Hyperhidrosis
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
primary: axillary hyperhidrosis
topical aluminum chloride
Topical aluminum chloride is the first-line treatment for axillary hyperhidrosis.[2]Solish N, Wang R, Murray CA. Evaluating the patient presenting with hyperhidrosis. Thorac Surg Clin. 2008 May;18(2):133-40. http://www.ncbi.nlm.nih.gov/pubmed/18557587?tool=bestpractice.com [11]Gee S, Yamauchi PS. Nonsurgical management of hyperhidrosis. Thorac Surg Clin. 2008 May;18(2):141-55. http://www.ncbi.nlm.nih.gov/pubmed/18557588?tool=bestpractice.com [19]Solish N, Bertucci V, Dansereau A, et al. A comprehensive approach to the recognition, diagnosis and severity-based treatment of focal hyperhidrosis: recommendations of the Canadian Hyperhidrosis Advisory Committee. Dermatol Surg. 2007 Aug;33(8):908-23. http://www.ncbi.nlm.nih.gov/pubmed/17661933?tool=bestpractice.com
Commonly used preparations include 20% aluminum chloride in ethanol and 6.25% aluminum tetrachloride.
Local stinging and burning may occur due to formation of hydrochloric acid when sweat combines with the aluminum chloride. Topical baking soda or hydrocortisone cream may help if this occurs.[11]Gee S, Yamauchi PS. Nonsurgical management of hyperhidrosis. Thorac Surg Clin. 2008 May;18(2):141-55. http://www.ncbi.nlm.nih.gov/pubmed/18557588?tool=bestpractice.com
Primary options
aluminum chloride topical: apply to the affected area(s) once daily at bedtime until desired effect is achieved, then taper to once weekly
short-term anticholinergic
Treatment recommended for SOME patients in selected patient group
For those patients with symptoms exacerbated in known anxiety-provoking situations, a short-term oral anticholinergic taken as required can be considered together with any of the other therapies, although its side effects (e.g., dry eyes and mouth, urinary retention, cramps, weakness, nausea, and headache) may limit its usefulness.
Glycopyrrolate (as glycopyrronium) is also available as a topical wipe and is approved for patients with primary axillary hyperhidrosis.
Primary options
glycopyrrolate: 1-2 mg orally twice or three times daily when required
OR
oxybutynin: 2.5 mg orally (immediate-release) once daily initially, increase gradually according to response, maximum 10 mg/day given in 2 divided doses; 5-10 mg orally (extended-release) once daily
OR
glycopyrronium topical: (2.4% pad) apply one pad to affected area once daily
onabotulinumtoxinA
If symptoms do not resolve with aluminum chloride, onabotulinumtoxinA (botulinum toxin type A) injections may be considered.
Approved in the US for axillary use and can be effective for months at a time.[11]Gee S, Yamauchi PS. Nonsurgical management of hyperhidrosis. Thorac Surg Clin. 2008 May;18(2):141-55. http://www.ncbi.nlm.nih.gov/pubmed/18557588?tool=bestpractice.com [20]Heckmann M, Ceballos-Baumann AO, Plewig G, et al. Botulinum toxin A for axillary hyperhidrosis (excessive sweating). New Engl J Med. 2001 Feb 15;344(7):488-93. https://www.nejm.org/doi/full/10.1056/NEJM200102153440704 http://www.ncbi.nlm.nih.gov/pubmed/11172190?tool=bestpractice.com
The injection process may be painful. However, local topical anesthetic may help.[11]Gee S, Yamauchi PS. Nonsurgical management of hyperhidrosis. Thorac Surg Clin. 2008 May;18(2):141-55. http://www.ncbi.nlm.nih.gov/pubmed/18557588?tool=bestpractice.com
Primary options
onabotulinumtoxinA: 50 units intradermally given in 0.1 to 0.2 mL aliquots to multiple sites (10-15) 1-2 cm apart in each axilla
short-term anticholinergic
Treatment recommended for SOME patients in selected patient group
For those patients with symptoms exacerbated in known anxiety-provoking situations, a short-term oral anticholinergic taken as required can be considered together with any of the other therapies, although its side effects (e.g., dry eyes and mouth, urinary retention, cramps, weakness, nausea, and headache) may limit its usefulness.
Glycopyrrolate (as glycopyrronium) is also available as a topical wipe.
Primary options
glycopyrrolate: 1-2 mg orally twice or three times daily when required
OR
oxybutynin: 2.5 mg orally (immediate-release) once daily initially, increase gradually according to response, maximum 10 mg/day given in 2 divided doses; 5-10 mg orally (extended-release) once daily
OR
glycopyrronium topical: (2.4% pad) apply one pad to affected area once daily
targeted alkali thermolysis (TAT) technology patch
If the patient does not respond to onabotulinumtoxinA or does not want repeated painful shots with temporary results, a targeted alkali thermolysis (TAT) technology patch is another treatment option. It has been approved by the Food and Drug Administration (FDA) for the treatment of primary axillary hyperhidrosis. In TAT, the sodium in the path interacting with the water of the sweat produces thermal energy causing local inactivation of the sweat glands for a period of several months. A double-blinded multicenter study showed a statistically significant improvement compared to placebo, with a decrease in sweat production by more than half in 60% of those treated.[21]Glaser DA, Green L, Kaminer MS, et al. Outcomes from the SAHARA clinical study on the TAT patch for excessive axillary sweating or primary axillary hyperhidrosis. Paper presented at: American Academy of Dermatology annual meeting. 2023. Louisiana, USA. https://candesant.com/wp-content/uploads/2023/07/SCALE_2023_Poster_Clinical_050423.pdf
short-term anticholinergic
Treatment recommended for SOME patients in selected patient group
For those patients with symptoms exacerbated in known anxiety-provoking situations, a short-term oral anticholinergic taken as required can be considered together with any of the other therapies, although its side effects (e.g., dry eyes and mouth, urinary retention, cramps, weakness, nausea, and headache) may limit its usefulness.Glycopyrrolate (as glycopyrronium) is also available as a topical wipe.
Primary options
glycopyrrolate: 1-2 mg orally twice or three times daily when required
OR
oxybutynin: 2.5 mg orally (immediate-release) once daily initially, increase gradually according to response, maximum 10 mg/day given in 2 divided doses; 5-10 mg orally (extended-release) once daily
OR
glycopyrronium topical: (2.4% pad) apply one pad to affected area once daily
local microwave treatment
Local microwave treatment is another noninvasive treatment option for primary axillary hyperhidrosis.[16]McConaghy JR, Fosselman D. Hyperhidrosis: management options. Am Fam Physician. 2018 Jun 1;97(11):729-34. https://www.aafp.org/afp/2018/0601/p729.html http://www.ncbi.nlm.nih.gov/pubmed/30215934?tool=bestpractice.com [22]Rzany B, Bechara FG, Feise K, et al. Update of the S1 guidelines on the definition and treatment of primary hyperhidrosis. J Dtsch Dermatol Ges. 2018 Jul;16(7):945-52. http://www.ncbi.nlm.nih.gov/pubmed/29989362?tool=bestpractice.com [23]National Insitute for Health and Care Excellence. Transcutaneous microwave ablation for severe primary axillary hyperhidrosis. Dec 2017 [internet publication]. https://www.nice.org.uk/guidance/ipg601 It works by destroying eccrine sweat glands through thermolysis. In one study, 90% of patients who received microwave therapy experienced a 50% reduction in axillary sweat at 12 months follow-up.[24]Hong HC, Lupin M, O'Shaughnessy KF. Clinical evaluation of a microwave device for treating axillary hyperhidrosis. Dermatol Surg. 2012 May;38(5):728-35. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3489040 http://www.ncbi.nlm.nih.gov/pubmed/22452511?tool=bestpractice.com
short-term anticholinergic
Treatment recommended for SOME patients in selected patient group
For those patients with symptoms exacerbated in known anxiety-provoking situations, a short-term oral anticholinergic taken as required can be considered together with any of the other therapies, although its side effects (e.g., dry eyes and mouth, urinary retention, cramps, weakness, nausea, and headache) may limit its usefulness.Glycopyrrolate (as glycopyrronium) is also available as a topical wipe.
Primary options
glycopyrrolate: 1-2 mg orally twice or three times daily when required
OR
oxybutynin: 2.5 mg orally (immediate-release) once daily initially, increase gradually according to response, maximum 10 mg/day given in 2 divided doses; 5-10 mg orally (extended-release) once daily
OR
glycopyrronium topical: (2.4% pad) apply one pad to affected area once daily
local sweat gland excision
If the patient does not respond to onabotulinumtoxinA or does not want repeated painful injections with temporary results, local sweat gland excision by curettage or liposuction should be considered next.
Local axillary gland surgeries (including subcutaneous gland resection with or without resection of the overlying skin, curettage-liposuction, or electrosurgical or laser glandular destruction) have been shown to be effective.[25]Skoog T, Thyresson N. Hyperhidrosis of the axillae. A method of surgical treatment. Acta Chir Scand. 1962 Dec;124:531-8. http://www.ncbi.nlm.nih.gov/pubmed/13989093?tool=bestpractice.com [26]Bechara FG, Sand M, Tomi NS, et al. Repeat liposuction-curettage treatment of axillary hyperhidrosis is safe and effective. Br J Dermatol. 2007 Oct;157(4):739-43. http://www.ncbi.nlm.nih.gov/pubmed/17634083?tool=bestpractice.com [27]Lawrence CM, Lonsdale Eccles AA. Selective sweat gland removal with minimal skin excision in the treatment of axillary hyperhidrosis: a retrospective clinical and histological review of 15 patients. Br J Dermatol. 2006 Jul;155(1):115-8. http://www.ncbi.nlm.nih.gov/pubmed/16792762?tool=bestpractice.com [28]Bechara FG, Altmeyer P, Sand M, et al. Surgical treatment of axillary hyperhidrosis. Br J Dermatol. 2007 Feb;156(2):398-9. http://www.ncbi.nlm.nih.gov/pubmed/17223898?tool=bestpractice.com [29]Kim IH, Seo SL, Oh CH. Minimally invasive surgery for axillary osmidrosis: combined operation with CO2 laser and subcutaneous tissue remover. Dermatol Surg. 1999 Nov;25(11):875-9. http://www.ncbi.nlm.nih.gov/pubmed/10594601?tool=bestpractice.com Local procedures seem to be more effective, with better patient satisfaction than thoracoscopic sympathetic surgeries, and have less compensatory and gustatory sweating.[30]Heidemann E, Licht PB. A comparative study of thoracoscopic sympathicotomy versus local surgical treatment for axillary hyperhidrosis. Ann Thorac Surg. 2013 Jan;95(1):264-8. http://www.ncbi.nlm.nih.gov/pubmed/23200232?tool=bestpractice.com
The procedure may be complicated by poor wound healing or scarring. Unlike surgical sympathectomy, local surgical procedures generally have no systemic manifestations (e.g., compensatory hyperhidrosis).
short-term anticholinergic
Treatment recommended for SOME patients in selected patient group
For those patients with symptoms exacerbated in known anxiety-provoking situations, a short-term oral anticholinergic taken as required can be considered together with any of the other therapies, although its side effects (e.g., dry eyes and mouth, urinary retention, cramps, weakness, nausea, and headache) may limit its usefulness.
Glycopyrrolate (as glycopyrronium) is also available as a topical wipe.
Primary options
glycopyrrolate: 1-2 mg orally twice or three times daily when required
OR
oxybutynin: 2.5 mg orally (immediate-release) once daily initially, increase gradually according to response, maximum 10 mg/day given in 2 divided doses; 5-10 mg orally (extended-release) once daily
OR
glycopyrronium topical: (2.4% pad) apply one pad to affected area once daily
endoscopic thoracoscopic sympathectomy (ETS)
If symptoms persist, ETS may be considered.[31]National Institute for Health and Care Excellence. Endoscopic thoracic sympathectomy for primary hyperhidrosis of the upper limb. May 2014 [internet publication]. https://www.nice.org.uk/guidance/ipg487 The procedure is generally done on both sides at one sitting, under general anesthesia, and is a short-stay procedure in the majority of instances.
The specific hyperhidrosis disorder determines the level of the sympathetic procedure.
For example, surgery at the third (T3), fourth (T4), or fifth (T5) thoracic ganglia is for axillary hyperhidrosis.
Some controversy exists whether compensatory sweating is more problematic at higher sympathectomy levels, but patient selection is likely far more important.[32]Baumgartner F, Konecny J. Compensatory hyperhidrosis after sympathectomy: level of resection versus location of hyperhidrosis. Ann Thorac Surg. 2007 Oct;84(4):1422. http://www.ncbi.nlm.nih.gov/pubmed/17889025?tool=bestpractice.com
Sympathetic surgery at T3 or T4 can be expected to benefit 80% to 90% of patients with axillary hyperhidrosis. However, several studies have shown that sympathetic surgery in patients with axillary hyperhidrosis is less successful and that the level of patient satisfaction is lower than it is for patients with palmar hyperhidrosis.[14]Baumgartner FJ. Surgical approaches and techniques in the management of severe hyperhidrosis. Thorac Surg Clin. 2008 May;18(2):167-81.
http://www.ncbi.nlm.nih.gov/pubmed/18557590?tool=bestpractice.com
[33]Reisfeld R. One-year follow-up after thoracoscopic sympathectomy for hyperhidrosis. Ann Thorac Surg. 2007 Jan;83(1):358-9.
http://www.ncbi.nlm.nih.gov/pubmed/17184714?tool=bestpractice.com
[34]Rex LO, Drott C, Claes G, et al. The Boras Experience of endoscopic thoracic sympathicotomy for palmar, axillary, facial hyperhidrosis and facial blushing. Eur J Surg Suppl. 1998;580:23-6.
http://www.ncbi.nlm.nih.gov/pubmed/9641381?tool=bestpractice.com
[35]Dewey TM, Herbert MA, Hill SL, et al. One-year follow-up after thoracoscopic sympathectomy for hyperhidrosis: outcomes and consequences. Ann Thorac Surg. 2006 Apr;81(4):1227-33.
http://www.ncbi.nlm.nih.gov/pubmed/16564248?tool=bestpractice.com
[36]Zacherl J, Huber ER, Imhof M, et al. Long-term results of 630 thoracoscopic sympathicotomies for primary hyperhidrosis: the Vienna experience. Eur J Surg Suppl. 1998 Apr;580:43-6.
http://www.ncbi.nlm.nih.gov/pubmed/9641386?tool=bestpractice.com
[37]Dumont P, Denoyer A, Robin P. Long-term results of thoracoscopic sympathectomy for hyperhidrosis. Ann Thorac Surg. 2004 Nov;78(5):1801-7.
http://www.ncbi.nlm.nih.gov/pubmed/15511477?tool=bestpractice.com
[38]Sugimura H, Spratt EH, Compeau CG, et al. Thoracoscopic sympathetic clipping for hyperhidrosis: long-term results and reversibility. J Thorac Cardiovasc Surg. 2009 Jun;137(6):1370-8.
http://www.ncbi.nlm.nih.gov/pubmed/19464450?tool=bestpractice.com
[40]Bell D, Jedynak J, Bell R. Predictors of outcome following endoscopic thoracic sympathectomy. ANZ J Surg. 2014 Jan-Feb;84(1-2):68-72.
http://www.ncbi.nlm.nih.gov/pubmed/23432865?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Thoracoscopic view of the left upper posterior mediastinum with the sympathetic chain visualized over the 2nd, 3rd, and 4th costal heads (R2, R3, and R4, respectively)From the personal collection of Fritz Baumgartner, MD [Citation ends].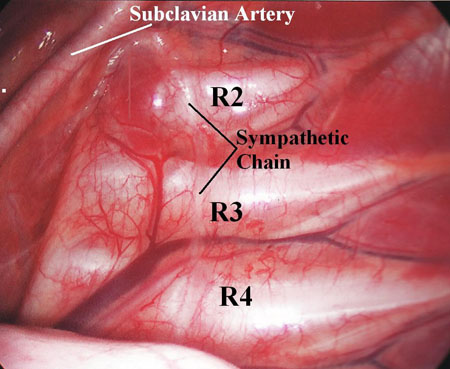
short-term anticholinergic
Treatment recommended for SOME patients in selected patient group
For those patients with symptoms exacerbated in known anxiety-provoking situations, a short-term oral anticholinergic taken as required can be considered together with any of the other therapies, although its side effects (e.g., dry eyes and mouth, urinary retention, cramps, weakness, nausea, and headache) may limit its usefulness.
Glycopyrrolate (as glycopyrronium) is also available as a topical wipe.
Primary options
glycopyrrolate: 1-2 mg orally twice or three times daily when required
OR
oxybutynin: 2.5 mg orally (immediate-release) once daily initially, increase gradually according to response, maximum 10 mg/day given in 2 divided doses; 5-10 mg orally (extended-release) once daily
OR
glycopyrronium topical: (2.4% pad) apply one pad to affected area once daily
primary: palmar hyperhidrosis
topical aluminum chloride
Topical aluminum chloride is often the first-choice treatment for palmar hyperhidrosis but tends not to be as effective as it is for treating axillary hyperhidrosis.[2]Solish N, Wang R, Murray CA. Evaluating the patient presenting with hyperhidrosis. Thorac Surg Clin. 2008 May;18(2):133-40. http://www.ncbi.nlm.nih.gov/pubmed/18557587?tool=bestpractice.com [11]Gee S, Yamauchi PS. Nonsurgical management of hyperhidrosis. Thorac Surg Clin. 2008 May;18(2):141-55. http://www.ncbi.nlm.nih.gov/pubmed/18557588?tool=bestpractice.com [19]Solish N, Bertucci V, Dansereau A, et al. A comprehensive approach to the recognition, diagnosis and severity-based treatment of focal hyperhidrosis: recommendations of the Canadian Hyperhidrosis Advisory Committee. Dermatol Surg. 2007 Aug;33(8):908-23. http://www.ncbi.nlm.nih.gov/pubmed/17661933?tool=bestpractice.com [31]National Institute for Health and Care Excellence. Endoscopic thoracic sympathectomy for primary hyperhidrosis of the upper limb. May 2014 [internet publication]. https://www.nice.org.uk/guidance/ipg487 [41]Moran KT, Brady MP. Surgical management of primary hyperhidrosis. Br J Surg. 1991 Mar;78(3):279-83. http://www.ncbi.nlm.nih.gov/pubmed/2021839?tool=bestpractice.com
Commonly used preparations include 20% aluminum chloride in ethanol and 6.25% aluminum tetrachloride.
Local stinging and burning may occur due to formation of hydrochloric acid when sweat combines with the aluminum chloride. Topical baking soda or hydrocortisone cream may help if this occurs.[11]Gee S, Yamauchi PS. Nonsurgical management of hyperhidrosis. Thorac Surg Clin. 2008 May;18(2):141-55. http://www.ncbi.nlm.nih.gov/pubmed/18557588?tool=bestpractice.com
Primary options
aluminum chloride topical: apply to the affected area(s) once daily at bedtime until desired effect is achieved, then taper to once weekly
short-term anticholinergic
Treatment recommended for SOME patients in selected patient group
For those patients with symptoms exacerbated in known anxiety-provoking situations, a short-term oral anticholinergic taken as required can be considered together with any of the other therapies, although its side effects (e.g., dry eyes and mouth, urinary retention, cramps, weakness, nausea, and headache) may limit its usefulness.
Glycopyrrolate (as glycopyrronium) is also available as a topical wipe.
Primary options
glycopyrrolate: 1-2 mg orally twice or three times daily when required
OR
oxybutynin: 2.5 mg orally (immediate-release) once daily initially, increase gradually according to response, maximum 10 mg/day given in 2 divided doses; 5-10 mg orally (extended-release) once daily
OR
glycopyrronium topical: (2.4% pad) apply one pad to affected area once daily
iontophoresis
For patients who do not respond or cannot tolerate topical aluminum chloride on their hands, iontophoresis with tap water may be used.
Using an iontophoresis device, ions are introduced into cutaneous tissues via an electrical current.
The mechanism most likely involves the ionic current temporarily blocking the sweat duct at the level of the stratum corneum.
The addition of anticholinergics or onabotulinumtoxinA to the iontophoresis tap water may improve its efficacy.[11]Gee S, Yamauchi PS. Nonsurgical management of hyperhidrosis. Thorac Surg Clin. 2008 May;18(2):141-55. http://www.ncbi.nlm.nih.gov/pubmed/18557588?tool=bestpractice.com [42]Dolianitis C, Scarff CE, Kelly J, et al. Iontophoresis with glycopyrrolate for the treatment of palmoplantar hyperhidrosis. Australas J Dermatol. 2004 Nov;45():208-12. http://www.ncbi.nlm.nih.gov/pubmed/15527429?tool=bestpractice.com
Skin irritation from galvanic currents may occur.
Iontophoresis is contraindicated in patients with pacemakers or metal implants, or who are pregnant.[11]Gee S, Yamauchi PS. Nonsurgical management of hyperhidrosis. Thorac Surg Clin. 2008 May;18(2):141-55. http://www.ncbi.nlm.nih.gov/pubmed/18557588?tool=bestpractice.com
short-term anticholinergic
Treatment recommended for SOME patients in selected patient group
For those patients with symptoms exacerbated in known anxiety-provoking situations, a short-term oral anticholinergic taken as required can be considered together with any of the other therapies, although its side effects (e.g., dry eyes and mouth, urinary retention, cramps, weakness, nausea, and headache) may limit its usefulness.
Glycopyrrolate (as glycopyrronium) is also available as a topical wipe.
Primary options
glycopyrrolate: 1-2 mg orally twice or three times daily when required
OR
oxybutynin: 2.5 mg orally (immediate-release) once daily initially, increase gradually according to response, maximum 10 mg/day given in 2 divided doses; 5-10 mg orally (extended-release) once daily
OR
glycopyrronium topical: (2.4% pad) apply one pad to affected area once daily
endoscopic thoracoscopic sympathectomy (ETS)
ETS is appropriate for severe, debilitating palmar sweating when other treatments have failed.[31]National Institute for Health and Care Excellence. Endoscopic thoracic sympathectomy for primary hyperhidrosis of the upper limb. May 2014 [internet publication]. https://www.nice.org.uk/guidance/ipg487
In these cases, the expected benefits generally outweigh the known side effects, which may include compensatory sweating.[9]Baumgartner FJ, Bertin S, Konecny J. Superiority of thoracoscopic sympathectomy over medical management for the palmoplantar subset of severe hyperhidrosis. Ann Vasc Surg. 2009 Jan-Feb;23(1):1-7. http://www.ncbi.nlm.nih.gov/pubmed/18619780?tool=bestpractice.com [14]Baumgartner FJ. Surgical approaches and techniques in the management of severe hyperhidrosis. Thorac Surg Clin. 2008 May;18(2):167-81. http://www.ncbi.nlm.nih.gov/pubmed/18557590?tool=bestpractice.com
The specific hyperhidrosis disorder determines the level of the sympathetic procedure. For example, surgery at the second (T2) or third (T3) thoracic ganglia is recommended for palmar hyperhidrosis.
ETS is also appropriate for patients with severe palmar and severe plantar hyperhidrosis (palmoplantar hyperhidrosis) when other treatments have failed. It is emphasized that the ETS procedure is meant to cure the palmar hyperhidrosis, and any benefit for the feet is never the primary intent of the surgery.
Surgery can be performed at the T2 or T3 level, although some suggest the T4 level. The best level to select is unclear and controversial. Surgery at the T2 level may be more consistently curative with less dramatic failures than at T3,[49]Baumgartner FJ, Reyes M, Sarkisyan GG, et al. Thoracoscopic sympathicotomy for disabling palmar hyperhidrosis: a prospective randomized comparison between two levels. Ann Thorac Surg. 2011 Dec;92(6):2015-9. http://www.ncbi.nlm.nih.gov/pubmed/22115211?tool=bestpractice.com [50]Yazbek G, Wolosker N, de Campos JR, et al. Palmar hyperhidrosis. Which is the best level of denervation using video-assisted thoracoscopic sympathectomy: T2 or T3 ganglion? J Vasc Surg. 2005 Aug;42(2):281-5. http://www.ncbi.nlm.nih.gov/pubmed/16102627?tool=bestpractice.com but is associated with an increased incidence of compensatory hyperhidrosis postoperatively.[48]Cerfolio RJ, De Campos JR, Bryant AS, et al. The Society of Thoracic Surgeons expert consensus for the surgical treatment of hyperhidrosis. Ann Thorac Surg. 2011 May;91(5):1642-8. https://www.annalsthoracicsurgery.org/article/S0003-4975(11)00467-X/fulltext http://www.ncbi.nlm.nih.gov/pubmed/21524489?tool=bestpractice.com [49]Baumgartner FJ, Reyes M, Sarkisyan GG, et al. Thoracoscopic sympathicotomy for disabling palmar hyperhidrosis: a prospective randomized comparison between two levels. Ann Thorac Surg. 2011 Dec;92(6):2015-9. http://www.ncbi.nlm.nih.gov/pubmed/22115211?tool=bestpractice.com [50]Yazbek G, Wolosker N, de Campos JR, et al. Palmar hyperhidrosis. Which is the best level of denervation using video-assisted thoracoscopic sympathectomy: T2 or T3 ganglion? J Vasc Surg. 2005 Aug;42(2):281-5. http://www.ncbi.nlm.nih.gov/pubmed/16102627?tool=bestpractice.com However, excellent long-term results with a low (1.3%) rate of severe compensatory sweating have been reported by some using the T2 level.[52]Atkinson JL, Fode-Thomas NC, Fealey RD, et al. Endoscopic transthoracic limited sympathotomy for palmar-plantar hyperhidrosis: outcomes and complications during a 10-year period. Mayo Clin Proc. 2011 Aug;86(8):721-9. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3146372/pdf/mayoclinproc_86_8_004.pdf http://www.ncbi.nlm.nih.gov/pubmed/21803954?tool=bestpractice.com
Successful outcomes for palmar sweating are achieved in >95% of cases.[51]Yazbek G, Wolosker N, Kauffman P, et al. Twenty months of evolution following sympathectomy on patients with palmar hyperhidrosis: sympathectomy at the T3 level is better than at the T2 level. Clinics (Sao Paulo). 2009;64(8):743-9. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2728186/pdf/cln64_8p743.pdf http://www.ncbi.nlm.nih.gov/pubmed/19690657?tool=bestpractice.com Plantar sweating is improved in the short term in approximately 80% of cases, although not as dramatically as the palmar sweating.
Because of the higher incidence of moderate or severe compensatory hyperhidrosis, some recommend avoiding T2 procedures altogether, although others report excellent results using the T2 level.[49]Baumgartner FJ, Reyes M, Sarkisyan GG, et al. Thoracoscopic sympathicotomy for disabling palmar hyperhidrosis: a prospective randomized comparison between two levels. Ann Thorac Surg. 2011 Dec;92(6):2015-9.
http://www.ncbi.nlm.nih.gov/pubmed/22115211?tool=bestpractice.com
[52]Atkinson JL, Fode-Thomas NC, Fealey RD, et al. Endoscopic transthoracic limited sympathotomy for palmar-plantar hyperhidrosis: outcomes and complications during a 10-year period. Mayo Clin Proc. 2011 Aug;86(8):721-9.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3146372/pdf/mayoclinproc_86_8_004.pdf
http://www.ncbi.nlm.nih.gov/pubmed/21803954?tool=bestpractice.com
Some even recommend levels of sympathetic intervention for palmoplantar hyperhidrosis at levels lower than T3 (i.e., over the 4th or 5th rib levels), although this may result in "moister hands".[48]Cerfolio RJ, De Campos JR, Bryant AS, et al. The Society of Thoracic Surgeons expert consensus for the surgical treatment of hyperhidrosis. Ann Thorac Surg. 2011 May;91(5):1642-8.
https://www.annalsthoracicsurgery.org/article/S0003-4975(11)00467-X/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/21524489?tool=bestpractice.com
It is suggested that proper patient selection is far more important than sympathectomy level in achieving patient satisfaction regarding compensatory sweating.[15]Baumgartner F. Compensatory hyperhidrosis after thoracoscopic sympathectomy. Ann Thorac Surg. 2005 Sep;80(3):1161.
http://www.ncbi.nlm.nih.gov/pubmed/16122529?tool=bestpractice.com
Some surgeons perform ramicotomy rather than sympathetic nerve/ganglion intervention to limit the severity of compensatory sweating. However, the incidence of recurrent sweating does seem to be higher with ramicotomy.[53]Hwang JJ, Kim DH, Hong YJ, et al. A comparison between two types of limited sympathetic surgery for palmar hyperhidrosis. Surg Today. 2013 Apr;43(4):397-402.
http://link.springer.com/article/10.1007/s00595-012-0246-1/fulltext.html
http://www.ncbi.nlm.nih.gov/pubmed/22798011?tool=bestpractice.com
Thoracoscopic sympathetic intervention can be safe and effective in younger patients, even in early teenage years, and has been shown to result in markedly improved long-term quality of life compared to nonoperative cohorts.[54]Neves S, Uchoa PC, Wolosker N, et al. Long-term comparison of video-assisted thoracic sympathectomy and clinical observation for the treatment of palmar hyperhidrosis in children younger than 14. Pediatr Dermatol. 2012 Sep-Oct;29(5):575-9.
http://www.ncbi.nlm.nih.gov/pubmed/22486301?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Thoracoscopic view of the right upper posterior mediastinum with the sympathetic chain visualized over the 2nd and 3rd rib costal heads (R2 and R3, respectively). Transection of the sympathetic chain at the level of T2 on the right and left sides is curative for palmar hyperhidrosisFrom the personal collection of Fritz Baumgartner, MD [Citation ends].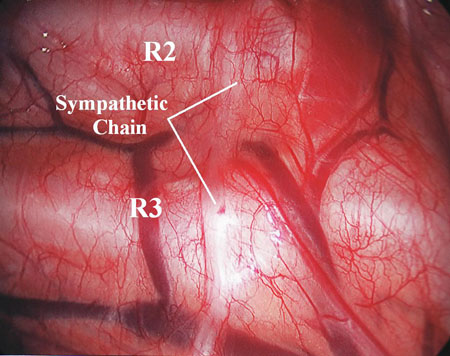 [Figure caption and citation for the preceding image starts]: Thoracoscopic view of the left upper posterior mediastinum with the sympathetic chain visualized over the 2nd, 3rd, and 4th costal heads (R2, R3, and R4, respectively)From the personal collection of Fritz Baumgartner, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Thoracoscopic view of the left upper posterior mediastinum with the sympathetic chain visualized over the 2nd, 3rd, and 4th costal heads (R2, R3, and R4, respectively)From the personal collection of Fritz Baumgartner, MD [Citation ends].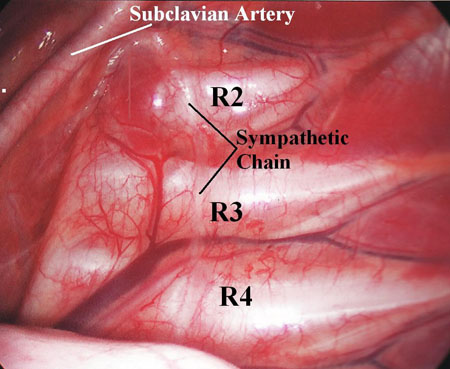
short-term anticholinergic
Treatment recommended for SOME patients in selected patient group
For those patients with symptoms exacerbated in known anxiety-provoking situations, a short-term oral anticholinergic taken as required can be considered together with any of the other therapies, although its side effects (e.g., dry eyes and mouth, urinary retention, cramps, weakness, nausea, and headache) may limit its usefulness.
Glycopyrrolate (as glycopyrronium) is also available as a topical wipe.
Primary options
glycopyrrolate: 1-2 mg orally twice or three times daily when required
OR
oxybutynin: 2.5 mg orally (immediate-release) once daily initially, increase gradually according to response, maximum 10 mg/day given in 2 divided doses; 5-10 mg orally (extended-release) once daily
OR
glycopyrronium topical: (2.4% pad) apply one pad to affected area once daily
primary: plantar hyperhidrosis
supportive care
Initial management should include keeping the feet as dry as possible by use of absorbent foot powders and shoe inserts, and frequent changing of socks and shoes.
short-term anticholinergic
Treatment recommended for SOME patients in selected patient group
For those patients with symptoms exacerbated in known anxiety-provoking situations, a short-term oral anticholinergic taken as required can be considered together with any of the other therapies, although its side effects (e.g., dry eyes and mouth, urinary retention, cramps, weakness, nausea, and headache) may limit its usefulness.
Glycopyrrolate (as glycopyrronium) is also available as a topical wipe.
Primary options
glycopyrrolate: 1-2 mg orally twice or three times daily when required
OR
oxybutynin: 2.5 mg orally (immediate-release) once daily initially, increase gradually according to response, maximum 10 mg/day given in 2 divided doses; 5-10 mg orally (extended-release) once daily
OR
glycopyrronium topical: (2.4% pad) apply one pad to affected area once daily
topical aluminum chloride with supportive care
Management of localized plantar sweating is primarily medical.
Topical aluminum chloride tends not to be as effective for plantar hyperhidrosis as it is for axillary hyperhidrosis.[41]Moran KT, Brady MP. Surgical management of primary hyperhidrosis. Br J Surg. 1991 Mar;78(3):279-83. http://www.ncbi.nlm.nih.gov/pubmed/2021839?tool=bestpractice.com
Commonly used preparations include 20% aluminum chloride in ethanol and 6.25% aluminum tetrachloride.
Local stinging and burning may occur due to formation of hydrochloric acid when sweat combines with the aluminum chloride. Topical baking soda or hydrocortisone cream may help if this occurs.[11]Gee S, Yamauchi PS. Nonsurgical management of hyperhidrosis. Thorac Surg Clin. 2008 May;18(2):141-55. http://www.ncbi.nlm.nih.gov/pubmed/18557588?tool=bestpractice.com
Patients should keep their feet as dry as possible using absorbent foot powders and/or shoe inserts, with frequent changing of socks and shoes.
Primary options
aluminum chloride topical: apply to the affected area(s) once daily at bedtime until desired effect is achieved, then taper to once weekly
short-term anticholinergic
Treatment recommended for SOME patients in selected patient group
For those patients with symptoms exacerbated in known anxiety-provoking situations, a short-term oral anticholinergic taken as required can be considered together with any of the other therapies, although its side effects (e.g., dry eyes and mouth, urinary retention, cramps, weakness, nausea, and headache) may limit its usefulness.
Glycopyrrolate (as glycopyrronium) is also available as a topical wipe.
Primary options
glycopyrrolate: 1-2 mg orally twice or three times daily when required
OR
oxybutynin: 2.5 mg orally (immediate-release) once daily initially, increase gradually according to response, maximum 10 mg/day given in 2 divided doses; 5-10 mg orally (extended-release) once daily
OR
glycopyrronium topical: (2.4% pad) apply one pad to affected area once daily
iontophoresis with supportive care
For patients who do not respond or cannot tolerate topical aluminum chloride, iontophoresis with tap water may be used.
The mechanism most likely involves the ionic current temporarily blocking the sweat duct at the level of the stratum corneum.
Oral anticholinergics or onabotulinumtoxinA added to the iontophoresis tap water may improve its efficacy.[11]Gee S, Yamauchi PS. Nonsurgical management of hyperhidrosis. Thorac Surg Clin. 2008 May;18(2):141-55. http://www.ncbi.nlm.nih.gov/pubmed/18557588?tool=bestpractice.com [42]Dolianitis C, Scarff CE, Kelly J, et al. Iontophoresis with glycopyrrolate for the treatment of palmoplantar hyperhidrosis. Australas J Dermatol. 2004 Nov;45():208-12. http://www.ncbi.nlm.nih.gov/pubmed/15527429?tool=bestpractice.com
Skin irritation from galvanic currents may occur.
Iontophoresis is contraindicated in patients with pacemakers or metal implants, or who are pregnant.[11]Gee S, Yamauchi PS. Nonsurgical management of hyperhidrosis. Thorac Surg Clin. 2008 May;18(2):141-55. http://www.ncbi.nlm.nih.gov/pubmed/18557588?tool=bestpractice.com
Patients should keep their feet as dry as possible using absorbent foot powders and/or shoe inserts, with frequent changing of socks and shoes.
short-term anticholinergic
Treatment recommended for SOME patients in selected patient group
For those patients with symptoms exacerbated in known anxiety-provoking situations, a short-term oral anticholinergic taken as required can be considered together with any of the other therapies, although its side effects (e.g., dry eyes and mouth, urinary retention, cramps, weakness, nausea, and headache) may limit its usefulness.
Glycopyrrolate (as glycopyrronium) is also available as a topical wipe.
Primary options
glycopyrrolate: 1-2 mg orally twice or three times daily when required
OR
oxybutynin: 2.5 mg orally (immediate-release) once daily initially, increase gradually according to response, maximum 10 mg/day given in 2 divided doses; 5-10 mg orally (extended-release) once daily
OR
glycopyrronium topical: (2.4% pad) apply one pad to affected area once daily
primary: craniofacial hyperhidrosis
topical aluminum chloride
Topical aluminum chloride can be used for facial sweating.
Commonly used preparations include 20% aluminum chloride in ethanol and 6.25% aluminum tetrachloride.
Local stinging and burning may occur due to formation of hydrochloric acid when sweat combines with the aluminum chloride. Topical baking soda or hydrocortisone cream may help if this occurs.[11]Gee S, Yamauchi PS. Nonsurgical management of hyperhidrosis. Thorac Surg Clin. 2008 May;18(2):141-55. http://www.ncbi.nlm.nih.gov/pubmed/18557588?tool=bestpractice.com
Primary options
aluminum chloride topical: apply to the affected area(s) once daily at bedtime until desired effect is achieved, then taper to once weekly
short-term anticholinergic
Treatment recommended for SOME patients in selected patient group
For those patients with symptoms exacerbated in known anxiety-provoking situations, a short-term oral anticholinergic taken as required can be considered together with any of the other therapies, although its side effects (e.g., dry eyes and mouth, urinary retention, cramps, weakness, nausea, and headache) may limit its usefulness.
Glycopyrrolate (as glycopyrronium) is also available as a topical wipe.
Primary options
glycopyrrolate: 1-2 mg orally twice or three times daily when required
OR
oxybutynin: 2.5 mg orally (immediate-release) once daily initially, increase gradually according to response, maximum 10 mg/day given in 2 divided doses; 5-10 mg orally (extended-release) once daily
OR
glycopyrronium topical: (2.4% pad) apply one pad to affected area once daily
endoscopic thoracoscopic sympathectomy (ETS)
ETS is used for craniofacial sweating, although there is a higher incidence of patient dissatisfaction and complaints of compensatory sweating compared with palmar hyperhidrosis.[14]Baumgartner FJ. Surgical approaches and techniques in the management of severe hyperhidrosis. Thorac Surg Clin. 2008 May;18(2):167-81. http://www.ncbi.nlm.nih.gov/pubmed/18557590?tool=bestpractice.com [33]Reisfeld R. One-year follow-up after thoracoscopic sympathectomy for hyperhidrosis. Ann Thorac Surg. 2007 Jan;83(1):358-9. http://www.ncbi.nlm.nih.gov/pubmed/17184714?tool=bestpractice.com [34]Rex LO, Drott C, Claes G, et al. The Boras Experience of endoscopic thoracic sympathicotomy for palmar, axillary, facial hyperhidrosis and facial blushing. Eur J Surg Suppl. 1998;580:23-6. http://www.ncbi.nlm.nih.gov/pubmed/9641381?tool=bestpractice.com [35]Dewey TM, Herbert MA, Hill SL, et al. One-year follow-up after thoracoscopic sympathectomy for hyperhidrosis: outcomes and consequences. Ann Thorac Surg. 2006 Apr;81(4):1227-33. http://www.ncbi.nlm.nih.gov/pubmed/16564248?tool=bestpractice.com [36]Zacherl J, Huber ER, Imhof M, et al. Long-term results of 630 thoracoscopic sympathicotomies for primary hyperhidrosis: the Vienna experience. Eur J Surg Suppl. 1998 Apr;580:43-6. http://www.ncbi.nlm.nih.gov/pubmed/9641386?tool=bestpractice.com [37]Dumont P, Denoyer A, Robin P. Long-term results of thoracoscopic sympathectomy for hyperhidrosis. Ann Thorac Surg. 2004 Nov;78(5):1801-7. http://www.ncbi.nlm.nih.gov/pubmed/15511477?tool=bestpractice.com [38]Sugimura H, Spratt EH, Compeau CG, et al. Thoracoscopic sympathetic clipping for hyperhidrosis: long-term results and reversibility. J Thorac Cardiovasc Surg. 2009 Jun;137(6):1370-8. http://www.ncbi.nlm.nih.gov/pubmed/19464450?tool=bestpractice.com [39]Smidfelt K, Drott C. Late results of endoscopic thoracic sympathectomy for hyperhidrosis and facial blushing. Br J Surg. 2011 Dec;98(12):1719-24. http://www.ncbi.nlm.nih.gov/pubmed/21928403?tool=bestpractice.com [40]Bell D, Jedynak J, Bell R. Predictors of outcome following endoscopic thoracic sympathectomy. ANZ J Surg. 2014 Jan-Feb;84(1-2):68-72. http://www.ncbi.nlm.nih.gov/pubmed/23432865?tool=bestpractice.com Treatment of craniofacial hyperhidrosis surgically should be considered very carefully as the side effects can be severe.
However, most patients with craniofacial hyperhidrosis will have significant benefit from sympathetic surgery at the T2 level. [Figure caption and citation for the preceding image starts]: Thoracoscopic view of the right upper posterior mediastinum with the sympathetic chain visualized over the 2nd and 3rd rib costal heads (R2 and R3, respectively). Transection of the sympathetic chain at the level of T2 on the right and left sides is curative for palmar hyperhidrosisFrom the personal collection of Fritz Baumgartner, MD [Citation ends].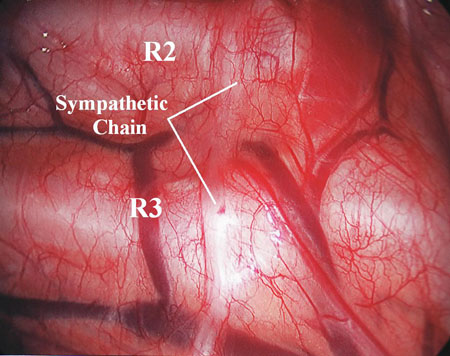
short-term anticholinergic
Treatment recommended for SOME patients in selected patient group
For those patients with symptoms exacerbated in known anxiety-provoking situations, a short-term oral anticholinergic taken as required can be considered together with any of the other therapies, although its side effects (e.g., dry eyes and mouth, urinary retention, cramps, weakness, nausea, and headache) may limit its usefulness.
Glycopyrrolate (as glycopyrronium) is also available as a topical wipe.
Primary options
glycopyrrolate: 1-2 mg orally twice or three times daily when required
OR
oxybutynin: 2.5 mg orally (immediate-release) once daily initially, increase gradually according to response, maximum 10 mg/day given in 2 divided doses; 5-10 mg orally (extended-release) once daily
OR
glycopyrronium topical: (2.4% pad) apply one pad to affected area once daily
secondary hyperhidrosis
treatment of underlying condition
This form of hyperhidrosis is a manifestation of an underlying pathology, and necessitates treating the primary cause of the disorder.
For example, focal sweating may result from acute spinal cord injury, cerebral or medullary infarcts, or other nerve injuries (e.g., posttraumatic vasomotor dystrophy), and facial gustatory sweating may be caused by Frey syndrome. More generalized sweating may be due to endocrine, neoplastic, infectious, drug, and toxicologic-related problems and, depending on the history and physical examination, may require additional testing.
short-term anticholinergic
Treatment recommended for SOME patients in selected patient group
If symptoms persist after treatment of the underlying condition, oral anticholinergic medication to reduce sweating may be appropriate, although the side effects (e.g., dry eyes and mouth, urinary retention, cramps, weakness, nausea, and headache) may limit its usefulness.
Glycopyrrolate (as glycopyrronium) is also available as a topical wipe.
Primary options
glycopyrrolate: 1-2 mg orally twice or three times daily when required
OR
oxybutynin: 2.5 mg orally (immediate-release) once daily initially, increase gradually according to response, maximum 10 mg/day given in 2 divided doses; 5-10 mg orally (extended-release) once daily
OR
glycopyrronium topical: (2.4% pad) apply one pad to affected area once daily

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer