Approach
Malignant pleural mesothelioma is a rare malignancy and can be overlooked as a possible cause of dyspnoea or pleural effusion. History of asbestos exposure associated with a pleural effusion is strongly suggestive; however, the absence of asbestos exposure on history does not exclude this diagnosis. Patients may be asymptomatic and present with an incidental finding of pleural abnormalities on diagnostic imaging studies.
Clinical presentation
A careful social history, enquiring about possible asbestos exposure (at least occupational), including source and dates of exposure, is crucial. Occupational history regarding the type of work performed (shipyard; construction; maintenance; vehicle brake mechanic; asbestos cement; insulation; or production of tiles, shingles, gaskets, brakes, or textiles) may provide some clues. Men are predominantly affected (male to female ratio 3:1) and as the latency period between exposure to asbestos and development of malignant pleural mesothelioma is 20 to 40 years, patients are typically older adults in their sixth to ninth decade of life.[3]
Symptoms are usually related to the presence of intrathoracic disease and include shortness of breath; dry, non-productive cough; and chest pain. Non-specific symptoms, such as fatigue, fever, sweats, and weight loss, are also common. A history of abdominal distension and/or pain is more typical of primary peritoneal mesothelioma, but may also denote intra-abdominal extension from advanced pleural disease.
Physical findings suggestive of a pleural effusion are typical. These include decreased breath sounds and dullness to percussion on the affected side. Decreased breath sounds can also indicate trapped lung or bronchial obstruction, both of which may be caused by malignant pleural mesothelioma.
Imaging studies
When mesothelioma is suspected, imaging studies should be obtained.
Chest x-ray
Possible findings include unilateral pleural effusion, pleural thickening, reduced lung volumes, or parenchymal changes related to asbestos exposure (e.g., lower zone linear interstitial fibrosis, pleural calcification). However, chest x-ray (CXR) visualises the pleura poorly and will miss subtle abnormalities. [Figure caption and citation for the preceding image starts]: Chest x-ray demonstrating total left-sided collapse and replacement of hemithorax with mesothelioma; there is reduced expansion on this sideFrom BMJ Case Reports 2011;doi:10.1136/bcr.09.2010.3319 [Citation ends].
European guidelines recommend CXR for patients with relevant symptoms and signs (e.g., dyspnoea, chest pain, and weight loss).[35][36][37]
Computed tomography
If clinical suspicion is high, a computed tomography (CT) scan of the chest and upper abdomen with intravenous contrast should also be obtained.[35][38] Findings suggesting a malignant process include circumferential or nodular pleural thickening or involvement of the mediastinal pleura.[39] However, differentiating benign from malignant pleural abnormalities with CT alone is not reliable.[Figure caption and citation for the preceding image starts]: Computed tomography scan of the lung showing a right-sided pleural mesothelioma and left-sided calcified pleural plaqueFrom the collection of Dr Chris R. Kelsey; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Computed tomography scan of the mediastinum showing a right-sided pleural mesothelioma and left-sided calcified pleural plaqueFrom the collection of Dr Chris R. Kelsey; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Computed tomography scan of the mediastinum showing a right-sided pleural mesothelioma and left-sided calcified pleural plaqueFrom the collection of Dr Chris R. Kelsey; used with permission [Citation ends].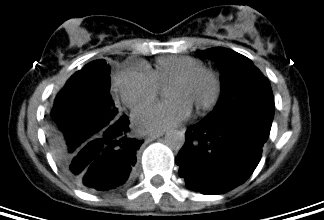
Confirming the diagnosis and prognostication
The diagnosis of mesothelioma cannot be made from imaging studies alone.
Thoracentesis
When imaging studies confirm pleural effusion, with or without other pleural abnormalities, thoracentesis should be performed to determine whether the fluid is a transudate or exudate, and to obtain pleural fluid for cytological examination.[38] The sensitivity of cytology for mesothelioma is relatively low and often requires further pathological assessment of biopsied tissues.[40]
Biopsy
The best study to evaluate the pleural lining of the lung and to obtain optimal biopsies is video-assisted thoracoscopic surgery (VATS).[38] Biopsies of suspicious sites can confirm the diagnosis.
Histological assessment aims to confirm the pathological diagnosis for prognostication and treatment planning by establishing that the lesion meets three criteria:[2]
It is diffuse (more aggressive) and not solitary (usually has a different pathogenesis and a less aggressive course)
It is mesothelial in origin (e.g., exclude other carcinomas with symptom overlap)
It is malignant and not reactive (e.g., based on the presence of invasion into adjacent tissue and full-thickness serosal involvement).
Immunohistochemistry
Recommended for all primary diagnoses.[35][38] Studies should use selected markers expected to be positive in mesothelioma (e.g., calretinin, keratins 5/6, and nuclear WT1) as well as markers expected to be negative in mesothelioma (e.g., CEA, EPCAM, claudin 4, and TTF-1). Other markers can also be used to help exclude differential diagnoses.[38]
Biomarkers, including soluble mesothelin-related peptides (SMRP), cannot be used alone to confirm malignant pleural mesothelioma.[35][36]
Additional studies
Once a diagnosis of mesothelioma is made, additional tests may be necessary to guide management. These include positron emission tomography scans to evaluate for regional or distant disease.[38] In patients who are considered for surgical resection, pulmonary function tests, echocardiogram, and mediastinoscopy are performed to assess cardiopulmonary function and to exclude metastases in the paratracheal and subcarinal lymph nodes within the mediastinum.
Routine blood work, including full blood count and basic metabolic panel, is necessary to establish baseline function before treatment.[Figure caption and citation for the preceding image starts]: Positron emission tomography scan showing hypermetabolic right-sided pleural mesotheliomaFrom the collection of Dr Chris R. Kelsey; used with permission [Citation ends].
Use of this content is subject to our disclaimer