Aetiology
Seronegative arthritis is characterised by joint pain and inflammation in the absence of rheumatoid factor (RF). Although no clear-cut definition exists, the following differential diagnoses should be considered:
Spondyloarthropathies
Crystalline arthropathies
Inflammatory/connective tissue disease
Systemic diseases
Infectious arthritis
Neoplastic/paraneoplastic arthritis.
Spondyloarthropathies, crystalline and viral arthropathies, and rheumatoid arthritis are the most common diagnoses in patients with seronegative arthritis.[1][2]
Spondyloarthropathic
Spondyloarthropathies encompass ankylosing spondylitis, psoriatic arthritis, reactive arthritis, enteropathic arthritis, and undifferentiated spondyloarthropathy.
The hallmark of this group of diseases is enthesitis. This may present with dactylitis or 'sausage digit', or tenderness at entheseal insertions (e.g., Achilles tendon or plantar fascia insertions).
When the axial skeleton is involved, the presentation is with inflammatory back pain.
Peripheral joint involvement may be oligoarticular, involving large joints, or polyarticular.
Psoriatic arthritis may present with distal interphalangeal (DIP) involvement. [Figure caption and citation for the preceding image starts]: Psoriatic arthritisFrom the collection of Dr Tsu-Yi Chuang; used with permission [Citation ends].

Extra-articular manifestations may include uveitis, psoriasis, keratoderma blennorrhagica, and erythema nodosum. [Figure caption and citation for the preceding image starts]: Psoriasis plaque: legsFrom the collection of Dr Tsu-Yi Chuang; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Keratoderma blennorrhagica in a patient with reactive arthritisImage provided by the CDC Public Health Image Library [Citation ends].
[Figure caption and citation for the preceding image starts]: Keratoderma blennorrhagica in a patient with reactive arthritisImage provided by the CDC Public Health Image Library [Citation ends]. [Figure caption and citation for the preceding image starts]: Erythema nodosum on the shin of a patientFrom the collection of Dr Om P. Sharma; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Erythema nodosum on the shin of a patientFrom the collection of Dr Om P. Sharma; used with permission [Citation ends].
Crystalline deposition
Calcium pyrophosphate deposition disease (CPPD)
Arthritis may present in 4 patterns: pseudo-rheumatoid arthritis, osteoarthritis with synovitis, pseudogout, and monoarthropathy. [Figure caption and citation for the preceding image starts]: Wrist radiograph from a patient with chronic calcium pyrophosphate arthritis showing severe degenerative changesFrom the collection of Ann K. Rosenthal, MD; used with permission [Citation ends].

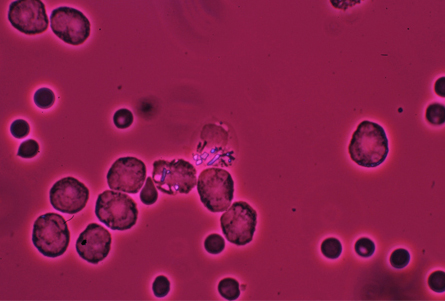
Investigation for CPPD crystals is recommended in all synovial fluid obtained from inflamed joints, especially knees and wrists of older patients.[3][Figure caption and citation for the preceding image starts]: Image of intracellular calcium pyrophosphate crystals under compensated polarising light microscopyFrom the collection of Ann K. Rosenthal, MD; used with permission [Citation ends].
Co-existing septic arthritis should be considered in the differential of monoarthritis.[3]
Gout
Early gout usually presents with acute arthritis and affects men aged under 50 years. If untreated, it evolves into polyarticular tophaceous gout. [Figure caption and citation for the preceding image starts]: Chronic tophaceous gout showing nodules in periarticular structures and arthritisAdapted from BMJ Case Reports 2009 [doi:10.1136/bcr.03.2009.1668] Copyright © 2009 by the BMJ Publishing Group Ltd [Citation ends].

Women present with gout at an older age, and may have their first presentation with polyarticular tophaceous gout. In addition, podagra (inflammation of the great toe) is less common, as are recurrent gout attacks.[4]
When chronic it may be difficult to differentiate from other types of inflammatory arthritis.
Inflammatory/rheumatic
In older people, acute polyarthritis may present with acute onset of pitting oedema of the hands. The differential diagnoses are polymyalgia rheumatica, remitting seronegative symmetrical synovitis with pitting oedema syndrome, crystalline arthropathies, and older-onset rheumatoid arthritis.
Polymyalgia rheumatica
Usually presents with upper limb girdle myalgia and stiffness and responds to low-dose corticosteroids.
Polyarthritis may also occur; it may be difficult to differentiate from older-onset rheumatoid arthritis.[5] One third of patients may be seronegative for RF and antibodies against cyclic citrullinated peptides.
Remitting seronegative symmetrical synovitis with pitting oedema syndrome
Rare disease that usually presents in men aged over 50 years with acute-onset polyarthritis and bilateral hand-pitting oedema. Patients respond to low-dose corticosteroids. Those who do not respond should be assessed for underlying malignancy.[6][7]
Rheumatoid arthritis
Usually causes a symmetrical small joint polyarthritis in the wrists and hands, particularly affecting the metacarpophalangeal (MCP) or proximal interphalangeal (PIP) joints.[8]
Patients with acute disease may also feel generally unwell with fatigue and low mood.
Acute-phase reactants and RF may be normal in 37% or less of patients.[2]
Juvenile idiopathic arthritis (JIA)
The cardinal symptoms are significant fever, arthralgia, myalgia, and rash. The rash may be maculopapular or an evanescent salmon-pink rash.
Acute-phase reactants are elevated. Leukocytosis, hyperferritinaemia, and elevation of transaminases may be seen.[9]
Osteoarthritis
Slow onset and typical pattern of joint involvement and osteophyte formation.
A small proportion of patients may develop erosive osteoarthritis. This is a variant that occurs in middle-aged women and is associated with typical PIP and DIP gull wing erosions on plain x-rays. Imaging shows central and peripheral joint erosion and low-grade inflammation within the joint.[10][11][12]
Sarcoidosis
Acute sarcoidosis may present with bilateral ankle periarthritis. The arthritis usually lasts for 3 to 4 weeks.[13]
Connective tissue disease
Arthritis or arthralgia may occur in connective tissue diseases such as systemic lupus erythematosus (SLE), scleroderma, inflammatory myositis, Sjogren's syndrome, or mixed connective tissue disease.
Small- to medium-vessel vasculitis
May present with arthralgia, constitutional symptoms, purpura, mononeuritis multiplex, or glomerulonephritis. May suggest a more rapid work-up with particular attention to multiple organ function.
Symptoms of mesenteric ischaemia and evidence of cardiac decompensation or hypertension are suggestive of polyarteritis nodosa.[14]
Infectious
Non-gonococcal infectious arthritis
Infectious arthritis should be considered in any acute monoarticular joint involvement, especially in the presence of fever. Risk factors include: >80 years of age, diabetes mellitus, rheumatoid arthritis, joint surgery, hip or knee prosthesis, skin infection, and human immunodeficiency infection.[15][16][17][18] Staphylococcus aureus and streptococci are the most common pathogens.
Gram-negative bacteria or anaerobes should be considered in intravenous drug users or immunocompromised patients.[15]
Disseminated gonococcal infection
Gonococcal arthritis is a clinical manifestation of disseminated gonococcal infection, a rare complication of N gonorrhoeae infection.[19][20]
Disseminated gonococcal infection is more frequent in women and presents with migratory polyarthralgia and tenosynovitis. The knees, wrists, ankles, and elbows are the most commonly affected joints. Tenosynovitis affects the hands, ankles, knees, and feet.
A significant proportion of patients have fever and dermatitis, which may present as a maculopapular or a vesicular rash.
Most patients do not have local genitourinary, rectal, or pharyngeal symptoms. However, gonococcal infection can be demonstrated in 70% to 80% of cases.[21][Figure caption and citation for the preceding image starts]: Gonococcal arthritis of the hand, which caused the hand and wrist to swellCDC/ Susan Lindsley, VD; used with permission [Citation ends].

Bacterial endocarditis
Subacute polyarthritis may complicate subacute bacterial endocarditis due to immune complex formation. The most common presentations are oligoarticular and monoarticular arthritis. Involvement of ankles, knees, shoulders, and sternoclavicular joints may be seen.
Low back pain and diffuse lower extremity myalgias may occur.[22][23]
Other manifestations include constitutional symptoms, splinter haemorrhages, Osler's nodes, Janeway lesions, petechial haemorrhages, splenomegaly, and haematuria.[24][25][Figure caption and citation for the preceding image starts]: Cutaneous infarctsFrom the collection of Sanjay Sharma; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Janeway lesionsFrom the collection of Sanjay Sharma; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Janeway lesionsFrom the collection of Sanjay Sharma; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Osler's nodeFrom the collection of Sanjay Sharma; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Osler's nodeFrom the collection of Sanjay Sharma; used with permission [Citation ends].
Rheumatic fever
Acute rheumatic fever occurs after streptococcal throat infection and may present with migratory polyarthritis affecting large joints, including knees, ankles, wrists, and elbows.
Atypical presentations with oligoarthritis or monoarthritis may occur, as well as dactylitis. It may be associated with carditis, chorea, erythema marginatum, or subcutaneous nodules.[26]
Lyme disease
Early disease may present with fever and migratory arthralgia or may be painless. The diagnosis can be challenging in the absence of erythema migrans.
Arthritis may manifest within one to several months after infection, primarily affecting the large joints, but small joints can also be involved.[27] Acute-phase reactants may not be elevated, and antinuclear antibody and RF are usually negative.[28][29][Figure caption and citation for the preceding image starts]: Erythema migransFrom the collection of Dr Cristian Speil; used with permission [Citation ends].

Viral-induced arthritis
Infections that may cause polyarticular symptoms include HIV infection; hepatitis A, B, and C infections; human T-cell lymphotropic virus; and alpha viruses, such as chikungunya virus.
Arthritis related to hepatitis B virus infection may present as acute polyarthritis related to acute infection.
Hepatitis C virus infection commonly causes polyarthralgia but is often associated with a positive RF. Parvovirus B19 infection presents acutely with polyarticular symmetrical arthralgia without significant swelling. Arthralgia is more common in women and may be associated with erythema infectiosum.[30] The arthralgia usually lasts 3 to 4 weeks but may last several months.
Before highly active antiretroviral therapy (HAART), rheumatic manifestations of HIV infection included HIV-associated arthritis, reactive arthritis, psoriatic arthritis, and painful articular syndrome. However, the spectrum of disease has significantly changed with HAART therapy, and a syndrome resembling rheumatoid arthritis, SLE, or polymyositis may emerge de novo.[31][Figure caption and citation for the preceding image starts]: Typical erythematous 'slapped cheeks' of erythema infectiosumFrom the collection of Gary A. Dyer, MD; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Lacy, reticular, erythematous eruption of erythema infectiosum on an upper extremityFrom the collection of Gary A. Dyer, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Lacy, reticular, erythematous eruption of erythema infectiosum on an upper extremityFrom the collection of Gary A. Dyer, MD; used with permission [Citation ends].
Whipple's disease
Patients may present with arthralgia, fever, and diarrhoea. A rare disease, prevalence is greater in white people compared with African-Americans, but does not differ with respect to sex.[32] The diagnosis may be confirmed by demonstrating the presence of periodical acid-Schiff positive organisms in the lamina propria of the small intestine. Polymerase chain reaction of blood and cerebrospinal fluid may demonstrate the presence of Tropheryma whipplei.[33]
Neoplastic/paraneoplastic
Neoplastic carcinomatosis
Monoarticular and sometimes polyarticular forms of arthritis have been reported to occur with non-Hodgkin's lymphoma and acute and chronic leukemia. The arthritis does not respond to conventional therapy.[34][35]
Paraneoplastic arthritis
Polyarthritis may occur as a paraneoplastic syndrome. It may mimic rheumatoid arthritis. RF is frequently negative. It may be differentiated by its asymmetrical distribution, affliction of predominantly lower extremities, extreme pain, synovitis, constitutional symptoms, and the presence of hepatosplenomegaly and lymphadenopathy.
Paraneoplastic arthritis is most commonly associated with breast, colon, lung, ovarian, gastric, and oesophageal cancers and lymphoproliferative disorders.[36][37]
Use of this content is subject to our disclaimer