History and exam
Key diagnostic factors
common
fever >38°C
Virtually all patients with rickettsial infection are febrile.
rash
Rash is common in all rickettsial infections but is not present for the first few days of the infection. In most cases it takes about 1 week for the rash to develop. In people with darker skin the rash may be difficult to see. It is usually macular or papular but in some rickettsial infections may be vesicular (e.g., Queensland tick typhus due to Rickettsia australis and rickettsial pox due to R akari) or petechial (e.g., epidemic typhus due to R prowazekii).[Figure caption and citation for the preceding image starts]: Characteristic rash (in this case caused by Rocky Mountain spotted fever)CDC Public Health Image Library [Citation ends].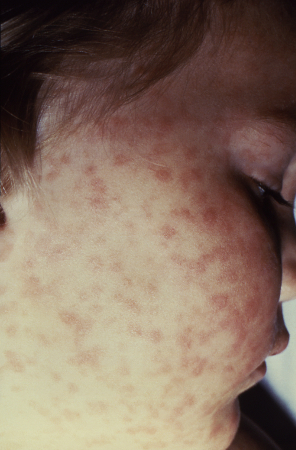
uncommon
eschar
Whether an eschar is present or not is highly variable from patient to patient, and from geographic place to place, and varies according to the Rickettsia species or Orientia tsutsugamushi strain involved. Sometimes it is present but located on a part of the body difficult to examine (e.g., hair, under scrotum, natal cleft, under breasts, groin). When present it is a very good prognostic indicator of a rickettsial infection.
lymphadenopathy associated with eschar
This sign depends on the virulence of the species of rickettsia causing the infection at the arthropod inoculation site (the eschar). More virulent rickettsia provoke greater regional lymphadenopathy, which may be palpable.
Other diagnostic factors
common
uncommon
hepatosplenomegaly
Patients may have hepatosplenomegaly.[22]
tachypnoea
Patients may be tachypnoeic.
Risk factors
strong
exposure to human body lice
People living in poverty, especially in cold climates, may be infested with the human body louse. The louse can often be detected in the seams of their clothing. If the lice are infected with Rickettsia prowazekii then the patient probably has epidemic typhus.[6]
exposure to rodents (rats and mice) and their fleas
These patients are often people living in poor economic circumstances or in sub-standard housing where there are rodents present. The rodent fleas may be infected with Rickettsia typhi leading to infection by inhalation of the flea faeces (most commonly) or via inoculation of the flea bite site with the flea faeces (less commonly). The infection, murine typhus, is also called endemic typhus.[2]
tick bites
Patients may not recall having been bitten by a tick, and the bite may have been many days ago and the tick no longer attached. There is a wide variety of rickettsial infections that are tick transmitted, with different rickettsial species involved, most of which are members of the spotted fever group. Many different tick species, in many different parts of the world, may be involved in this infection.[1] CDC: tick ID Opens in new window
mite bites
The larval form of a specific mite carries the rickettsia (Orientia tsutsugamushi, O chuto, O chiloensis) that causes scrub typhus. R akari is also carried by mites and causes rickettsialpox.[2]
weak
travel to the tropics
Patients exposed to ectoparasites as part of their tropical travel are often predisposed to rickettsial infection. These patients have often been in environmental situations where they were exposed to rickettsial infections, either through their (poor) living conditions or holiday activities (e.g., game safaris).
exposure to natural vegetation, forests, scrub, bush
Ticks live on vegetation and in most parts of the world they attach to people who are passing through the vegetation.
exposure to cat or dog fleas
Cat and dog fleas in most parts of the world carry a rickettsia, Rickettsia felis. A person bitten by such an infected flea is likely to develop cat-flea rickettsiosis (also known as flea-borne spotted fever).
Use of this content is subject to our disclaimer