Investigations
1st investigations to order
MRI spinal cord
Test
Required in all patients to exclude compressive myelopathy.[1]
Detection of intrinsic cord lesion assists in confirmation of myelitis.
Partial/asymmetric cord lesion extending over 1 or 2 vertebral segments supports diagnosis of acute partial TM.[8]
Complete TM with longitudinally extensive lesion (≥3 contiguous vertebral segments) supports the diagnosis of longitudinally extensive TM, which suggests causes other than multiple sclerosis. These include neuromyelitis optica spectrum disorder, infection, connective tissue disease-associated TM, or idiopathic TM.[1][23][8]
If initial MRI is negative, reconsider diagnosis of myelopathy and consider repeating in 7 to 10 days.[1][23][8][Figure caption and citation for the preceding image starts]: Sagittal T2-weighted MRI of cervical spinal cord showing myelitis lesionFrom the personal collection of Dean M. Wingerchuk, MD, MSc, FRCP(C); used with permission [Citation ends].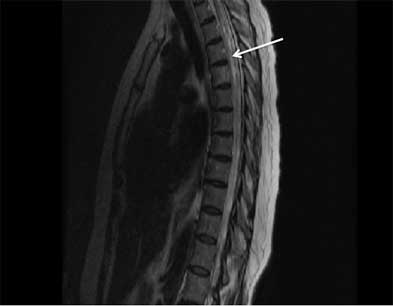 [Figure caption and citation for the preceding image starts]: Sagittal T2-weighted MRI showing multiple sclerosis-related myelitis lesionFrom the personal collection of Dean M. Wingerchuk, MD, MSc, FRCP(C); used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Sagittal T2-weighted MRI showing multiple sclerosis-related myelitis lesionFrom the personal collection of Dean M. Wingerchuk, MD, MSc, FRCP(C); used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Sagittal T2-weighted MRI showing longitudinally extensive transverse myelitis lesionFrom the personal collection of Dean M. Wingerchuk, MD, MSc, FRCP(C); used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Sagittal T2-weighted MRI showing longitudinally extensive transverse myelitis lesionFrom the personal collection of Dean M. Wingerchuk, MD, MSc, FRCP(C); used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Sagittal T1-weighted MRI showing enhancement of neuromyelitis optica-related lesionFrom the personal collection of Dean M. Wingerchuk, MD, MSc, FRCP(C); used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Sagittal T1-weighted MRI showing enhancement of neuromyelitis optica-related lesionFrom the personal collection of Dean M. Wingerchuk, MD, MSc, FRCP(C); used with permission [Citation ends].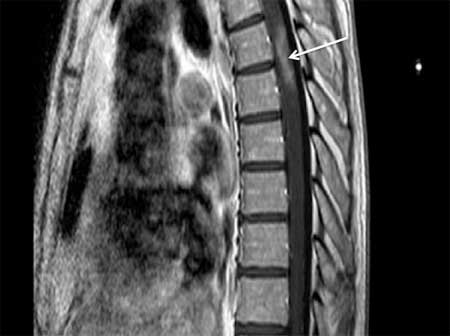
Result
increased T2-weighted MRI signal within the spinal cord, usually with gadolinium enhancement of the lesion; excludes compressive lesion
MRI brain
Test
Peri-ventricular, brain stem, and juxta-cortical lesions suggest multiple sclerosis (MS) in setting of acute partial TM.[58]
Peri-aqueductal lesions or lesions involving the thalamic and hypothalamic region suggest neuromyelitis optica spectrum disorder (NMOSD).
Normal results suggest NMOSD or idiopathic TM in setting of complete TM.[1][23][8]
Result
lesions detected by increased T2-weighted MRI signal in setting of MS (common) and NMOSD (uncommon); otherwise normal
serum aquaporin-4 auto-antibodies and myelin oligodendrocyte glycoprotein auto-antibodies
Test
Longitudinally extensive myelitis, defined by a lesion extending over ≥3 contiguous vertebral segments, has a greater risk of recurrence if serum aquaporin-4 (AQP4) auto-antibodies are present.[5]
Testing for the presence of anti-AQP4 auto-antibodies is therefore critical for determining whether preventive therapy is necessary.
Persistently positive myelin oligodendrocyte glycoprotein-IgG is also associated with clinical relapses.[59][60]
Result
may be present
cerebrospinal fluid cell count, cell differential, protein level, IgG index, oligoclonal bands
Test
Increased cell count (>5 WBC/mm³) supports inflammatory myelitis.
Normal cerebrospinal fluid does not exclude TM but consider repeating lumbar puncture in 7 to 10 days if TM is strongly suspected.
Most causes are associated with 10 to 2000 WBC/mm³.
Presence of neutrophils, >50 WBC/mm³, and negative oligoclonal bands suggests neuromyelitis optica spectrum disorder.[4]
Less than 50 WBC/mm³ with lymphocytic differential and presence of increased IgG index or oligoclonal bands in setting of acute partial TM suggests multiple sclerosis.[1][23][8]
Result
pleocytosis, increased protein level, abnormal immunoglobulin production (IgG index), and presence of oligoclonal bands
cerebrospinal fluid Gram stain, cultures (bacterial, tubercular, fungal), and India ink smear
Test
Negative in non-infectious TM; helpful when there are constitutional symptoms, fever, and/or cerebrospinal fluid pleocytosis.[61]
Result
positive in infectious myelitis caused by bacteria, TB, or fungi
cerebrospinal fluid, polymerase chain reaction for herpes simplex virus (HSV)-1, HSV-2, varicella zoster virus (VZV), Borrelia burgdorferi (Lyme disease), cytomegalovirus (CMV), Epstein-Barr virus (EBV), and West Nile virus
Test
Useful for detection of HSV-1, HSV-2, VZV, Borrelia burgdorferi (Lyme disease), CMV, EBV, West Nile virus.[61]
Result
positive in specific infection
cerebrospinal fluid Venereal Disease Research Laboratory test
Test
Positive cerebrospinal fluid Venereal Disease Research Laboratory test is virtually 100% specific for syphilis, but a negative result does not exclude the diagnosis.
Result
positive in syphilis
serum anti-nuclear antibody, double-stranded DNA
Test
Multiple positive auto-antibodies are also often found in association with neuromyelitis optica spectrum disorder.[62]
Result
positive in systemic lupus erythematosus
extractable nuclear antigen (including SSA and SSB)
Test
Multiple positive auto-antibodies are also often found in association with neuromyelitis optica spectrum disorder.[62]
These antibodies are insensitive, and salivary gland biopsy may be needed if there is a high suspicion for Sjogren's syndrome.
Result
positive in Sjogren's syndrome
serum and cerebrospinal fluid paraneoplastic auto-antibodies
Test
May indicate the presence of an underlying malignancy. The most common are amphyphisin and collapsin response-mediator protein-5.[42]
Result
positive in myelopathy associated with paraneoplastic antibodies
other neural auto-antibodies
Test
Disease associated with auto-antibodies to glial fibrillary acidic protein (GFAP) is an inflammatory central nervous system disorder, in both paraneoplastic and idiopathic autoimmune contexts, that may present with TM.[63]
Result
positive in myelopathy associated with GFAP-IgG antibody
Investigations to consider
serum and cerebrospinal fluid angiotensin-converting enzyme
Test
Insensitive tests.
Result
elevated in sarcoidosis
chest x-ray
Test
May detect pulmonary infection or mediastinal lymphadenopathy or other lung parenchymal abnormality consistent with sarcoidosis.
Result
positive with some infections, malignancy, and sarcoidosis
CT body (chest, abdomen, and pelvis)
Test
May detect pulmonary infection or mediastinal lymphadenopathy or other lung parenchymal abnormality consistent with sarcoidosis.[64]
Result
lymphadenopathy in sarcoidosis, malignancy
whole-body PET scan
Test
May be done in conjunction with CT body. Part of the diagnostic work-up for occult malignancy related to paraneoplastic myelopathy.
Result
malignancy and lymphadenopathy in sarcoidosis
cerebrospinal fluid cytology and flow cytometry
Test
Indicated if high clinical suspicion of malignancy.
May require up to 3 serial cerebrospinal fluid examinations to exclude false-negative results.
Result
positive in malignancy
serology for herpes simplex virus (HSV)-1, HSV-2, varicella zoster virus, cytomegalovirus, Epstein-Barr virus, and West Nile virus
Test
Acute and convalescent serologies may confirm recent infection in para-infectious or infectious TM.[61]
Result
positive in viral infection
urinalysis
Test
May be useful to detect possible systemic lupus erythematosus (SLE).
Result
haematuria with SLE
HIV antibodies
Test
High-risk individuals.[23]
Result
positive in HIV
visual-evoked potential
optical coherence tomography
Test
Thinning of the retinal nerve fibre layer, supports recent or prior optic neuropathy/neuritis.[45]
Result
abnormal in multiple sclerosis and neuromyelitis optica spectrum disorder
therapeutic trial with corticosteroid
Test
If the MRI and cerebrospinal fluid studies support TM but all other studies are negative, empiric treatment with corticosteroids can be considered both to confirm that the disorder is steroid-responsive and to improve symptoms.[23]
Clinical improvement during or shortly after corticosteroids confirms a steroid-responsive inflammatory TM in most cases, although keep in mind the possibility of central nervous system lymphoma, which also responds to corticosteroids.[23]
At this point, the evaluation can move from diagnosis to evaluation of risk for recurrent TM, neuromyelitis optica spectrum disorder, or multiple sclerosis.
Result
clinical and radiological improvement in inflammatory myelitis
spinal cord biopsy
Test
Biopsy should be considered in patients with severe TM with failure to improve; or an enlarging lesion despite empiric corticosteroids.[23] Biopsy may allow differentiation of inflammatory TM from granulomatous disease (sarcoidosis), lymphoma, or other neoplasm.
Result
confirms inflammatory myelopathy or specific diagnosis
Use of this content is subject to our disclaimer