber CA, et al. Usefulness of pulse deficit to predict in-hospital complications and mortality in patients with acute type A aortic dissection. Am J Cardiol. 2002 Apr 1;89(7):851-5.
http://www.ncbi.nlm.nih.gov/pubmed/11909573?tool=bestpractice.com
[59]Ranasinghe AM, Strong D, Boland B, et al. Acute aortic dissection. BMJ. 2011 Jul 29;343:d4487.
http://www.ncbi.nlm.nih.gov/pubmed/21803810?tool=bestpractice.com
If blood pressure is elevated, a second measurement should be taken.[60]National Institute for Health and Care Excellence. Hypertension in adults: diagnosis and management. Nov 2023 [internet publication].
https://www.nice.org.uk/guidance/ng136
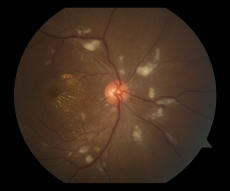
A fundoscopic examination should be performed, with the aid of slit lamp examination and pupillary mydriasis if necessary, looking for the presence of arteriolar spasm, retinal oedema, retinal haemorrhages, retinal exudates, papilloedema, or engorged retinal veins.[7]Bress AP, Anderson TS, Flack JM, et al. The management of elevated blood pressure in the acute care setting: a scientific statement from the American Heart Association. Hypertension. 2024 Aug;81(8):e94-106.
https://www.ahajournals.org/doi/full/10.1161/HYP.0000000000000238
http://www.ncbi.nlm.nih.gov/pubmed/38804130?tool=bestpractice.com
[18]Kulkarni S, Glover M, Kapil V, et al. Management of hypertensive crisis: British and Irish Hypertension Society Position document. J Hum Hypertens. 2023 Oct;37(10):863-79.
https://www.nature.com/articles/s41371-022-00776-9
http://www.ncbi.nlm.nih.gov/pubmed/36418425?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Fundus photograph of the right eye with multiple dot-blot haemorrhages typical of hypertensive retinopathyCourtesy Angie Wen MD, Attending Faculty, New York Eye and Ear Infirmary, New York; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Fundus photograph of the left eye with multiple cotton-wool spots typical of hypertensive retinopathyCourtesy Angie Wen MD, Attending Faculty, New York Eye and Ear Infirmary, New York; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Fundus photograph of the left eye with multiple cotton-wool spots typical of hypertensive retinopathyCourtesy Angie Wen MD, Attending Faculty, New York Eye and Ear Infirmary, New York; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Fundus photograph of the right eye centred on the optic nerve, showing multiple cotton-wool spots and macular exudates in a radiating star configuration around the foveaCourtesy Angie Wen MD, Attending Faculty, New York Eye and Ear Infirmary, New York; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Fundus photograph of the right eye centred on the optic nerve, showing multiple cotton-wool spots and macular exudates in a radiating star configuration around the foveaCourtesy Angie Wen MD, Attending Faculty, New York Eye and Ear Infirmary, New York; used with permission [Citation ends].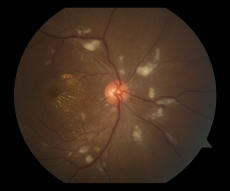
A rapid bedside neurological examination is also required, including testing cognition, cranial nerve function, dysarthria, motor strength, gross sensory function, upper extremity pronator drift, and gait.
Cardiopulmonary status should be assessed, examining in particular for the presence of new murmurs, friction rubs, additional heart sounds, lateral displacement of the apex beat, jugular venous distension, carotid or renal artery bruits, rales, and lower extremity oedema.
Abdominal examination should be performed. Tenderness to palpation in the right upper quadrant is seen in severe pre-eclampsia and HELLP (haemolysis, elevated liver enzymes, low platelets) syndrome.[61]National Institute for Health and Care Excellence. Hypertension in pregnancy: diagnosis and management. Apr 2023 [internet publication].
https://www.nice.org.uk/guidance/ng133
[62]Turner JA. Diagnosis and management of pre-eclampsia: an update. Int J Womens Health. 2010 Sep 30;2:327-37.
https://www.dovepress.com/diagnosis-and-management-of-pre-eclampsia-an-update-peer-reviewed-fulltext-article-IJWH
http://www.ncbi.nlm.nih.gov/pubmed/21151680?tool=bestpractice.com
Phaeochromocytoma may be associated with an abdominal mass.
Renovascular hypertension should be suspected in patients with severe hypertension who have abdominal bruits and/or unexplained renal deterioration with angiotensin-converting enzyme inhibitor treatment, although the clinical presentation is variable.
During pregnancy, hypertension in a previously normotensive woman with proteinuria or evidence of systemic involvement (e.g., renal insufficiency, impaired liver function, neurological complications, haematological complications) is diagnostic of pre-eclampsia.[48]American College of Obstetricians and Gynecologists. Practice bulletin no. 222: gestational hypertension and preeclampsia. Jun 2020 [internet publication].
https://journals.lww.com/greenjournal/abstract/2020/06000/gestational_hypertension_and_preeclampsia__acog.44.aspx
http://www.ncbi.nlm.nih.gov/pubmed/32443077?tool=bestpractice.com
[61]National Institute for Health and Care Excellence. Hypertension in pregnancy: diagnosis and management. Apr 2023 [internet publication].
https://www.nice.org.uk/guidance/ng133
Pre-eclampsia should be considered in patients with headache who are at least 20 0/7 weeks of gestation, or within 6 weeks postnatally, and who have blood pressure ≥140 mmHg systolic or ≥90 mmHg diastolic.[55]American College of Obstetricians and Gynecologists. Clinical practice guideline no. 3: headaches in pregnancy and postpartum. May 2022 [internet publication].
https://journals.lww.com/greenjournal/abstract/2022/05000/headaches_in_pregnancy_and_postpartum__acog.37.aspx
http://www.ncbi.nlm.nih.gov/pubmed/35576364?tool=bestpractice.com
At least two measurements should be made, at least 4 hours apart.[48]American College of Obstetricians and Gynecologists. Practice bulletin no. 222: gestational hypertension and preeclampsia. Jun 2020 [internet publication].
https://journals.lww.com/greenjournal/abstract/2020/06000/gestational_hypertension_and_preeclampsia__acog.44.aspx
http://www.ncbi.nlm.nih.gov/pubmed/32443077?tool=bestpractice.com
The neurological examination is typically normal in pre-eclampsia.[55]American College of Obstetricians and Gynecologists. Clinical practice guideline no. 3: headaches in pregnancy and postpartum. May 2022 [internet publication].
https://journals.lww.com/greenjournal/abstract/2022/05000/headaches_in_pregnancy_and_postpartum__acog.37.aspx
http://www.ncbi.nlm.nih.gov/pubmed/35576364?tool=bestpractice.com
See Pre-eclampsia (Diagnostic approach).
Laboratory evaluation
Baseline blood and urine samples must be collected prior to administration of treatment. Laboratory evaluation should include the following:[7]Bress AP, Anderson TS, Flack JM, et al. The management of elevated blood pressure in the acute care setting: a scientific statement from the American Heart Association. Hypertension. 2024 Aug;81(8):e94-106.
https://www.ahajournals.org/doi/full/10.1161/HYP.0000000000000238
http://www.ncbi.nlm.nih.gov/pubmed/38804130?tool=bestpractice.com
[18]Kulkarni S, Glover M, Kapil V, et al. Management of hypertensive crisis: British and Irish Hypertension Society Position document. J Hum Hypertens. 2023 Oct;37(10):863-79.
https://www.nature.com/articles/s41371-022-00776-9
http://www.ncbi.nlm.nih.gov/pubmed/36418425?tool=bestpractice.com
[54]Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension Global Hypertension practice guidelines. Hypertension. 2020 Jun;75(6):1334-57.
https://www.ahajournals.org/doi/full/10.1161/HYPERTENSIONAHA.120.15026
http://www.ncbi.nlm.nih.gov/pubmed/32370572?tool=bestpractice.com
Blood chemistry panel, including creatinine and electrolytes
Full blood count, including peripheral blood smear
Urinalysis with microscopy.
In some circumstances, the following may also be indicated:
Liver function tests, if pre-eclampsia or HELLP (haemolysis, elevated liver enzymes, low platelets) syndrome are suspected.[48]American College of Obstetricians and Gynecologists. Practice bulletin no. 222: gestational hypertension and preeclampsia. Jun 2020 [internet publication].
https://journals.lww.com/greenjournal/abstract/2020/06000/gestational_hypertension_and_preeclampsia__acog.44.aspx
http://www.ncbi.nlm.nih.gov/pubmed/32443077?tool=bestpractice.com
[61]National Institute for Health and Care Excellence. Hypertension in pregnancy: diagnosis and management. Apr 2023 [internet publication].
https://www.nice.org.uk/guidance/ng133
Cardiac enzymes and/or brain natriuretic peptide, if acute coronary syndrome or acute heart failure is suspected.[18]Kulkarni S, Glover M, Kapil V, et al. Management of hypertensive crisis: British and Irish Hypertension Society Position document. J Hum Hypertens. 2023 Oct;37(10):863-79.
https://www.nature.com/articles/s41371-022-00776-9
http://www.ncbi.nlm.nih.gov/pubmed/36418425?tool=bestpractice.com
Coagulation profile, if disseminated intravascular coagulation is suspected.[18]Kulkarni S, Glover M, Kapil V, et al. Management of hypertensive crisis: British and Irish Hypertension Society Position document. J Hum Hypertens. 2023 Oct;37(10):863-79.
https://www.nature.com/articles/s41371-022-00776-9
http://www.ncbi.nlm.nih.gov/pubmed/36418425?tool=bestpractice.com
Urine or serum pregnancy test (in women of childbearing age not known to be pregnant).[18]Kulkarni S, Glover M, Kapil V, et al. Management of hypertensive crisis: British and Irish Hypertension Society Position document. J Hum Hypertens. 2023 Oct;37(10):863-79.
https://www.nature.com/articles/s41371-022-00776-9
http://www.ncbi.nlm.nih.gov/pubmed/36418425?tool=bestpractice.com
A urine drug screen, if illicit drug use is suspected.[63]Cífková R, Johnson MR, Kahan T, et al. Peripartum management of hypertension: a position paper of the ESC Council on Hypertension and the European Society of Hypertension. Eur Heart J Cardiovasc Pharmacother. 2020 Nov 1;6(6):384-93.
https://academic.oup.com/ehjcvp/article/6/6/384/5678784
http://www.ncbi.nlm.nih.gov/pubmed/31841131?tool=bestpractice.com
Plasma renin activity and aldosterone levels, if primary aldosteronism is suspected (e.g., in patients with diastolic hypertension with persistent hypokalaemia and metabolic alkalosis).
Spot urine or plasma-free metanephrine levels, if phaeochromocytoma is suspected (e.g., in patients with hypertension and palpitations, headaches, and/or diaphoresis, although clinical presentation is very variable).[18]Kulkarni S, Glover M, Kapil V, et al. Management of hypertensive crisis: British and Irish Hypertension Society Position document. J Hum Hypertens. 2023 Oct;37(10):863-79.
https://www.nature.com/articles/s41371-022-00776-9
http://www.ncbi.nlm.nih.gov/pubmed/36418425?tool=bestpractice.com
[63]Cífková R, Johnson MR, Kahan T, et al. Peripartum management of hypertension: a position paper of the ESC Council on Hypertension and the European Society of Hypertension. Eur Heart J Cardiovasc Pharmacother. 2020 Nov 1;6(6):384-93.
https://academic.oup.com/ehjcvp/article/6/6/384/5678784
http://www.ncbi.nlm.nih.gov/pubmed/31841131?tool=bestpractice.com
These tests need to be interpreted carefully, with consideration for possible confounding factors such as drugs (e.g., tricyclic antidepressants, clozapine, phenoxybenzamine, beta-blockers, sympathomimetics, buspirone), or major physiological stress.
Thyroid function tests, if signs of hypo- or hyperthyroidism.
24-hour urinary free cortisol, if Cushing syndrome is suspected.
Sleep study, in cases of resistant hypertension and for patients with signs or symptoms of obstructive sleep apnoea.[34]Yeghiazarians Y, Jneid H, Tietjens JR, et al. Obstructive sleep apnea and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2021 Jul 20;144(3):e56-67.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000988?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org
http://www.ncbi.nlm.nih.gov/pubmed/34148375?tool=bestpractice.com
Further investigation
ECG and chest x-ray should be strongly considered.[7]Bress AP, Anderson TS, Flack JM, et al. The management of elevated blood pressure in the acute care setting: a scientific statement from the American Heart Association. Hypertension. 2024 Aug;81(8):e94-106.
https://www.ahajournals.org/doi/full/10.1161/HYP.0000000000000238
http://www.ncbi.nlm.nih.gov/pubmed/38804130?tool=bestpractice.com
[54]Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension Global Hypertension practice guidelines. Hypertension. 2020 Jun;75(6):1334-57.
https://www.ahajournals.org/doi/full/10.1161/HYPERTENSIONAHA.120.15026
http://www.ncbi.nlm.nih.gov/pubmed/32370572?tool=bestpractice.com
If aortic dissection is considered possible, urgent thoracic computed tomography angiography (CTA) scan with contrast is recommended.[64]Bossone E, LaBounty TM, Eagle KA. Acute aortic syndromes: diagnosis and management, an update. Eur Heart J. 2018 Mar 1;39(9):739-49d.
https://academic.oup.com/eurheartj/article/39/9/739/3904550
http://www.ncbi.nlm.nih.gov/pubmed/29106452?tool=bestpractice.com
[65]Writing Committee Members, Isselbacher EM, Preventza O, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on clinical practice guidelines. J Am Coll Cardiol. 2022 Dec 13;80(24):e223-393.
https://www.sciencedirect.com/science/article/pii/S0735109722057692
http://www.ncbi.nlm.nih.gov/pubmed/36334952?tool=bestpractice.com
For patients who cannot receive iodinated contrast, computed tomography (CT) without contrast is an acceptable alternative. Transthoracic echocardiography (TTE) may be used in the accident and emergency department, intensive care unit (ICU), or operating room for acute proximal dissections if the patient is clinically unstable and there is any question about the diagnosis, or if CTA is unavailable or contraindicated.[64]Bossone E, LaBounty TM, Eagle KA. Acute aortic syndromes: diagnosis and management, an update. Eur Heart J. 2018 Mar 1;39(9):739-49d.
https://academic.oup.com/eurheartj/article/39/9/739/3904550
http://www.ncbi.nlm.nih.gov/pubmed/29106452?tool=bestpractice.com
[65]Writing Committee Members, Isselbacher EM, Preventza O, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on clinical practice guidelines. J Am Coll Cardiol. 2022 Dec 13;80(24):e223-393.
https://www.sciencedirect.com/science/article/pii/S0735109722057692
http://www.ncbi.nlm.nih.gov/pubmed/36334952?tool=bestpractice.com
See Aortic dissection.
In clinical situations with high suspicion for renal artery disease, the use of doppler ultrasound, usually recommended as first-line imaging. This may be followed by magnetic resonance angiography and/or CTA.[66]Aboyans V, Ricco JB, Bartelink MEL, et al. 2017 ESC guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the European Society for Vascular Surgery (ESVS): document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO)The Task Force for the diagnosis and treatment of peripheral arterial diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur Heart J. 2018 Mar 1;39(9):763-816.
https://academic.oup.com/eurheartj/article/39/9/763/4095038
http://www.ncbi.nlm.nih.gov/pubmed/28886620?tool=bestpractice.com
Due to the potential risks with invasive procedures, angiography is generally limited to visualisation and quantification of the stenosis before vascular intervention.[66]Aboyans V, Ricco JB, Bartelink MEL, et al. 2017 ESC guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the European Society for Vascular Surgery (ESVS): document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO)The Task Force for the diagnosis and treatment of peripheral arterial diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur Heart J. 2018 Mar 1;39(9):763-816.
https://academic.oup.com/eurheartj/article/39/9/763/4095038
http://www.ncbi.nlm.nih.gov/pubmed/28886620?tool=bestpractice.com
If ischaemic stroke or intracranial haemorrhage is suspected (e.g., in patients with decreased consciousness or those with focal neurological deficits), an urgent non-contrast CT scan of the head and/or a magnetic resonance imaging scan should be requested, depending on local availability.[18]Kulkarni S, Glover M, Kapil V, et al. Management of hypertensive crisis: British and Irish Hypertension Society Position document. J Hum Hypertens. 2023 Oct;37(10):863-79.
https://www.nature.com/articles/s41371-022-00776-9
http://www.ncbi.nlm.nih.gov/pubmed/36418425?tool=bestpractice.com
Typically patients initially undergo a non-contrast head CT, in order to exclude a brain haemorrhage and guide treatment.[67]Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019 Dec;50(12):e344-418.
https://www.ahajournals.org/doi/10.1161/STR.0000000000000211
http://www.ncbi.nlm.nih.gov/pubmed/31662037?tool=bestpractice.com
The mismatch between diffusion-weighted imaging and fluid-attenuated inversion recovery findings on magnetic resonance imaging (MRI) can be useful for selecting those who may benefit from intravenous thrombolysis.[67]Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019 Dec;50(12):e344-418.
https://www.ahajournals.org/doi/10.1161/STR.0000000000000211
http://www.ncbi.nlm.nih.gov/pubmed/31662037?tool=bestpractice.com
However, MRI may take more than 30 minutes to complete, and is not universally available. See Ischaemic stroke and Stroke due to spontaneous intracerebral haemorrhage.
The American College of Obstetricians and Gynecologists recommends evaluating headaches in pregnancy that warrant brain or vascular imaging with magnetic resonance techniques that limit the use of gadolinium.[55]American College of Obstetricians and Gynecologists. Clinical practice guideline no. 3: headaches in pregnancy and postpartum. May 2022 [internet publication].
https://journals.lww.com/greenjournal/abstract/2022/05000/headaches_in_pregnancy_and_postpartum__acog.37.aspx
http://www.ncbi.nlm.nih.gov/pubmed/35576364?tool=bestpractice.com
 [Figure caption and citation for the preceding image starts]: Fundus photograph of the left eye with multiple cotton-wool spots typical of hypertensive retinopathyCourtesy Angie Wen MD, Attending Faculty, New York Eye and Ear Infirmary, New York; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Fundus photograph of the left eye with multiple cotton-wool spots typical of hypertensive retinopathyCourtesy Angie Wen MD, Attending Faculty, New York Eye and Ear Infirmary, New York; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Fundus photograph of the right eye centred on the optic nerve, showing multiple cotton-wool spots and macular exudates in a radiating star configuration around the foveaCourtesy Angie Wen MD, Attending Faculty, New York Eye and Ear Infirmary, New York; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Fundus photograph of the right eye centred on the optic nerve, showing multiple cotton-wool spots and macular exudates in a radiating star configuration around the foveaCourtesy Angie Wen MD, Attending Faculty, New York Eye and Ear Infirmary, New York; used with permission [Citation ends].