Approach
The dermatological manifestations of HIV are protean and often multiple in patients with HIV infection. Therefore, taking a thorough history and full-body examinations are mandatory.
History
The initial approach is to elicit a standard dermatological history. If the patient presents with a rash, then duration, initial presentation, and subsequent progression should be noted. The duration of each individual lesion, along with any exacerbating or relieving factors, should be noted. Any associated pruritus, burning or pain, and enlarged or tender lymph nodes should also be noted. If the patient presents with a tumour or tumours, then duration and any change in size, shape, or colour should be determined. A personal or family history of atopic disease and psoriasis should be obtained.
History of HIV infection
Duration and seroconversion date or first positive HIV test, if known.
CD4 count at presentation, CD4 nadir, and current CD4 count and HIV viral load. Low CD4 counts are important as a predictor of diseases of advanced immunosuppression, such as opportunistic infections.
Coinfection with hepatitis B and C is important, as patients are more likely to have pruritus and/or prurigo nodularis. People with hepatitis C virus may present with cryoglobulinaemic vasculitis.[63][64][Figure caption and citation for the preceding image starts]: Prurigo nodularis showing nodules and hyperpigmentation on forearmCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].

History of opportunistic infections may indicate previous profound immunosuppression whose effects may not be fully reversible even when CD4 count recovers and HIV viral load is suppressed.
Full drug history
Should be taken, with awareness of any current drug-drug interactions.
Establishing exactly when drug treatment commenced may be helpful in determining whether drug rash may be likely and the putative drugs involved. With severely immunocompromised patients (CD4 <50 cells/microlitre) reactions may occur to almost any drug given, including antiretroviral therapy (e.g., abacavir, efavirenz, or nevirapine).[65]
Particular attention is required regarding antiretroviral therapy (ART) history, previous ART, and any reasons for treatment discontinuation or interruption. If patients have recently started ART, diseases of immune reconstitution syndrome such as eosinophilic folliculitis or flat warts should be considered.[66][67]
Patients presenting with acneiform eruption should be carefully screened for previous use of corticosteroids, such as testosterone or anabolic steroids.
Trimethoprim-sulfamethoxazole and other antibiotics have a high prevalence of morbilliform reactions in HIV-infected patients. Morbilliform reactions must be differentiated from more severe hypersensitivity reactions involved with nevirapine, in which rash is accompanied by influenza-like symptoms, blisters, oropharyngeal sores, facial swelling, and conjunctivitis.
History of allergy, especially any drug allergies.
Use of methamphetamine (crystal) or cocaine (crack) should be noted, as these are often associated with pruritus. Often, use of these drugs predicts high-risk sexual behaviours; other STIs should be considered.[Figure caption and citation for the preceding image starts]: Eosinophilic folliculitis on cheekCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Eosinophilic folliculitis on chestCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Eosinophilic folliculitis on chestCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
Sexual history
Men who have sex with men have higher risk of perianal warts and dysplasia.[68] Often, asymptomatic pharyngeal and anal sexually transmitted infections should be considered.
Ongoing assessments of sexual activity and risk for STIs should be done routinely for all patients with HIV.
Kaposi's sarcoma (KS)
Patients may often present with smaller, millimetre-sized lesions that they may not have noticed for the interval time.
Endemic KS (observed in sub-Saharan Africa), which can have an aggressive course, may affect patients who present to carers with a relatively heavy tumour burden, including large fungating tumours.[69]
Physical examination
A full-body skin examination is very helpful in the initial evaluation. Drug eruptions, viral exanthemata, syphilis, psoriasis, and scabies should be considered in patients presenting with generalised rashes. [Figure caption and citation for the preceding image starts]: Eosinophilic folliculitis on chestCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Oral hairy leukoplakiaFrom the collection of Tim Berger, MD, University of California San Francisco Department of Dermatology; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Oral hairy leukoplakiaFrom the collection of Tim Berger, MD, University of California San Francisco Department of Dermatology; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Oral hairy leukoplakiaFrom the collection of Tim Berger, MD, University of California San Francisco Department of Dermatology; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Oral hairy leukoplakiaFrom the collection of Tim Berger, MD, University of California San Francisco Department of Dermatology; used with permission [Citation ends].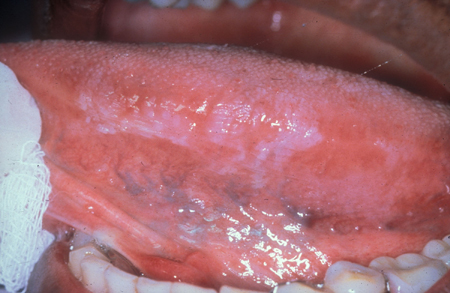 [Figure caption and citation for the preceding image starts]: Oral hairy leukoplakiaFrom the collection of Tim Berger, MD, University of California San Francisco Department of Dermatology; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Oral hairy leukoplakiaFrom the collection of Tim Berger, MD, University of California San Francisco Department of Dermatology; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Papular pruritic eruption on forearmCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Papular pruritic eruption on forearmCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Photodermatitis on sun-exposed area - lower faceCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Photodermatitis on sun-exposed area - lower faceCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Prurigo nodularis showing nodules and hyperpigmentation on forearmCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Prurigo nodularis showing nodules and hyperpigmentation on forearmCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Kaposi's sarcoma on palateCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Kaposi's sarcoma on palateCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].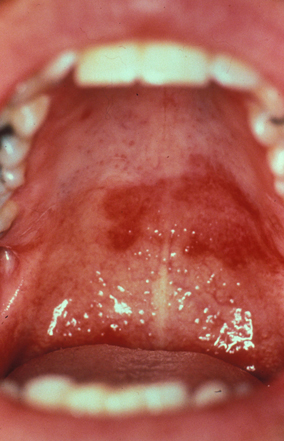 [Figure caption and citation for the preceding image starts]: Psoriatic plaques showing well-marginated silvery scale on erythematous baseUniversity of California San Francisco Department of Dermatology; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Psoriatic plaques showing well-marginated silvery scale on erythematous baseUniversity of California San Francisco Department of Dermatology; used with permission [Citation ends].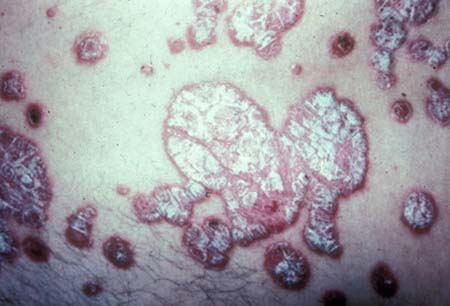 [Figure caption and citation for the preceding image starts]: Inverse psoriasis on soles of feetCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Inverse psoriasis on soles of feetCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Inverse psoriasis on palms of handsUniversity of California San Francisco Department of Dermatology; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Inverse psoriasis on palms of handsUniversity of California San Francisco Department of Dermatology; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Seborrhoeic dermatitis showing typical distribution on faceCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Seborrhoeic dermatitis showing typical distribution on faceCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Herpes simplex virus on buttocksCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Herpes simplex virus on buttocksCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Syphilis on sole of footCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Syphilis on sole of footCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Syphilis eruption on chestCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Syphilis eruption on chestCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Scabetic burrowsCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Scabetic burrowsCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Crusted scabiesCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Crusted scabiesCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
Particular attention should be paid to the following areas.
Head and scalp: scaly patches and plaques suggest psoriasis or seborrhoeic dermatitis; 'moth-eaten' alopecia may be seen in secondary syphilis.
Face and mouth: scaliness may be seen in seborrhoeic dermatitis, predominantly affecting the eyebrows, nasolabial fold, and cheeks. With increased pigmentation, photodermatitis is considered. The mouth may show oral hairy leukoplakia, candida, and/or KS. Aphthous stomatitis and herpes simplex may cause oral ulcers. Lengthened eyelashes (i.e., trichomegaly) have been reported to be associated with HIV infection.[70] Oropharyngeal/perioral lesions may be present with mpox infection.[71]
Trunk: follicular-based papules or pustules may be present. If they are very itchy, eosinophilic folliculitis is considered.
Limbs: with excoriated papules and nodules, prurigo nodularis or papular pruritic eruption of HIV should be considered.
Hands and feet: if scaly eruptions are seen, psoriasis, eczema, or tinea is a likely cause. Scabetic burrows may be present on the web spaces; if they are hyperkeratotic, crusted scabies may be present. Yellowing and thickening of the nails is common in HIV-infected people with dermatophytosis. Nail irregularities have been noted with use of certain nucleoside reverse transcriptase inhibitors and protease inhibitors and are common in psoriasis.
Genitalia: human papillomavirus-associated changes, both benign and malignant, should be sought. Ulcers or fissures in the anorectal area could be a sign of herpes simplex virus (HSV) involvement. Anal manifestation of STIs should be considered in the presence of genital ulcers. Umbilicated papules in the groin or anorectal areas could be molluscum contagiosum. Scaling in the gluteal cleft could be a sign of psoriasis. Mpox may lead to anorectal/genital involvement, causing symptoms such as tenesmus, proctitis, rectal bleeding, dysuria, paraphimosis/phimosis or urethritis.[71] This is usually associated with a rash involving the limbs, face, and trunk.
Generalised: evaluation for lymphadenopathy may detect persistent generalised lymphadenopathy.
Investigations for HIV-associated skin disease
Many conditions do not require investigation, as the diagnosis is evident from the history and examination.
Patients should have a recent cluster of differentiation 4 count, HIV viral load, and syphilis serology.
In specific patients the following tests should be carried out.
Cultures and Gram stain: if infection is suspected.
Skin biopsy: may be helpful when histopathological confirmation is needed, as in malignancy, or when further evaluation may be helpful for diagnosis.
Microscopic evaluation of skin scrapings under potassium hydroxide: when tinea is suspected.
Porphyria screen: to rule out other causes of photosensitivity.
Hepatitis serology: to assess pruritus or prurigo nodularis.
Nucleic acid amplification tests (e.g., polymerase chain reaction): when HSV or varicella zoster virus is suspected.
Fasting lipids: when HIV lipodystrophy is suspected.
Fasting plasma glucose: when HIV lipodystrophy is suspected.
STI screening: if (asymptomatic) sexually transmitted infections (gonorrhoea, chlamydia, human papillomavirus) are suspected.
Use of this content is subject to our disclaimer