The presentation of cryptosporidiosis is non-specific watery diarrhoea with no pathognomonic features; laboratory testing is necessary to make a diagnosis, usually by detection of Cryptosporidium oocysts, antigens, or DNA in stools. Other samples (intestinal fluid, tissue samples, biopsy specimens, and sputum) may also be tested if considered appropriate: for example, in an immunocompromised patient with complicated disease.
Populations at risk
Physicians should consider cryptosporidiosis as a cause for prolonged diarrhoea in the following populations:
Severely immunocompromised or immunosuppressed individuals and those living with advanced HIV/AIDS
Malnourished infants and young children
Young children, especially those in day care
People who have recently been in contact with farm animals, and visitors to farms or petting zoos
Those who have drunk contaminated water
Travellers returning from non-industrialised countries
Swimmers or bathers
Those in contact with other people with diarrhoea
Those who toilet or change nappies of young children.
As with other causes of infectious diarrhoea, it is important to note occupation as a food-handler or carer, as this may have implications for exclusion from work.
Clinical assessment
Cryptosporidiosis should be considered in any individual who presents with diarrhoea, particularly if duration is >7 days, or the patient is immunocompromised. Clinical history should be taken as epidemiological risk factors will guide testing and hygiene advice (including medical history, household, daycare, travel, recreational water exposure, animal contact, and drinking water). The spectrum of illness ranges from mild to severe. Patients may present with symptoms characteristic of acute disease, or of severe, chronic, or intractable diarrhoeal disease. It is rare for the diarrhoea to be bloody but co-infections with other pathogens may occur. Asymptomatic carriage also occurs.[74]Shane AL, Mody RK, Crump JA, et al. 2017 Infectious Diseases Society of America clinical practice guidelines for the diagnosis and management of infectious diarrhea. Clin Infect Dis. 2017 Nov 29;65(12):1963-73.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5848254
http://www.ncbi.nlm.nih.gov/pubmed/29194529?tool=bestpractice.com
Acute disease
Typical symptoms are watery diarrhoea, nearly always accompanied by abdominal cramps and often loss of appetite, low-grade fever, nausea, and/or vomiting. Symptoms relapse in 30% to 40% of cases.[38]Hunter PR, Hughes S, Woodhouse S, et al. Sporadic cryptosporidiosis case-control study with genotyping. Emerg Infect Dis. 2004 Jul;10(7):1241-9.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3323324
http://www.ncbi.nlm.nih.gov/pubmed/15324544?tool=bestpractice.com
[73]MacKenzie WR, Schell WL, Blair KA, et al. Massive outbreak of waterborne Cryptosporidium infection in Milwaukee, Wisconsin: recurrence of illness and risk of secondary transmission. Clin Infect Dis. 1995 Jul;21(1):57-62.
http://www.ncbi.nlm.nih.gov/pubmed/7578760?tool=bestpractice.com
Symptoms can be persistent, lasting for up to 4 weeks. Significant weight loss can also occur.
Severe, chronic, or intractable diarrhoeal disease
Severe, chronic, or intractable diarrhoeal disease, associated with increased morbidity and mortality, may occur in people with acquired or congenital T-cell immune deficiency. Diarrhoea is watery, of large volume (sometimes >2 litres per day), and is often associated with profound weight loss and prostration. Right upper quadrant abdominal pain is a sign of cholangitis, which is a feature of pancreatobiliary disease occasionally found in severely immunocompromised people. Jaundice may signify sclerosing cholangitis, which can lead eventually to liver cirrhosis, but occurs only in severely immunocompromised people. Sinusitis has very rarely been described in severely immunocompromised people. Tracheobronchial involvement, signified by cough and dyspnoea, occurs rarely in immunocompromised patients.
Patients with HIV infection with CD4+ counts >180/mm^3 are more likely to have transient or self-limiting disease.[75]Flanigan T, Whalen C, Turner J, et al. Cryptosporidium infection and CD4 counts. Ann Intern Med. 1992 May 15;116(10):840-2.
http://www.ncbi.nlm.nih.gov/pubmed/1348918?tool=bestpractice.com
[76]Blanshard C, Jackson AM, Shanson DC, et al. Cryptosporidiosis in HIV-seropositive patients. Q J Med. 1992 Nov-Dec;85(307-308):813-23.
http://www.ncbi.nlm.nih.gov/pubmed/1362461?tool=bestpractice.com
Fulminant disease (marked by the passing of >2 litres stool per day) has only occurred in patients with CD4+ counts <50/mm^3.[76]Blanshard C, Jackson AM, Shanson DC, et al. Cryptosporidiosis in HIV-seropositive patients. Q J Med. 1992 Nov-Dec;85(307-308):813-23.
http://www.ncbi.nlm.nih.gov/pubmed/1362461?tool=bestpractice.com
Lower CD4+ counts were predictive of chronic diarrhoea.[77]Navin TR, Weber R, Vugia DJ, et al. Declining CD4+ T-lymphocyte counts are associated with increased risk of enteric parasitosis and chronic diarrhea: results of a 3-year longitudinal study. J Acquir Immune Defic Syndr Hum Retrovirol. 1999 Feb 1;20(2):154-9.
http://www.ncbi.nlm.nih.gov/pubmed/10048902?tool=bestpractice.com
Four distinct clinical syndromes of cryptosporidiosis have been identified in patients with AIDS with CD4+ counts <200/mm^3: transient diarrhoea, relapsing illness, chronic diarrhoea, and cholera-like illness.[11]Manabe YC, Clark DP, Moore RD, et al. Cryptosporidiosis in patients with AIDS: correlates of disease and survival. Clin Infect Dis. 1998 Sep;27(3):536-42.
http://cid.oxfordjournals.org/content/27/3/536.long
http://www.ncbi.nlm.nih.gov/pubmed/9770154?tool=bestpractice.com
In this patient group, chronic diarrhoea and cholera-like illness with severe weight loss predominated. Although cryptosporidiosis significantly influenced survival rates, this was not linked to individual cryptosporidiosis clinical syndromes.[11]Manabe YC, Clark DP, Moore RD, et al. Cryptosporidiosis in patients with AIDS: correlates of disease and survival. Clin Infect Dis. 1998 Sep;27(3):536-42.
http://cid.oxfordjournals.org/content/27/3/536.long
http://www.ncbi.nlm.nih.gov/pubmed/9770154?tool=bestpractice.com
Asymptomatic carriage
Asymptomatic carriage also occurs, at least among young children, including those in industrialised countries.[12]Pettoello-Mantovani M, Di Martino L, Dettori G, et al. Asymptomatic carriage of intestinal Cryptosporidium immunocompetent and immunodeficient children: a prospective study. Pediatr Infect Dis J. 1995 Dec;14(12):1042-7.
http://www.ncbi.nlm.nih.gov/pubmed/8745015?tool=bestpractice.com
[13]Isaacs D, Hunt GH, Phillpis AD, et al. Cryptosporidiosis in immunocompentent children. J Clin Pathol. 1985 Jan;38(1):76-81.
http://www.ncbi.nlm.nih.gov/pubmed/4038504?tool=bestpractice.com
[14]Baxby D, Hart CA. The incidence of cryptosporidiosis: a two-year prospective survey in a children's hospital. J Hyg (Lond). 1986 Feb;96(1):107-11.
http://www.ncbi.nlm.nih.gov/pubmed/3950390?tool=bestpractice.com
[15]Addiss DG, Stewart JM, Finton RJ, et al. Giardia lamblia and Cryptosporidium infections in child day-care centers in Fulton County, Georgia. Pediatr Infect Dis J. 1991 Dec;10(12):907-11.
http://www.ncbi.nlm.nih.gov/pubmed/1766706?tool=bestpractice.com
[16]García-Rodríguez JA, Martín-Sánchez AM, Canut Blasco A, et al. The prevalence of Cryptosporidium species in children in day care centres and primary schools in Salamanca (Spain): an epidemiological study. Eur J Epidemiol. 1990 Dec;6(4):432-5.
http://www.ncbi.nlm.nih.gov/pubmed/2091947?tool=bestpractice.com
[17]Davies AP, Campbell B, Evans MR, et al. Asymptomatic carriage of protozoan parasites in children in day care centers in the United Kingdom. Pediatr Infect Dis J. 2009 Sep;28(9):838-40.
http://www.ncbi.nlm.nih.gov/pubmed/19684527?tool=bestpractice.com
[18]Lacroix C, Berthier M, Agius G, et al. Cryptosporidium oocysts in immunocompetent children: epidemiologic investigations in the day-care centers of Poitiers, France. Eur J Epidemiol. 1987 Dec;3(4):381-5.
http://www.ncbi.nlm.nih.gov/pubmed/2826221?tool=bestpractice.com
In low-middle income countries, large scale studies have demonstrated that Cryptosporidium infection causes lasting health impacts and high mortality in malnourished infants and young children. Ongoing malnutrition, stunted growth, wasting and cognitive deficit are among the impacts across sub-Saharan Africa, South America and South East Asia.[3]Gilbert IH, Vinayak S, Striepen B, et al. Safe and effective treatments are needed for cryptosporidiosis, a truly neglected tropical disease. BMJ Glob Health. 2023 Aug;8(8):e012540.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10407372
[19]Sallon S, Deckelbaum RJ, Schmid II, et al. Cryptosporidium, malnutrition, and chronic diarrhea in children. Am J Dis Child. 1988 Mar;142(3):312-5.
http://www.ncbi.nlm.nih.gov/pubmed/3344720?tool=bestpractice.com
[20]Sarabia-Arce S, Salazar-Lindo E, Gilman RH, et al. Case-control study of Cryptosporidium parvum infection in Peruvian children hospitalized for diarrhea: possible association with malnutrition and nosocomial infection. Pediatr Infect Dis J. 1990 Sep;9(9):627-31.
http://www.ncbi.nlm.nih.gov/pubmed/2235186?tool=bestpractice.com
[21]Lima AA, Fang G, Schorling JB, et al. Persistent diarrhea in Northeast Brazil: etiologies and interactions with malnutrition. Acta Paediatr Suppl. 1992 Sep;381:39-44.
http://www.ncbi.nlm.nih.gov/pubmed/1421939?tool=bestpractice.com
[22]Mølbak K, Andersen M, Aaby P, et al. Cryptosporidium infection in infancy as a cause of malnutrition: a community study from Guinea-Bissau, west Africa. Am J Clin Nutr. 1997 Jan;65(1):149-52.
http://www.ncbi.nlm.nih.gov/pubmed/8988927?tool=bestpractice.com
[23]Checkley W, Epstein LD, Gilman RH, et al. Effects of Cryptosporidium parvum in Peruvian children: growth faltering and subsequent catch-up growth. Am J Epidemiol. 1998 Sep 1;148(5):497-506.
http://aje.oxfordjournals.org/cgi/reprint/148/5/497
http://www.ncbi.nlm.nih.gov/pubmed/9737562?tool=bestpractice.com
Asymptomatic carriage occurs in both immunocompetent and immunocompromised patients.
Laboratory assessment
The initial assessment for patients with any suspected infectious diarrhoea is traditionally stool microscopy and culture.[74]Shane AL, Mody RK, Crump JA, et al. 2017 Infectious Diseases Society of America clinical practice guidelines for the diagnosis and management of infectious diarrhea. Clin Infect Dis. 2017 Nov 29;65(12):1963-73.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5848254
http://www.ncbi.nlm.nih.gov/pubmed/29194529?tool=bestpractice.com
Increasingly, detection of pathogen nucleic acid: for example, by polymerase chain reaction (PCR)-based methods, is used for diagnosing cryptosporidiosis.[74]Shane AL, Mody RK, Crump JA, et al. 2017 Infectious Diseases Society of America clinical practice guidelines for the diagnosis and management of infectious diarrhea. Clin Infect Dis. 2017 Nov 29;65(12):1963-73.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5848254
http://www.ncbi.nlm.nih.gov/pubmed/29194529?tool=bestpractice.com
These are often provided as multiplex panels with other gastrointestinal pathogens; Cryptosporidium must be included. A positive Cryptosporidium PCR result can be reported without confirmation using another test.[78]Public Health England. UK standards for microbiology investigations S 7: gastroenteritis. Oct 2020 [internet publication].
https://www.gov.uk/government/publications/smi-s-7-gastroenteritis-and-diarrhoea
If microscopy is used, healthcare providers must include relevant information such as travel history or immunocompromise, or they must specifically request testing for Cryptosporidium. This is because regular stool microscopy for ova, cysts, and parasites will not detect Cryptosporidium oocysts, and tests such as staining for Cryptosporidium may not be routinely undertaken.[69]Centers for Disease Control and Prevention. CDC Yellow Book 2024: health information for international travel. Section 5: travel-associated infections and diseases - cryptosporidiosis. May 2023 [internet publication].
https://wwwnc.cdc.gov/travel/yellowbook/2024/infections-diseases/cryptosporidiosis
[79]Garcia LS, Arrowood M, Kokoskin E, et al. Practical guidance for clinical microbiology laboratories: laboratory diagnosis of parasites from the gastrointestinal tract. Clin Microbiol Rev. 2017 Nov 15;31(1):e00025-17.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5740970
http://www.ncbi.nlm.nih.gov/pubmed/29142079?tool=bestpractice.com
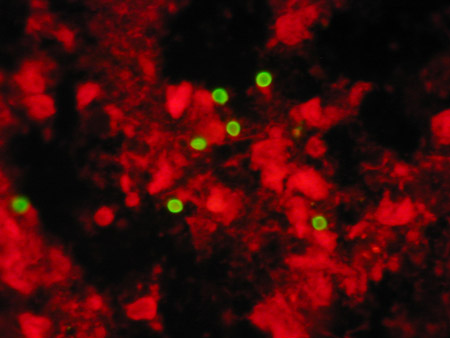
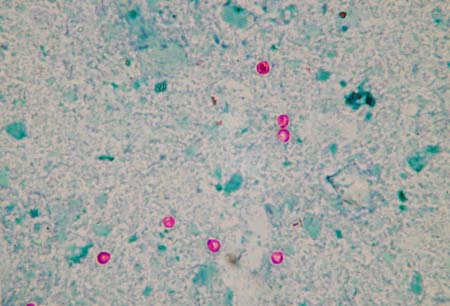
The diagnosis cannot be excluded by one negative stained microscopy test result, and several samples should be tested (3 are recommended).[80]Garcia LS. Diagnostic medical parasitology. 5th ed. Washington DC: ASM Press; 2007. Oocyst concentration by formalin ethyl acetate sedimentation is recommended for formalin-preserved stools before stained microscopy for Cryptosporidium.[80]Garcia LS. Diagnostic medical parasitology. 5th ed. Washington DC: ASM Press; 2007. Staining techniques used in stool microscopy for Cryptosporidium oocysts are acid-fast staining, fluorescent staining (e.g., auramine phenol), and direct fluorescent antibody staining.
Alternatively, enzyme immunoassays or immunochromatographic assays may be used to detect oocyst antigens. Cryptosporidium antigen detection methods provide an alternative to labour-intensive, highly skilled stained microscopy. Enzyme immunoassays are reportedly superior to acid-fast microscopy and can be comparable to direct fluorescent antibody microscopy in terms of sensitivity and specificity. Combined kits for the detection of Cryptosporidium and Giardia, or Cryptosporidium, Giardia, and Entamoeba histolytica are available. Rapid immunochromatographic assays are comparable to acid-fast microscopy but not direct fluorescent antibody staining.[81]Roellig DM, Yoder JS, Madison-Antenucci S, et al. Community laboratory testing for cryptosporidium: multicenter study retesting public health surveillance stool samples positive for cryptosporidium by rapid cartridge assay with direct fluorescent antibody testing. PLoS One. 2017 Jan 13;12(1):e0169915.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5234809
http://www.ncbi.nlm.nih.gov/pubmed/28085927?tool=bestpractice.com
The test kit performance should be monitored, as false positives have been reported.[80]Garcia LS. Diagnostic medical parasitology. 5th ed. Washington DC: ASM Press; 2007.[81]Roellig DM, Yoder JS, Madison-Antenucci S, et al. Community laboratory testing for cryptosporidium: multicenter study retesting public health surveillance stool samples positive for cryptosporidium by rapid cartridge assay with direct fluorescent antibody testing. PLoS One. 2017 Jan 13;12(1):e0169915.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5234809
http://www.ncbi.nlm.nih.gov/pubmed/28085927?tool=bestpractice.com
[82]Doing KM, Hamm JL, Jellison JA, et al. False-positive results obtained with the Alexon ProSpecT Cryptosporidium enzyme immunoassay. J Clin Microbiol. 1999 May;37(5):1582-3.
http://jcm.asm.org/cgi/content/full/37/5/1582?view=long&pmid=10203528
http://www.ncbi.nlm.nih.gov/pubmed/10203528?tool=bestpractice.com
CDC: laboratory identification of parasitic diseases of public health concern - cryptosporidiosis
Opens in new window Positive reactions should be confirmed by a different test.
[Figure caption and citation for the preceding image starts]: Acid-fast-stained Cryptosporidium oocystsFrom the Cryptosporidium Reference Unit collection; used with permission [Citation ends].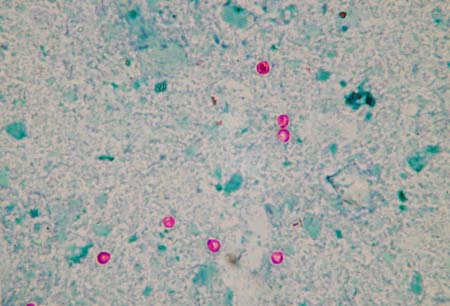 [Figure caption and citation for the preceding image starts]: Auramine-phenol-stained Cryptosporidium oocystsFrom the Cryptosporidium Reference Unit collection; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Auramine-phenol-stained Cryptosporidium oocystsFrom the Cryptosporidium Reference Unit collection; used with permission [Citation ends].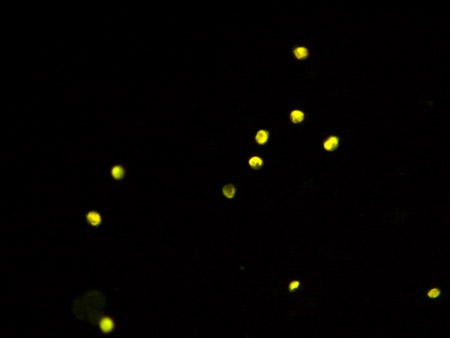 [Figure caption and citation for the preceding image starts]: Direct-immunofluorescent-stained Cryptosporidium oocystsFrom the Cryptosporidium Reference Unit collection; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Direct-immunofluorescent-stained Cryptosporidium oocystsFrom the Cryptosporidium Reference Unit collection; used with permission [Citation ends].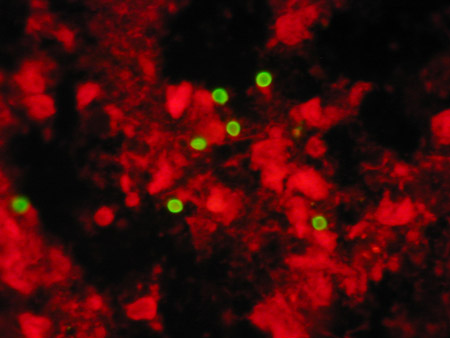
Specialist testing
Detection of DNA by PCR-based methods may be requested for the detection of other lifecycle stages in specimen types other than stool (intestinal fluid, broncho-alveolar washings, antral washings, tissue samples, biopsy specimens) from immunocompromised patients.
None of the methods used in routine primary diagnostic laboratories will identify the Cryptosporidium species present. These PCR-based genotyping tests are available in reference laboratories.
Imaging
Where biliary tract involvement is suspected in an immunocompromised patient, ultrasound or CT scan of the biliary tract is indicated. Confirmation of biliary cryptosporidiosis is possible using endoscopic retrograde cholangiopancreatography to obtain histological biopsies and bile for laboratory testing.
 [Figure caption and citation for the preceding image starts]: Auramine-phenol-stained Cryptosporidium oocystsFrom the Cryptosporidium Reference Unit collection; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Auramine-phenol-stained Cryptosporidium oocystsFrom the Cryptosporidium Reference Unit collection; used with permission [Citation ends].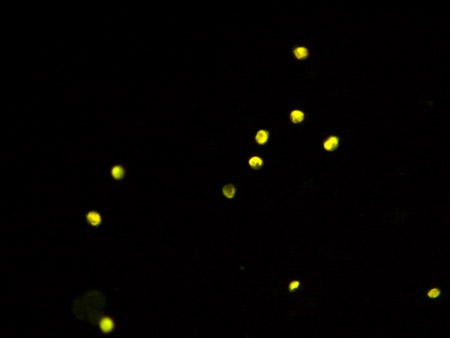 [Figure caption and citation for the preceding image starts]: Direct-immunofluorescent-stained Cryptosporidium oocystsFrom the Cryptosporidium Reference Unit collection; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Direct-immunofluorescent-stained Cryptosporidium oocystsFrom the Cryptosporidium Reference Unit collection; used with permission [Citation ends].