Investigations
1st investigations to order
blood cultures
Test
Obtain three sets of blood cultures from different venepuncture sites taken at 30-minute intervals prior to the initiation of antibiotic therapy.[7]
If the patient is unwell (e.g., with sepsis) do not delay empirical antibiotic therapy while waiting to take three sets of blood cultures.[27] The volume of blood sent for culture is more important than the number of sets of cultures.[34]
Use peripheral venepuncture sites and a meticulous sterile technique to minimise risk of contamination and a misleading result.[7] Take a 10 mL blood sample for each aerobic and anaerobic bottle.[28]
In practice, if the patient has a central venous catheter (CVC), take blood cultures from the CVC in addition to peripheral venepuncture sites because IE may be caused by infection of the CVC. Consider removing the CVC if the patient is bacteraemic.
When a micro-organism has been identified, repeat the blood cultures after 48 to 72 hours to check the effectiveness of treatment.[7]
Seek advice from an infectious disease or microbiology specialist microbiologist if the blood cultures are negative after 48 hours but there is ongoing clinical suspicion of IE.[7] The most common cause of culture-negative endocarditis is antibiotic therapy preceding blood cultures.[44] Blood culture-negative IE (no causative micro-organism grown using standard blood culture methods) requires more specialist investigation (e.g., systematic serological testing and blood polymerase chain reaction).[7]
Always consider IE if the patient has Staphylococcus aureus bacteraemia.[7] IE is highly prevalent in these patients and S aureus can cause devastating effects once infection is established.[7]
Result
bacteraemia; fungaemia
echocardiography
Test
Order echocardiography if you suspect IE.[7][35] Echocardiography is important not only for confirming or ruling out the diagnosis but also for evaluation of complications and prognosis. The choice between transthoracic echocardiography (TTE) and trans-oesophageal echocardiography (TOE) is often difficult and continues to be the subject of debate.[7][35][36][37] The European Society of Cardiology recommends that:[7]
Any patient suspected of having native valve IE should be screened with TTE
TOE is the preferred form of echocardiography in people with a prosthetic valve or intracardiac device that have suspected IE.[35] TOE is also indicated, in addition to TTE, if:
TTE is positive, unless the patient has isolated right-sided native valve IE with good-quality TTE examination and unequivocal echocardiographic findings
TTE is negative or non-diagnostic but there is high clinical suspicion of IE[35]
If the patient has Staphylococcus aureus bacteraemia, base the decision to use TTE and TOE on individual patient risk factors and the mode of acquisition of S aureus bacteraemia.
[Figure caption and citation for the preceding image starts]: Image from transoesophageal echocardiogram. White arrow indicates vegetation on the patient's aortic valveTeoh LS, Hart HH, Soh MC, et al. Bartonella henselae aortic valve endocarditis mimicking systemic vasculitis. BMJ Case Rep. 2010 Oct 21;2010. pii: bcr0420102945 [Citation ends]. [Figure caption and citation for the preceding image starts]: A transthoracic echo showing large mobile vegetations on the anterior and posterior leaflets of the tricuspid valveFoley JA, Augustine D, Bond R, et al. Lost without Occam's razor: Escherichia coli tricuspid valve endocarditis in a non-intravenous drug user. BMJ Case Rep. 2010 Aug 10;2010. pii: bcr0220102769 [Citation ends].
[Figure caption and citation for the preceding image starts]: A transthoracic echo showing large mobile vegetations on the anterior and posterior leaflets of the tricuspid valveFoley JA, Augustine D, Bond R, et al. Lost without Occam's razor: Escherichia coli tricuspid valve endocarditis in a non-intravenous drug user. BMJ Case Rep. 2010 Aug 10;2010. pii: bcr0220102769 [Citation ends].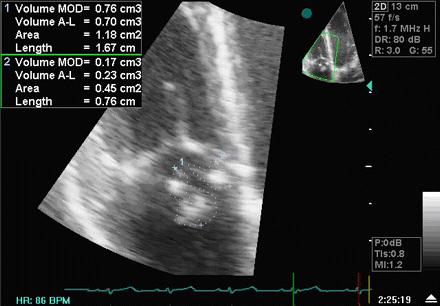
Repeat TTE and/or TOE within 5 to 7 days (or earlier if S aureus bacteraemia is present) for any patient with negative initial echocardiography but where clinical suspicion of IE remains high.[7]
Result
valvular, mobile vegetations
full blood count
Test
Most patients have a normocytic, normochromic anaemia. Leukocytosis is seen in about one third of patients with IE, often with neutrophilia.
Result
anaemia; leukocytosis
C-reactive protein
Test
Non-specific test. High in almost all patients.[45]
In practice, C-reactive protein is useful as a baseline test and to monitor response to treatment.
Result
markedly elevated
serum urea, electrolytes, and glucose
Test
Provides baseline assessment.
Result
normal or elevated urea
liver function tests
Test
Provides baseline assessment.
Result
normal or elevated
urinalysis
Test
Septic emboli are common complications of IE, and urinalysis may demonstrate active sediment assisting in the clinical diagnosis.
Result
microscopic haematuria; RBC casts; WBC casts; proteinuria; pyuria
ECG
Test
Record an ECG; progression of the infection may lead to conduction abnormalities.[38]
Conduction abnormalities secondary to IE (mainly first-, second-, and third-degree atrioventricular [AV] block) are uncommon but are associated with worse prognosis and higher mortality compared with patients without conduction abnormalities.[39]
Result
prolonged PR interval; non-specific ST/T wave abnormalities; AV block
Investigations to consider
rheumatoid factor/other immunological blood tests
Test
Check your local protocols for guidance on the most appropriate immunological blood tests to use. The European Society of Cardiology recommends considering rheumatoid factor (which forms part of the Duke criteria – see the Criteria section) and antinuclear antibodies.[7] Some centres (e.g., in the UK) may use anti-cyclic citrullinated peptides (anti-CCP) instead of rheumatoid factor.
Result
may be positive
erythrocyte sedimentation rate
Test
Non-specific marker of infection, but rarely used in practice. High in almost all patients.
Result
markedly elevated
complement levels
Test
May be performed if autoimmune infective endocarditis is suspected, but rarely used in practice.
Result
decreased
computed tomography
Test
CT imaging is used for the diagnosis of native and prosthetic valve IE and for detection of complications of IE, including abscesses, pseudoaneurysms, and fistulae. Cardiac CT has been found to compare favourably with transthoracic echocardiography in detecting valvular abnormalities in patients with IE, but it may miss small defects (e.g., small leaflet perforations [≤2 mm diameter], small vegetations <10 mm).[7][40] Cardiac CT is also used to assess the coronary arteries prior to cardiac surgery.[7]
Whole-body and brain CT can be used to look for distant lesions, systemic complications of IE, and septic emboli, as well as having a role in detecting extracardiac sources of bacteraemia and potentially alternate diagnoses in patients where IE has been excluded.[7] CT angiography is a sensitive and specific test for detecting mycotic arterial aneurysms; MRI is superior for assessment of neurological complications in terms of imaging, but is limited by accessibility and availability.
Result
valvular abnormalities and vegetations
magnetic resonance imaging
Test
MRI is of less diagnostic value than CT, but is the imaging modality of choice when investigating the cerebral complications of IE, with studies consistently reporting cerebral infarcts in up to 80% of patients.[7][41] MRI also reveals cerebral lesions in 50% of patients who do not demonstrate neurological symptoms.[42] MRI is also used to assess spinal involvement in IE, including spondylodiscitis and vertebral osteomyelitis.[7]
Result
may show cerebral lesions, spinal involvement
nuclear imaging and photon emission tomography (PET)
Test
18F-FDG-PET/CT and WBC single-photon emission CT (SPECT) are used in cases of suspected prosthetic valve IE where echocardiography is not diagnostic.[7]
Whole-body imaging with 18F-FDG-PET/CT can be useful to detect distant lesions, mycotic aneurysms, and portal of entry of bacteria, and to monitor response to antibiotic treatment in patients for whom surgery is being considered.[7]
Result
may reveal distant lesions, mycotic aneurysms, portal of bacterial entry; used to monitor response to antibiotic treatment
Use of this content is subject to our disclaimer