Investigations
1st investigations to order
ultrasound with colour Doppler of testis
Test
First-line test in patients with newly diagnosed palpable scrotal abnormality.[2][45][46]
Ultrasound should be carried out with colour Doppler assessment to confirm the presence of a testicular mass before orchiectomy.[47] Use of colour Doppler can help to distinguish from other testicular swellings (e.g., varicocele).[48]
The contralateral testis should also be evaluated for the presence of synchronous tumours and microcalcifications, and to measure the testicular volume.[47]
Ultrasound should be repeated in 6-8 weeks in patients with indeterminate findings on ultrasound and normal serum tumour markers.[2]
Result
testicular mass
chest imaging
Test
Essential for accurate staging work-up.[2][52] Chest x-ray is advised as first-line chest imaging for clinical stage I seminoma only. CT chest is recommended as first-line for other tumour types, or those with rising post-orchiectomy serum tumour markers, or with evidence of metastases on abdominal/pelvic imaging, chest x-ray, or physical examination.[2]
Result
mediastinal or lung mass suggestive of metastasis
CT scan abdomen and pelvis with contrast
serum beta-human chorionic gonadotrophin (beta-hCG)
Test
Using ultra-sensitive assays, the upper reference limit for men under 50 years of age is 0.7 IU/L.
Can be highly elevated in choriocarcinoma.
Elevations in pure seminoma are usually <300 IU/L.[53]
Result
>0.7 IU/L
serum alpha-fetoprotein (AFP)
Test
Half-life is 5 to 7 days, and the level should return to normal within 25 to 35 days of tumour removal.
Can be elevated by embryonal carcinoma, teratoma, yolk sac tumours, or mixed tumours.
Pure choriocarcinomas and seminomas are not associated with elevated AFP levels.
Result
>25 microgram/L (>25 ng/mL)
serum lactate dehydrogenase (LDH)
histological examination of testicular mass post-orchiectomy
Test
A biopsy is generally not advised in the evaluation of a testicular mass; diagnosis is established by removing and examining the involved testicle. Should be performed early in evaluation.
[Figure caption and citation for the preceding image starts]: Metastatic seminoma. Left image: H&E stain low power. Right image placental alkaline phosphatase (PLAP) stain high power. The H&E image shows nests of malignant cells with clear cytoplasm; the tumour cells are strongly positive for PLAP confirming the diagnosisLaw C et al. BMJ Case Rep. 2020 Apr 22;13(4):e233368. doi: 10.1136/bcr-2019-233368; used with permission [Citation ends].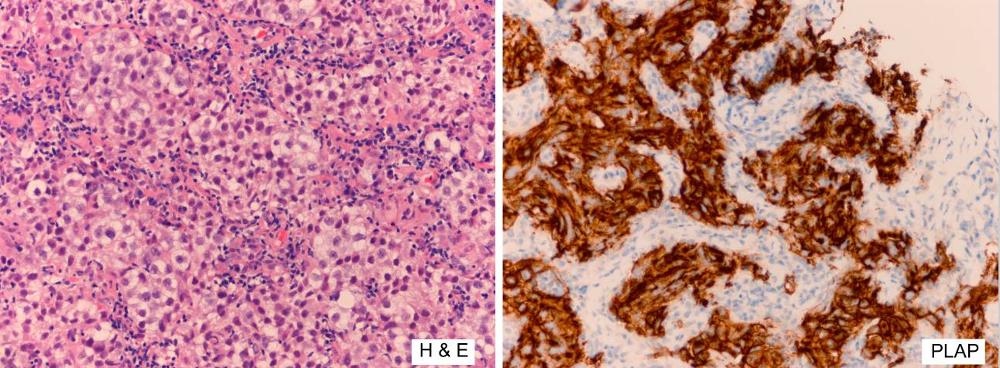 [Figure caption and citation for the preceding image starts]: Non-seminomaFrom the collection of Dr Francisco G. La Rosa; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Non-seminomaFrom the collection of Dr Francisco G. La Rosa; used with permission [Citation ends].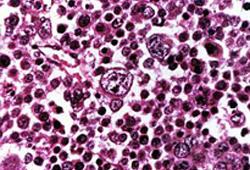
Result
confirms histology of testicular mass
Investigations to consider
serum placental alkaline phosphatase
Test
Normal ranges vary according to the specific assay used.
Elevated in up to 40% of patients with advanced disease.[53]
Result
elevated
MRI abdomen and pelvis
Test
May be useful as an alternative modality to CT, if CT is inconclusive or the contrast media is contraindicated due to patient allergy or renal insufficiency.
Result
staging tool
CT scan chest
Test
Staging tool, if not already done as first-line investigation. Recommended for those with rising post-orchiectomy serum tumour markers, or with evidence of metastases on initial chest x-ray, abdominal/pelvic imaging, or physical examination.[2]
Result
mediastinal or lung mass suggestive of metastasis
biopsy of contralateral testis
Test
Biopsy of the contralateral testis may be indicated if a suspicious mass is identified during ultrasound, the testis is atrophied, or there is a history of cryptorchidism. Biopsy is not recommended for testicular microcalcifications alone.[46][49][50]
Result
assessment for germ cell neoplasia in situ or metachronous germ cell tumour in contralateral testis
Use of this content is subject to our disclaimer