Investigations
1st investigations to order
neck CT with contrast
Test
Preferably done before biopsy as staging for suspected malignancy. CT scans performed without contrast are not as useful because of the inability to differentiate between normal and abnormal enhancement.[34] [Figure caption and citation for the preceding image starts]: CT scan showing bulky tumour invading ala of thyroid cartilageFrom the collection of Dr Amy Chen, Emory University; used with permission [Citation ends].
CT scans are better than physical examination for detecting cervical lymph node metastasis but cannot accurately assess lymph nodes <1 cm. The sensitivity of CT for detecting cervical lymph node metastasis is much less than that for PET scan (78% vs. 96%).[1][36]
Small laryngeal lesions may also be missed on CT scan, but these will be seen on flexible fibre-optic laryngoscopy.
Result
laryngeal mass may show cartilage invasion; presence or absence of cervical lymphadenopathy
chest CT with or without contrast
Test
Typically accompanies neck CT, as the most common site of metastasis of head and neck cancer is to the lungs.
Result
normal or metastatic nodules, lymphadenopathy
MRI with and without contrast
Test
May be used as a complementary tool if CT does not provide adequate information or in place of CT for patients who cannot undergo a CT.[1]
Result
evaluation of bony erosion or cartilage invasion as well as soft tissue invasion
fine needle aspiration of neck mass
Test
Indicated if a neck mass is palpable. If a mass is not palpable but is seen on CT scan, a CT-guided or ultrasound-guided biopsy may be useful.
Cytological analysis of the aspirate may often confirm the diagnosis of squamous cell carcinoma, as well as other malignancies.
A negative result does not rule out malignancy.
Result
may show squamous cell carcinoma
flexible fibre-optic laryngoscopy
Test
Performed in any person with hoarseness, dysphagia, odynophagia (painful swallowing), or throat pain lasting >3 weeks. Also necessary for sufficient follow-up of patients with laryngeal cancer.
Simultaneously allows excellent visualisation of the larynx and assessment of airway patency. In some cases biopsies can be performed using a fibre-optic laryngoscope. [Figure caption and citation for the preceding image starts]: Irregular mass of left arytenoid and aryepiglottic folds, and the right arytenoid mucosaFrom the collection of Dr Amy Chen, Emory University; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Small whitish mass along anterior third of left true vocal foldFrom the collection of Dr Amy Chen, Emory University; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Small whitish mass along anterior third of left true vocal foldFrom the collection of Dr Amy Chen, Emory University; used with permission [Citation ends].
Limitations include inability to completely assess extent of tumour in some patients and inability to definitively diagnose cancer (e.g., does not yield immediate histopathology results).
If no lesions are seen and the index of suspicion is high, rigid endoscopy is indicated.
Result
lesion involving the vocal folds, epiglottis, arytenoids, or aryepiglottic folds
Investigations to consider
rigid videostroboscopy
Test
Enables superior evaluation of the true vocal fold mucosal wave and vocal fold mechanics, at times helping to determine sub-mucosal extent of disease.
Result
may demonstrate vocal cord fixation
rigid direct laryngoscopy
Test
Strong suspicion of laryngeal cancer and complete tumour staging mandate direct laryngoscopy with biopsy.
General anaesthesia is required and necessitates careful co-ordination with the anaesthesiologist to secure and maintain the airway.
Result
ulcerative, friable, necrotic mass involving the larynx
immunohistochemistry testing
Test
Programmed death ligand-1 (PD-L1) immunohistochemistry testing should be performed in patients with recurrent or metastatic head and neck squamous cell carcinoma, and tumour mutational burden (TMB) testing may be performed when PD-L1 is not available.[37]
Result
PD-L1 combined positive score >1 should be interpreted as positive.TMB ≥10 should be interpreted as high.
laryngeal biopsy
Test
Indicated if laryngeal malignancy is suspected (e.g., at time of rigid endoscopy).
Multiple biopsies should be obtained of the lesion, as pathology is limited by the quality of the specimen collected. If the specimen is obtained from a necrotic portion of the tumour, pathology may not demonstrate features characteristic of squamous cell carcinoma.
Frozen section pathology may be used to confirm that the biopsy specimen is representative. Additional specimens may be obtained if frozen section is negative or if index of suspicion is high.
Result
superficial ulceration, necrosis, cellular atypia, mitotic figures, and invasion of basement membrane; in advanced cases, perineural and angiolymphatic invasion
whole-body PET/CT scan
Test
Whole-body PET/CT scan is more sensitive than CT in detecting nodal and distant metastases, and is indicated in patients with higher grade tumours (T3-T4 primary, or ≥N1 nodal stage).[1]
Increased uptake on PET imaging is not specific to malignancy. Infection or inflammation may also increase uptake. [Figure caption and citation for the preceding image starts]: Large, bulky transglottic mass and increased uptake on PET (bright yellow/orange)From the collection of Dr Amy Chen, Emory University; used with permission [Citation ends].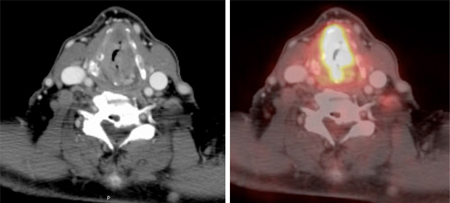
Findings must be put into context with the patient's overall clinical condition and may warrant additional studies to evaluate these areas.
Result
increased uptake in areas of malignancy and metastasis
fluorescence endoscopy
Test
Auto-fluorescence endoscopy is available in some centres, typically using a xenon arc lamp with a narrow excitation spectrum ranging from 375 to 440 nm. Remitted excitation light up to 440 nm is blocked out by an integrated optic filter within the endoscope, enabling switching from white-light endoscopy to fluorescence endoscopy.[35]
Result
red-violet coloration (loss of auto-fluorescence) in dysplastic lesions
Use of this content is subject to our disclaimer