Approach
Trichinellosis is a bi-phasic disease. During the systemic (parenteral) phase, the presence of fever, myalgia, and peri-orbital oedema, in association with a recent history of consuming raw or under-cooked meat, should raise suspicion of trichinellosis. The likelihood of the presence of trichinellosis increases if >1 person is affected in a household or community following consumption of the same meat source.
It is very unlikely for trichinellosis to be recognised and diagnosed during the gastrointestinal (enteric) phase of the disease, as the symptoms of this early stage are non-specific.[34]
The International Commission on Trichinellosis recommends a step-wise approach for the identification of cases of trichinellosis, including:[38]
Searching for typical signs such as diarrhoea, fever, facial oedema, myalgia, eosinophilia (>1000/mm³), and elevation of muscular enzymes and/or total IgE
Identifying if the case is isolated or part of a wider outbreak
Determining the severity of the disease (abortive, mild, moderate, or severe) based on symptomatology
Detecting complications (cardiac, neurological, ocular, respiratory, or digestive)
Hospitalising severe and complicated cases
Alerting public health authorities (e.g., in the US, trichinellosis is a notifiable disease).[39]
Clinical presentation
The incubation period for trichinellosis following the ingestion of raw or under-cooked meat is directly proportional to the acquired parasitic load and ranges from 1-2 days (enteral phase) to 2-8 weeks (parenteral phase) or more, depending on the infectious dose.[9]
The clinical picture can range from asymptomatic infection to fatal disease.[40] However, a full recovery within 6 weeks to 6 months is the most common course. Trichinella spiralis accounts for the most severe cases.[41] The clinical manifestations of trichinellosis develop and change as the weeks from infection progress.[34][Figure caption and citation for the preceding image starts]: Graphic representation of clinical manifestations according to the week of infectionFrom: Summary of Basic Science and Clinical Information section of The Trichinella Page (http://www.trichinella.org); used with permission from Dr Dickson Despommier [Citation ends].
Initial gastrointestinal (enteric) phase
Occurs within a few days of ingesting the parasite.
Manifests with gastrointestinal symptoms, such as abdominal pain, nausea, vomiting, and diarrhoea.
Subsequent systemic (parenteral) phase
Most common manifestations are fever, myalgia, and bi-lateral symmetric peri-orbital or facial oedema.
Fever is an early sign and is present in up to 90% of cases.[42] Fever >40°C (104°F) may occur in the initial 24 hours, but lower temperatures may persist for weeks.[43]
Myalgias are prominent and affect predominantly active muscles, such as oculomotor muscles, tongue, and respiratory muscles. Affected muscles are painful to touch, and there is associated muscle weakness.[43] Myalgia can be so severe that it prevents patients from moving and impairs the ability to chew, swallow, breathe, or talk depending on the muscles involved. The severity of myalgia usually correlates with the degree of eosinophilia.[44]
Facial oedema, particularly affecting the eyelids, can be so severe that the face becomes unrecognisable.[45]
Conjunctivitis and sub-conjunctival haemorrhages, subungual and retinal splinter haemorrhages, severe muscle weakness, apathy, a paralysis-like state, severe headache, and insomnia are common.[6][46]
Other ocular features include eyelid oedema, chemosis, disturbed vision, ocular pain, and paralysis of the ocular muscles.[32] Mydriasis, a marker of severe neurological disease and death, can also be present.[47]
Neurological features include hyporeflexia, tinnitus, vertigo, deafness, aphasia, and seizures.[6][7]
Cutaneous manifestations include pruritus, sweating, and the sensation of crawling insects beneath the skin. A non-specific maculopapular rash may occur (most probably due to parasite-induced vasculitis).[48]
Major complications such as myocarditis and encephalitis may occur in the systemic phase.[49] Myocarditis may present with chest pain, palpitations, dyspnoea, and lower extremity oedema secondary to congestive cardiac failure.
[Figure caption and citation for the preceding image starts]: Trichinellosis manifested by splinter haemorrhages under the finger nailsCDC/Dr Thomas F. Sellers/Emory University [Citation ends].

Chronic trichinellosis
The existence of chronic trichinellosis, following acute disease, remains disputed among experts.[50] Nevertheless, some patients may experience chronic pain, asthenia, excessive diaphoresis, chronic sensation of insects crawling beneath their skin, and rarely conjunctivitis and psychosis, for months to years following the acute infection.
These patients will most probably have a past medical history of confirmed trichinellosis.
Trichinellosis in special populations
The disease has been reported anecdotally in the immunosuppressed; severity does not appear to differ between those cases described and cases in immunocompetent patients.
In pregnant women, trichinellosis can cause miscarriage and premature delivery. The infection may be congenitally acquired, although the majority of babies born to infected women are uninfected.[51]
The infection is milder in children. This is due to a lower parasitic load secondary to the ingestion of smaller portions of affected meat, and to the lack of a strong allergic response.[52]
Initial blood tests
On presentation, all patients should receive a full blood panel including a full blood count (FBC) and muscle enzymes. Leukocytosis, eosinophilia, and elevation of muscle enzymes are present in trichinellosis.
Evaluation of blood chemistry and immunoglobulin E (IgE) is also advisable.
Full blood count
Leukocytosis: ranges from 12,000 to 18,000 cells/mm³.
Eosinophilia: ranges from 1000 to 3000 cells/mm³, but it can be as high as 8000 cells/mm³.[2] Eosinophils make up 10% to 50% of the leukocytosis. The degree of eosinophilia correlates with the number of adult worms causing the infection, and consequently with the number of newborn larvae entering the blood.[2] A low eosinophil count is a rare finding and, along with a sudden drop in the eosinophil count, constitutes a poor prognostic sign that may be associated with death.[46][53]
Muscle enzymes
Creatine kinase, aldolase, lactate dehydrogenase, and transaminases are elevated due to parasitic invasion of skeletal muscle and muscular destruction.[2]
There is a correlation between the degree of muscle enzyme elevation and the level of eosinophilia.[54]
Electrolytes
Hypokalaemia is a frequent finding.[54]
Albumin
Hypo-albuminaemia is a frequent finding and results in an increase of extracellular water content and subsequent oedema.[2]
IgE antibodies
Highly elevated.
It has been speculated that the increase in IgE represents a protective reaction on the part of the human host.[55]
Confirmatory tests
Antibody serology
The International Commission on Trichinellosis recommends the ELISA method using excretory/secretory antigens of the muscle larvae, for screening purposes.[57]
Antibodies to Trichinella species develop within 3-5 weeks of infection.[58] Peak levels may be seen in the second or third month post-infection, followed by a decline.[34] Usually positive in the systemic (parenteral) phase of the disease and by the time clinical symptoms develop, and may remain positive for years.[54]
May occasionally be negative during the systemic phase, but if there is a strong clinical suspicion of trichinellosis, serology should be repeated as the phenomenon of seroconversion is of great diagnostic value.
Positive results obtained by ELISA should be confirmed with Western blot.[57]
Muscle biopsy
Less frequently used technique in clinical practice.[34]
Sensitivity is greatest 4 weeks after infection, when the majority of patients are experiencing an improvement in symptoms. Therefore, it may not be ethically justifiable to undertake such an invasive procedure at this time.
In humans, the most commonly affected muscles are the extra-ocular muscles; the biceps; and the muscles of the jaw, neck, lower back, and diaphragm. However, biopsy samples are traditionally obtained from the deltoid muscle.
The biopsy sample can be examined by pressing it between two slides, digesting it using 1% HCl-1% pepsin (thus releasing larvae from the muscle), or by regular histopathological inspection for the detection of larvae.[2]
If performed too early in the systemic phase, the result may be negative.
Useful for typing the Trichinella species and determining the larval muscular burden.[Figure caption and citation for the preceding image starts]: Larva of Trichinella spiralis in a muscle nurse cellFrom: Summary of Basic Science and Clinical Information section of The Trichinella Page (http://www.trichinella.org); used with permission from Dr Dickson Despommier [Citation ends].
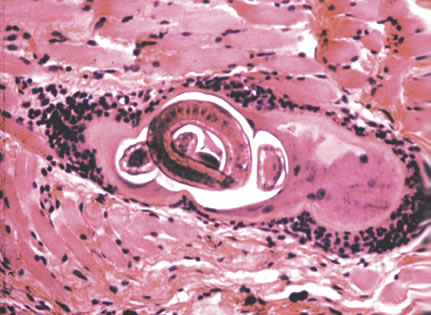 [Figure caption and citation for the preceding image starts]: Trichinella spiralis cysts seen embedded in a muscle tissue specimen, in a case of trichinellosisCDC [Citation ends].
[Figure caption and citation for the preceding image starts]: Trichinella spiralis cysts seen embedded in a muscle tissue specimen, in a case of trichinellosisCDC [Citation ends].
Further investigations
The following tests are not routinely performed, but may be considered in particular situations.
Electromyography
May be more helpful in confirming an alternative diagnosis (such as polymyositis) than in the diagnosis of trichinellosis.
Increased contractibility of striated muscle can be detected using electromyography. However, the findings are non-specific and seldom helpful in confirming the diagnosis of trichinellosis.
Decreased potential amplitude and interference of electrical conduction has been reported.[59]
Electromyographic changes may persist for years after the initial infection.[59]
MRI or CT brain and cerebrospinal fluid analysis
May be considered in suspected cases of neurotrichinellosis. Due to their minute size and lack of calcification in the early stages of the disease, Trichinella larvae in the muscle cannot be detected by conventional radiology.
In neurotrichinellosis, small hypo-dense areas, most probably representing infarctions secondary to parasite-induced vasculitis, may be detected in the brain parenchyma on CT or MRI.[6][60]
In cases of central nervous system compromise, analysis of the cerebrospinal fluid may reveal mild elevations in lymphocytes, eosinophils, and/or protein.[61]
Electroencephalogram
May be considered in suspected cases of trichinellosis complicated by encephalitis, particularly to rule out other aetiologies.
May show diffuse electrical slowing in trichinellosis cases complicated by encephalitis.
ECG
Should be undertaken in suspected cases of trichinella myocarditis.
Trichinella myocarditis is characterised by several ECG changes, including non-specific alteration of ventricular re-polarisation represented by ST-T wave abnormalities and arrhythmias (bundle-branch block or sinus tachycardia). Less commonly, other bradyarrhythmias and tachyarrhythmias, and low-voltage QRS complexes in the limb leads, are seen.[62]
Urinalysis, serum creatinine, and creatinine clearance
May be abnormal and help to identify renal failure in severe cases.[63]
Serum transaminases
May be performed if liver compromise is suspected.[64]
Investigations in delayed presentation
In patients with chronic trichinellosis, abnormal electromyography findings and positive serum antibodies may persist for years after the initial infection.[50][65]
Use of this content is subject to our disclaimer