Investigations
1st investigations to order
DNA-based assays
Test
Provide the most accurate diagnosis but usually reserved for antenatal diagnosis or those with genotypes that are more difficult to diagnose.
Often used for confirming an abnormality found by haemoglobin studies. May be used in place of haemoglobin studies in some screening programmes. Considered more reliable than haemoglobin isoelectric focusing (Hb IEF).
Result
replacement of both beta haemoglobin subunits with HbS is diagnostic for sickle cell anaemia (HbSS); presence of 1 normal beta haemoglobin subunit and 1 HbS is diagnostic for sickle cell trait
haemoglobin isoelectric focusing (Hb IEF)
Test
Although not a definitive diagnostic test, IEF is commonly used to determine the presence of the sickle cell gene.[26]
Can also be used to determine the percentage of HbS in a blood sample. This is particularly helpful in guiding and monitoring treatment - for example, to determine how effective simple or exchange transfusion has been to decrease the patient's level of sickled haemoglobin.
All newborn screening is performed using Hb IEF or high-performance liquid chromatography (HPLC).
Result
fetal haemoglobin (HbF) will predominate in newborns with sickle cell disease; in older infants the amount of HbS will increase as HbF decreases; by 2 years of age the amount of HbS and HbF stabilises; patients with sickle cell anaemia will have no HbA
cellulose acetate electrophoresis
Test
In older children and adults, cellulose acetate electrophoresis at an alkaline pH is most commonly used to determine haemoglobin subtype. Diagnosis can be confirmed using an alternative method.
Result
sickle cell anaemia 75% to 95% HbS, HbA is notably absent; sickle cell trait 40% HbS, <2% HbF, 60% HbA
high-performance liquid chromatography (HPLC)
Test
When abnormal haemoglobin is identified, DNA-based assays or HPLC are used to confirm the diagnosis and further identify the genotype. These tests also allow the distinction between heterozygotes and homozygotes.
Result
in newborns with sickle cell disease, fetal HbF will predominate; in older infants, the amount of HbS will increase as HbF decreases; by 2 years of age the amount of HbS and HbF stabilises; patients with sickle cell anaemia will have no HbA
haemoglobin solubility testing
Test
May be used for initial screening in older children and adults, but cannot distinguish between sickle cell trait (heterozygotes) and sickle cell disease (homozygotes).
Not recommended for infants under 6 months because the high proportion of fetal haemoglobin in relation to adult sickle cell haemoglobin in a newborn's blood may affect the results.
A normal result excludes sickle cell disease in patients older than 6 months without symptoms or signs of severe anaemia or very high fetal haemoglobin levels.
Result
≥10% to 15% HbS
peripheral blood smear
Test
Helps rule out additional causes of anaemia but requires expert interpretation and cannot be used to determine whether patient is in vaso-occlusive crisis.[Figure caption and citation for the preceding image starts]: Red cells in sickle cell diseaseFrom the personal collection of Sophie Lanzkron, MD; used with permission [Citation ends].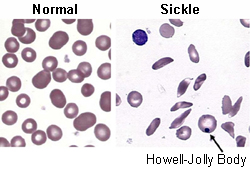
Evaluation of the type and an estimate of the number of white blood cells, red blood cells, and platelets is made to assess if they are normal in morphology and number. Sickle-shaped cells, Howell-Jolly bodies, presence of nucleated red blood cells, and cell fragments can be seen on the blood smear. Oat cells and target cells can be seen in HbSC disease.
Result
presence of nucleated red blood cells, sickle-shaped cells, and Howell-Jolly bodies
FBC and reticulocyte count
Test
Used in testing older children and adults to evaluate number and quality of red blood cells, haemoglobin content, and white blood cell count. Useful in establishing a baseline for on-going evaluation. Widely available, inexpensive, and provides rapid results, but it is not diagnostic.
Patients can present with vaso-occlusive pain and not have any change from baseline in their haemoglobin or reticulocyte count.
White blood cell count can occasionally be overestimated if the count is not corrected for the presence of nucleated red cells, which are often present.
In patients with very low reticulocyte counts <1%, parvovirus infection should be strongly considered.
Result
some degree of anaemia occurs in most patients; reticulocyte count is usually elevated, but may be reduced in aplastic crisis (caused by parvovirus B19 infection in patients with chronic haemolytic disorders) or bone marrow infarction
iron studies
Test
Helps distinguish haemolytic anaemia from iron-deficiency anaemia. Patients who have been transfused in the past will have elevated results.
Result
serum iron, transferrin, ferritin levels, and serum iron-binding capacity are normal or elevated
Investigations to consider
pulse oximetry
Test
Pulse oximetry monitoring is important as early drops in oxygen saturations can suggest the beginning of acute chest syndrome.
Result
shows oxygen desaturations in acute chest syndrome
plain x-rays of long bones
Test
Used to confirm the presence of bone infarction. Most bone infarctions are diagnosed clinically by symptoms (bone pain) and signs (e.g., absence of fever).
Result
infarctions seen by irregular margins or moth-eaten destruction with overlying periosteal new bone formation
bacterial cultures
Test
Bacterial cultures (using blood, sputum, urine, stool, and/or pus) should be obtained in patients with fever and/or those who appear toxic.
Result
bacterial pathogen culture may confirm infection
chest x-ray
Test
Performed if the patient has respiratory symptoms, fever, or chest pain.[Figure caption and citation for the preceding image starts]: Chest x-ray in acute chest syndromeFrom: Davies SC, Oni L. BMJ. 1997 Sep 13;315(7109):656-60 [Citation ends].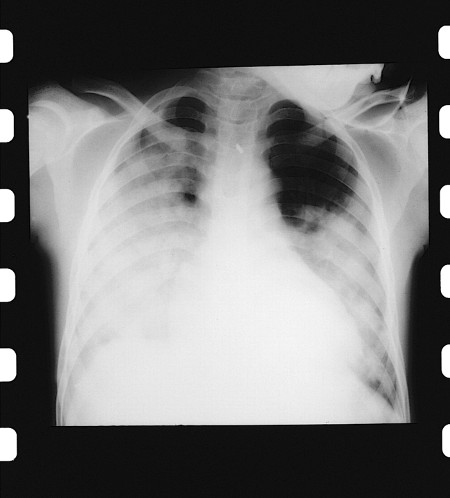
Result
presence of pulmonary infiltrate(s) may be an indication of acute chest syndrome
Use of this content is subject to our disclaimer