Approach
Carotid artery stenosis is the most common preventable cause of stroke. Because one of the major goals of management is the prevention of stroke, the identification of individuals with carotid stenosis is an important objective. In the presence of neurological symptoms, the focus is on preventing a recurrent stroke or transient ischaemic attack (TIA). In view of its low cost, ready availability, and relative accuracy, carotid duplex ultrasonography is the mainstay of screening, initial imaging, and, in some instances, is the only imaging modality utilised for the workup of carotid stenosis. However, with the emergence of mechanical thrombectomy as a treatment option for acute stroke, detailed evaluation of the extra- and intracranial vasculature is becoming more routine in patients presenting with strokes. Hence, contrast-enhanced computed tomography angiography (CTA) and magnetic resonance angiography (MRA) are increasingly used alternatives and have the advantage of imaging the full length of the carotid arteries. Other important considerations in the diagnosis include determining the degree of stenosis and assessing the presence of ischaemic injury to the brain.
History and physical examination
Most people with carotid artery stenosis are asymptomatic. The most frequent reason for suspecting the diagnosis is the presence of atherosclerotic high-risk factors. However, even though a cervical bruit is not a sensitive or specific sign (it is associated with carotid artery stenosis of any severity in 47% of patients), its presence often prompts evaluation for the condition.[20]
Auscultation: Carotid bruit
High-risk factors include:[14]
peripheral arterial occlusive disease
coronary artery bypass surgery
aged ≥55 years with at least two traditional atherosclerotic risk factors
hypertension, diabetes, or coronary artery disease
aged ≥55 years with active smoking
clinically occult cerebral infarction noted on imaging studies.
The patient should be assessed for the presence of focal neurological deficits. The presence of deficits (e.g., sudden onset of visual loss or visual field deficit, weakness, aphasia, altered sensation, or dysarthria) lasting >24 hours indicates ischaemic stroke. Stereotypical and temporary loss of sensory, motor, or visual function that lasts for <24 hours indicates a TIA.
Patients may present with a variety of visual symptoms, such as transient monocular blindness (amaurosis fugax or temporary loss of vision in the ipsilateral eye), homonymous hemianopia (decrease in visual field from emboli to the optic radiation), intermittent retinal blindness with loss of vision on exposure to bright light, neovascularisation of iris (resulting from ophthalmic artery ischaemia), and, rarely, complete blindness (resulting from ischaemic optic neuropathy).
Screening of the asymptomatic patient
Duplex ultrasonography can be used for identifying patients with asymptomatic carotid stenosis.[14][21][Figure caption and citation for the preceding image starts]: Echolucent internal carotid artery atheroma (yellow arrow) causing 70% stenosis (North American Symptomatic Carotid Endarterectomy Trial criteria). CCA = common carotid artery, ECA = external carotid artery, ICA = internal carotid artery, STA = superior thyroid arteryUsed with permission from BMJ 2013;346:f2420 [Citation ends].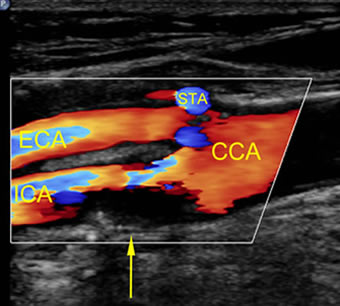
The low prevalence of asymptomatic carotid stenosis in the general population means that indiscriminate screening of all adults does not reduce the risk of stroke, and it is therefore not recommended.[14][22] Patients with at least one high-risk factor may be considered for imaging; however, this is controversial.
The presence of a bruit is associated with carotid artery stenosis of any severity in 47% of patients; however, a clinically high-grade stenosis is found in only <2% of individuals with a bruit.[20][23] Therefore, indiscriminate imaging of all patients with a bruit has not generally been recommended by guidelines, although it may be considered if there are other associated risk factors for stenosis.[14]
Investigations
Duplex ultrasonography, CTA, or MRA should be ordered when carotid artery stenosis is suspected in either an asymptomatic or symptomatic patient in whom intervention might be considered (or treatment modified). The most frequent reason for suspecting the diagnosis in an asymptomatic patient is the presence of atherosclerotic high-risk factors.[14] One study found that duplex ultrasonography will identify a ≥70% degree of stenosis with a sensitivity of 99%, specificity of 86%, and an overall accuracy of 95%.[24] The other modalities have similar accuracy.[25] One Cochrane review evaluating duplex ultrasound for diagnosis of symptomatic carotid stenosis found that it was accurate at discriminating between the presence or absence of significant carotid artery stenosis (<50% or 50% to 99%).[26]
Once it has been established that a stenosis is present in the cervical carotid artery, the next focus is to determine the degree of stenosis. The majority of carotid stenoses are either mild (<50% diameter reduction) or moderate (50% to 69% diameter reduction). Lesion severity has an important role in determination of the type of potential therapy for the patient and prognosis. Quantification is usually performed using the North American Symptomatic Carotid Endarterectomy Trial (NASCET) criteria, whereby the diameter of the arterial lumen at the tightest region of stenosis is compared with the region of the distal internal carotid artery that is free of disease and has non-tapering walls.[27] These criteria have become accepted worldwide and other criteria (e.g., the European Carotid Surgery Trial [ECST] criteria) are rarely used.
The formula used to calculate the degree of stenosis is:
Percentage stenosis = [1 - (minimum diameter/distal diameter)] × 100
Ultrasonography also identifies the anatomy, status of the contralateral carotid, collateral flow, and possible differential diagnoses.[28] CTA and MRA have the advantage of also identifying other lesions within the carotid and vertebral circulation.
When duplex ultrasonography is non-diagnostic, or more information is required on the vessels proximal or distal to the cervical carotid artery, CTA or MRA are appropriate alternatives.[2][14] These tests should be ordered when the results of duplex ultrasonography are equivocal, or fall in the moderate (50% to 69% diameter reduction) stenosis range, which is at the threshold where carotid artery revascularisation may be necessary. They should also be ordered when there is a need to evaluate the arterial anatomy proximal and distal to the cervical carotid artery, or to view the aortic arch before carotid stenting. CTA is performed more commonly compared with MRA, but MRA is preferred in some institutions with specialised capability. CTA is the best modality to determine the degree of stenosis. This is important when determining whether the patient is a candidate for carotid artery stenting or carotid endarterectomy. MRA has a tendency to overestimate stenosis severity.
In symptomatic patients, appropriate assessment of ischaemic brain injury is best accomplished with cranial magnetic resonance imaging (MRI) or computed tomography if MRI is unavailable or contraindicated.
Use of this content is subject to our disclaimer