Approach
Diagnosis of TM is made following history, physical examination, magnetic resonance imaging (MRI) spinal cord and brain, and cerebrospinal fluid (CSF) analysis. Other possible causes of symptoms, such as spinal cord compression and ischaemia, require exclusion. Additional tests are based on the MRI and CSF test results and aim to identify whether the spinal cord syndrome is due to an inflammatory disorder, infection, or paraneoplastic aetiology, and to pinpoint its cause.[37] They include testing for antibodies against aquaporin-4 (AQP4) and myelin oligodendrocyte glycoprotein (MOG), special CSF stains, cultures and tests for infections, chest x-ray, computed tomography (CT) of the thorax, viral serologies, auto-antibodies to test for systemic lupus erythematosus (SLE) or Sjogren's syndrome, visual evoked potential and/or optical coherence tomography, and biopsies.
Clinical presentation
The typical presentation leading to consideration of TM includes the following:[1][23][24][37][38]
Progressive paraparesis or quadriparesis
Sensory loss and/or paraesthesias
Autonomic (bowel and bladder) dysfunction
An evolution of signs over several days.
The clinical syndrome usually has bilateral features, although they may be asymmetric.[1][6][37] Radicular or segmental pain may occur at the level of the spinal lesion. Back pain, L'hermitte's sign (paraesthesias in the limbs, elicited by neck flexion), and paroxysmal tonic spasms (repetitive, stereotypic motor spasms of ≥1 limbs and/or the trunk, each lasting 30-45 seconds) may occur.[37]
Sensory loss to vibration, proprioception, and pain modalities occurs to varying degrees below the lesion, and examination usually reveals a sensory level at or a few vertebral segments caudal to the lesion.[2] Urinary and bowel incontinence or retention may occur. In severe and rapidly progressive cases, paralysis may be associated with areflexia ('spinal shock'), but this generally evolves into a typical spastic paraparesis/quadriparesis pattern with hyper-reflexia and Babinski's signs. Severe cases of ascending myelitis involving the cervical spinal cord may cause neurogenic respiratory failure.[4] Longitudinally extensive TM can produce hiccups due to involvement of the medulla, and persistent nausea and vomiting due to involvement of the area postrema.
Interpretation of clinical spinal cord syndrome
Characteristic spinal cord syndromes (complete cord syndrome, Brown-Sequard's syndrome, conus-medullaris syndrome) are associated with distinct pathologies and may assist in the differential diagnosis.
A complete cord syndrome, identified by loss of all motor and sensory modalities below the level of the lesion, is associated with acute, severe, 'necrotising' myelitis.
The Brown-Sequard's syndrome (partial or complete) suggests multiple sclerosis (MS). It is identified by detecting dysfunction of the corticospinal tracts (spastic weakness, hyper-reflexia, and an extensor plantar response) and dorsal columns (loss of vibration and proprioception) ipsilateral to the lesion, and spinothalamic tract dysfunction (loss of pain and temperature sensation) contralateral to the lesion.
Some viral or post-viral myelitis syndromes are associated with a conus-medullaris syndrome, which presents with relatively symmetric lower extremity weakness and hyper-reflexia, preserved knee jerks and affected ankle jerks, relatively symmetric peri-anal or saddle anaesthesia, and early bladder and sexual dysfunction. Conus-medullaris involvement is also frequent with TM associated with MOG-IgG.[39]
Exclusion of compressive myelopathy
The first step in evaluation of a patient with an acute or subacute spinal cord syndrome is to exclude a compressive lesion such as a neoplasm.[1][23] This is best accomplished with MRI of the entire spinal cord because it is rapid, highly sensitive, and specific for detection of compressive lesions, and can identify multiple sites of compression and avoid pitfalls such as false localising neurological signs.[37]
Interpretation of spinal cord MRI
Once extrinsic compressive lesions are excluded, the spinal cord MRI should be assessed for the presence of one or more intrinsic lesions. The presence of such lesions confirms the clinical suspicion of myelopathy and provides clues to its aetiology.[1][23] If the MRI does not reveal a hyper-intense signal abnormality within the cord, this should prompt re-evaluation of the diagnosis of myelopathy.[23] If one or more lesions are detected, then lesion number, size, and distribution can assist in the differential diagnosis.[Figure caption and citation for the preceding image starts]: Sagittal T2-weighted MRI of cervical spinal cord showing myelitis lesionFrom the personal collection of Dean M. Wingerchuk, MD, MSc, FRCP(C); used with permission [Citation ends].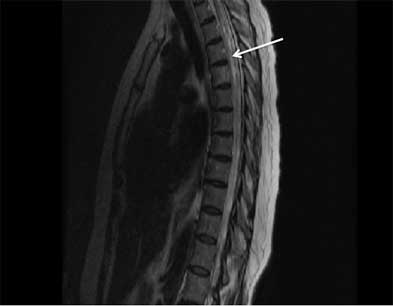 [Figure caption and citation for the preceding image starts]: Axial T2-weighted MRI of cervical spinal cord showing myelitis lesionFrom the personal collection of Dean M. Wingerchuk, MD, MSc, FRCP(C); used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Axial T2-weighted MRI of cervical spinal cord showing myelitis lesionFrom the personal collection of Dean M. Wingerchuk, MD, MSc, FRCP(C); used with permission [Citation ends].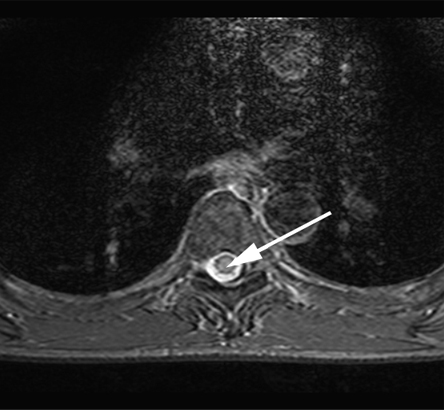 [Figure caption and citation for the preceding image starts]: Sagittal T2-weighted MRI showing multiple sclerosis-related myelitis lesionFrom the personal collection of Dean M. Wingerchuk, MD, MSc, FRCP(C); used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Sagittal T2-weighted MRI showing multiple sclerosis-related myelitis lesionFrom the personal collection of Dean M. Wingerchuk, MD, MSc, FRCP(C); used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Sagittal T2-weighted MRI showing longitudinally extensive transverse myelitis lesionFrom the personal collection of Dean M. Wingerchuk, MD, MSc, FRCP(C); used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Sagittal T2-weighted MRI showing longitudinally extensive transverse myelitis lesionFrom the personal collection of Dean M. Wingerchuk, MD, MSc, FRCP(C); used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Sagittal T1-weighted MRI showing enhancement of neuromyelitis optica-related lesionFrom the personal collection of Dean M. Wingerchuk, MD, MSc, FRCP(C); used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Sagittal T1-weighted MRI showing enhancement of neuromyelitis optica-related lesionFrom the personal collection of Dean M. Wingerchuk, MD, MSc, FRCP(C); used with permission [Citation ends].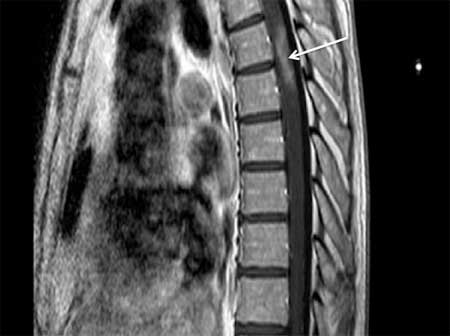
Longitudinally extensive lesions suggest NMOSD, whereas short-segment lesions are typical for MS. However, in up to 14% of patients with NMOSD, the initial myelitis may be associated with a short-segment lesion.[40][41]
The location of the lesions on axial MRI may also be helpful in determining the aetiology of TM. In patients with AQP4-IgG-associated NMOSD, lesions are located centrally, or centrally and peripherally, and involve more than 50% of the spinal cord area. MS lesions typically involve <50% of the transversal spinal cord area, usually located in the dorsal and lateral portions.[8] MOG-IgG- associated myelitis may have a distinctive 'H sign', with T2 hyperintensity restricted to the grey matter. Conus involvement is also common.[39] Paraneoplastic myelopathies often present tract-specific changes (tractopathy), with T2-hyperintensity of the dorsal columns, or the corticospinal tracts.[42] Spinal cord sarcoidosis may present dorsal subpial enhancement and central canal enhancement, which in axial images, has the appearance of a trident.[43]
Definition of the presence or absence of central nervous system (CNS) inflammation
CSF examination should be obtained. CSF abnormalities that suggest inflammatory myelitis (e.g., demyelinating, paraneoplastic, or other inflammatory myelitis) include mild pleocytosis, elevated protein, elevated IgG index, and the presence of oligoclonal bands. The presence of abnormal cells may indicate a neoplasm.[1][23][8]
Determination of the extent of CNS involvement
Brain MRI with intravenous gadolinium administration can determine whether the disorder is restricted to the spinal cord or involves other CNS regions. It can reveal white matter lesions consistent with demyelinating diseases such as MS or NMOSD, or other lesional patterns that may strongly suggest a specific diagnosis (e.g., sarcoidosis). Visual-evoked potentials and/or optical coherence tomography can detect sub-clinical involvement of the optic nerves.[44][1][45] Complete or partial TM with normal brain MRI and CSF studies suggests an isolated myelitis syndrome.[1][46]
Additional testing based on MRI and CSF results
Following positive MRI and CSF analysis, it is important to determine the cause of myelitis. Based on the clinical history and examination, patients should be tested for infection and systemic inflammatory and autoimmune diseases, and also for malignancy if paraneoplastic myelopathy is suspected.[37]
Auto-antibodies associated with longitudinally extensive TM: AQP4-IgG and MOG- IgG antibodies in serum.
Infection: tests should include CSF cultures, special CSF stains, serum cultures, and chest x-ray. HIV testing is recommended in high-risk patients.[23]
Systemic autoimmune or inflammatory disease: tests should include serum auto-antibodies and markers for systemic inflammatory diseases, urinalysis (for SLE), and chest x-ray. Serum and CSF angiotensin-converting enzyme may be elevated in patients with sarcoidosis, but these are insensitive tests.
Malignancy: serum and CSF paraneoplastic antibody panel should be obtained if paraneoplastic myelopathy in suspected.[42] Specific antibodies may guide malignancy work-up, but tests generally include chest x-ray, chest or body CT and/or positron emission tomography. CSF cytology and CSF flow cytometry may be helpful to diagnose intramedullary tumours. Patients with leptomeningeal carcinomatosis may require up to 3 serial CSF examinations to exclude false-negative results.
Consideration of a therapeutic trial with corticosteroids
A specific diagnosis may be achieved following completion of previous steps, in which case treatment may be instituted. In a retrospective study, the final diagnosis was idiopathic TM in 15.6% of patients presenting with acute TM.[24] In some instances, the diagnosis remains unclear but there are data to support a probable inflammatory myelopathy. Empirical treatment with corticosteroids may be reasonable at this point.[23] It is important to exclude pyogenic myelitis, epidural abscess and spinal cord abscess/compression/meningomyelitis due to TB in the differential diagnosis before attempting corticosteroid therapy. Clinical improvement suggests that the underlying pathophysiology is indeed inflammatory/demyelinating; however, CNS lymphoma should be considered.
Consideration of a spinal cord biopsy
In cases of progressive myelitis/myelopathy associated with an enlarging or treatment-unresponsive lesion, diagnostic biopsy should be considered for detection of infection, granulomatous disease, or neoplasm.[23]
Evaluation of risk of recurrence
If the diagnosis is an inflammatory TM, brain MRI and serological testing (AQP4-IgG and MOG-IgG antibodies) are helpful to determine recurrence risk. For patients with a short (1 or 2 segment) cord lesion, the presence of typical white matter lesions on brain MRI suggests a high risk for recurrent CNS inflammation and confirmed MS.[3][47][48][49]
Longitudinally extensive myelitis, defined by a lesion extending over three or more contiguous vertebral segments, has a greater risk of recurrence if serum AQP4 auto-antibodies are present.[5][8] Testing for the presence of anti-AQP4 auto-antibodies is therefore critical for determining whether preventive therapy is necessary.
In children, risk factors for relapse and disability after idiopathic TM include female sex, more severe disability at onset, gadolinium enhancement of the spinal cord lesion on MRI, absence of CSF pleocytosis, and absence of cervical or cervico-thoracic lesion on spinal MRI.[50]
Use of this content is subject to our disclaimer