Tests
1st tests to order
upper gastrointestinal endoscopy
Test
Gastroscopy has low sensitivity for the diagnosis of early achalasia and may be reported as normal. However, it is an essential first-line investigation to exclude malignancy.[25]
In patients with a dilated esophagus, a clear fluid diet for a prolonged period or esophageal lavage may be required before endoscopy to avoid aspiration and to obtain adequate views. The gastroesophageal junction can be tight but gives way with sustained gentle pressure with the gastroscope.
Biopsies from the cardia should be performed to exclude pseudoachalasia.
Result
mucosa obscured by retained saliva with frothy appearance; in advanced cases, esophagus may be dilated and tortuous and contain food debris (sigmoid esophagus)
barium swallow
Test
In early disease the swallow may be reported as normal. In advanced disease the dilated esophagus may be tortuous and sigmoid-shaped with diverticula.
Fluoroscopy is often used during a barium swallow.[26]
Result
loss of peristalsis and delayed esophageal emptying; dilated esophagus that tapers smoothly to a beak-like narrowing at the gastroesophageal junction
high-resolution esophageal manometry
Test
High-resolution manometry is more accurate than conventional manometry for the diagnosis of achalasia.[29][28] It has superseded conventional manometry and is now the gold standard for the diagnosis and subclassification of achalasia into 3 discrete subtypes.[28][36]
A multisensory catheter is used that enables detailed pressure topography plotting of esophageal motility.
In some patients with achalasia it might not be possible to pass the manometry catheter through the lower esophageal sphincter.
Longitudinal muscle spasm and consequent esophageal shortening can result in apparent pseudorelaxation with traditional manometry, but this problem does not arise with high-resolution manometry.[37]
Result
incomplete relaxation of the lower esophageal sphincter with wet swallows and esophageal aperistalsis are the two most important manometric criteria for the diagnosis of achalasia; high-resolution manometry defines three clinical subtypes of achalasia, which are classified using the Chicago criteria; type I: impaired lower esophageal sphincter (LOS) relaxation without peristalsis, characterized by 100% failed contractions and no esophageal pressurizations; type II: impaired LOS relaxation with pan-esophageal pressurization occurring in at least 20% of swallows; type III: impaired LOS relaxation with premature esophageal contractions or distal peristalsis in at least 20% of swallows. The subtype of achalasia predicts the response to treatment
Tests to consider
chest x-ray
Test
Appearance may suggest achalasia, but the test has a low sensitivity and is not diagnostic.
Result
absence of the gastric gas bubble and dilated esophagus with an air-fluid level
radionucleotide esophageal emptying studies
Test
This investigation can be used for monitoring response to therapy.[31]
Result
delayed esophageal transit
timed barium esophagogram
Test
Barium swallow in which multiple sequential films are shot at pre-set time intervals.
Simple technique that directly measures liquid esophageal emptying.
Does not require any special equipment or expertise and is repeatable; therefore, can be used to assess the progress of the disease and the outcome of treatment.[32][33][Figure caption and citation for the preceding image starts]: Classic appearance of dilated esophagus with tapered beak-like narrowing on barium studyFrom the collection of Dr Jin-Yong Kang; used with permission [Citation ends].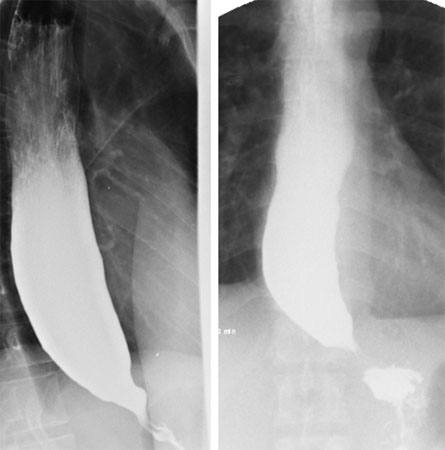
Result
delayed esophageal transit
CT chest
Test
Used to rule out gastroesophageal infiltration by invading extrinsic or intrinsic malignancy.
Asymmetric thickening may suggest pseudoachalasia.
Recommended in an older individual or if there is rapid or profound weight loss.
Result
dilation of the esophagus; often concentric thickening of esophageal wall
impedance planimetry
Test
To evaluate sphincter function by measuring changes in pressure with diameter and volume.[34][35] This can be utilized at the time of endoscopy or surgery at the gastroesophageal junction to measure the gastroesophageal junction distensibility using the functional luminal imaging probe (FLIP) device.
Result
may provide complementary information to high-resolution manometry where the diagnosis of achalasia is not clear and may provide peri-operative or endoscopic response to treatment in real-time.
Use of this content is subject to our disclaimer