History and exam
Key diagnostic factors
common
unimmunized status
While unimmunized status is a factor, paralytic poliomyelitis can also occur in children having received the vaccine, sometimes as a result of the oral attenuated poliovirus vaccine (OPV) itself or because OPV did not provide protective immunity.[1]
residence or travel in endemic area
Those who are not vaccinated or who are immunosuppressed are most at risk.[3]
decreased tone and motor function of affected limb
A sign of paralytic poliomyelitis.
decreased tendon reflexes of affected limb
A sign of paralytic poliomyelitis.
muscle atrophy of affected limb
A sign of paralytic poliomyelitis.[Figure caption and citation for the preceding image starts]: Child displaying deformity of her right leg due to poliomyelitisCDC Public Health Image Library [Citation ends].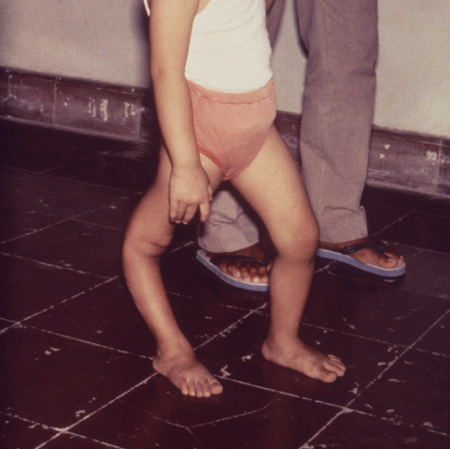
Other diagnostic factors
common
age <36 months
Those who are not vaccinated or who are immunosuppressed are most at risk.[3]
gastrointestinal prodrome
This is common in the minor and major illnesses but is a nonspecific sign, especially in the setting of developing countries, where multiple, far more common, diarrheal illnesses predominate.[1]
fever
Symptom in the mild, nonparalytic illness.
malaise
Symptom in the mild, nonparalytic illness.
uncommon
respiratory muscle atrophy and respiratory distress
A sign of bulbar paralytic poliomyelitis.
Risk factors
strong
lack of vaccination
poor sanitation
Due to the fecal-oral transmission route of the disease, inadequate sanitation facilitates the spread of poliovirus.[24]
area of endemic infection
Poliovirus-endemic areas are usually those with particular factors that inhibit vaccination, such as remote location, war-torn environment, and cultural barriers to vaccination. Thus, residence in one of these areas tends to confer risk of not being immunized, and consequently being at risk for endemic or imported poliomyelitis caused either by wild or vaccine-derived poliovirus.[26][27]
weak
poverty
As one of the social determinants of subsequent health, poverty is associated with lack of healthcare access. However, this is offset to some degree by the WHO poliomyelitis eradication teams that visit every household for vaccinations. In addition, many poverty-stricken areas of the world have successfully eliminated poliomyelitis.[25][26]
immunosuppression
Patients who are immunocompromised due to congenital or acquired immunodeficiency are more susceptible to infection from vaccine-attenuated virus present in the oral form of poliovirus vaccine.[28]
Use of this content is subject to our disclaimer