Aetiology
The aetiologies of different diseases involving the skin and HIV vary. Some skin diseases are fairly specific to HIV. Other skin diseases may appear in non-HIV-infected populations but have altered presentations in those with HIV.
Local epidemiology should be considered. The diagnostic and treatment approach can differ according to local availability; guidelines are scarce.[2][3] Antiretroviral therapy may reduce the prevalence and progression of certain dermatoses in patients with HIV; prevalence of cutaneous drug reactions may increase.
HIV-specific dermatoses
These diseases include HIV-related lipodystrophy, eosinophilic folliculitis (EF), oral hairy leukoplakia, papular pruritic eruption of HIV (PPE), HIV photodermatitis, prurigo nodularis, Kaposi's sarcoma, immune reconstitution inflammatory syndrome, and aphthous ulcers. They rarely appear outside immunocompromise or HIV.
HIV-related lipodystrophy: a metabolic disturbance thought in large part to be due to undesired effects from chronic use of antiretrovirals. The dyslipidaemic metabolic derangements, fatty deposition irregularities, and other symptoms and signs associated with HIV-related lipodystrophy are best noted in the drug classes nucleoside reverse transcriptase inhibitors, through mitochondrial dysfunction, and protease inhibitors, through fatty enzyme metabolic interruption.[4][5][Figure caption and citation for the preceding image starts]: HIV-associated lipodystrophy revealing facial atrophyUniversity of California San Francisco Department of Dermatology; used with permission [Citation ends].

EF: pathogenesis is not clearly understood. Although some suggest that EF pathogenesis involves a combination of immune disturbance and hypersensitivity reaction from exposure to the Demodex folliculorum mite, a common inhabitant of human skin, the literature on aetiology is inconsistent and needs clarification.[6][7][Figure caption and citation for the preceding image starts]: Eosinophilic folliculitis on cheekCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Eosinophilic folliculitis on chestCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Eosinophilic folliculitis on chestCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
Oral hairy leukoplakia: driven in large part by Epstein-Barr virus. [Figure caption and citation for the preceding image starts]: Oral hairy leukoplakiaFrom the collection of Tim Berger, MD, University of California San Francisco Department of Dermatology; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Oral hairy leukoplakiaFrom the collection of Tim Berger, MD, University of California San Francisco Department of Dermatology; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Oral hairy leukoplakiaFrom the collection of Tim Berger, MD, University of California San Francisco Department of Dermatology; used with permission [Citation ends].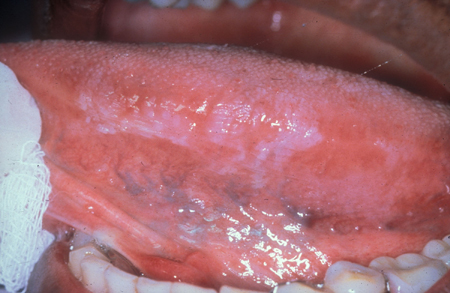 [Figure caption and citation for the preceding image starts]: Oral hairy leukoplakiaFrom the collection of Tim Berger, MD, University of California San Francisco Department of Dermatology; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Oral hairy leukoplakiaFrom the collection of Tim Berger, MD, University of California San Francisco Department of Dermatology; used with permission [Citation ends].
PPE: thought to be driven by arthropod bite reaction and HIV-related immune disruption.[8][Figure caption and citation for the preceding image starts]: Papular pruritic eruption on forearmCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].

HIV photodermatitis: unclear aetiology. If scarring and milia are seen on the face and/or hands, porphyria cutanea tarda is considered.[Figure caption and citation for the preceding image starts]: Photodermatitis on sun-exposed area - armUniversity of California San Francisco Department of Dermatology; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Photodermatitis on sun-exposed area - dorsum of handUniversity of California San Francisco Department of Dermatology; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Photodermatitis on sun-exposed area - dorsum of handUniversity of California San Francisco Department of Dermatology; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Photodermatitis on sun-exposed area - lower faceCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Photodermatitis on sun-exposed area - lower faceCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
Prurigo nodularis: significantly associated with HIV infection.[9][10] Sometimes associated with hepatitis C or B coinfection. [Figure caption and citation for the preceding image starts]: Prurigo nodularis showing nodules and hyperpigmentation on forearmCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].

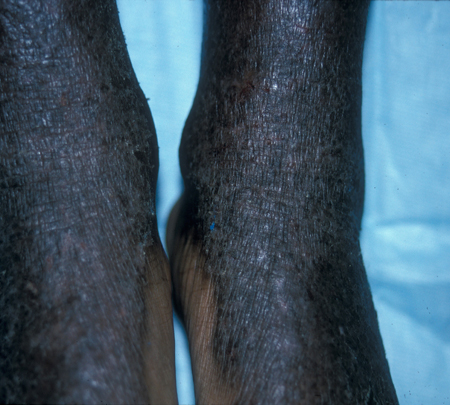
Kaposi's sarcoma: one of the most common HIV-associated malignancies in adults and children.[11][12][Figure caption and citation for the preceding image starts]: Kaposi's sarcoma on lower extremitiesCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Kaposi's sarcoma on palateCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Kaposi's sarcoma on palateCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].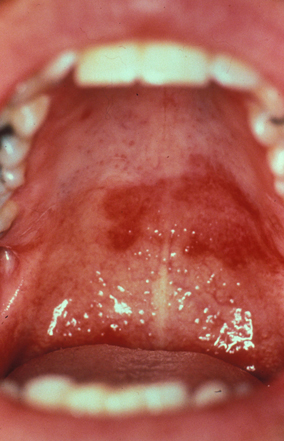
Immune reconstitution inflammatory syndrome: presents with worsening of the patient's general condition or the presentation of a new opportunistic infection after starting combination antiretroviral therapy. Patients with a CD4 count of <50 cells/microlitre have a higher risk.[13]
Aphthous ulcers: occur often during acute HIV infection. They are also directly related to immunological state. Patients with recurrent aphthous stomatitis frequently present with nutritional deficits.[14]
Non-HIV-specific dermatoses that have altered presentation with HIV
Skin diseases that occur in both immunocompetent and HIV-infected populations, which may present more commonly or in a more severe form in HIV-infected people.
Psoriasis: in HIV-infected people, frequency is similar to that in the general population (1% to 3%).[15][16][Figure caption and citation for the preceding image starts]: Psoriatic plaques showing well-marginated silvery scale on erythematous baseUniversity of California San Francisco Department of Dermatology; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Inverse psoriasis on soles of feetCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Inverse psoriasis on soles of feetCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Inverse psoriasis on palms of handsUniversity of California San Francisco Department of Dermatology; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Inverse psoriasis on palms of handsUniversity of California San Francisco Department of Dermatology; used with permission [Citation ends].
Seborrhoeic dermatitis: a common dermatosis in the general population (1% to 3%); seborrhoeic dermatitis prevalence of 1% to 25% has been reported among HIV-infected people in the antiretroviral therapy era.[17][18][Figure caption and citation for the preceding image starts]: Seborrhoeic dermatitis showing typical distribution on faceCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].

Atopic dermatitis: high prevalence in adult and paediatric populations; in one chart review, 20% of HIV-infected children and adolescents had atopic dermatitis.[19][Figure caption and citation for the preceding image starts]: Atopic dermatitis on antecubital fossaCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].

Xerosis: high prevalence in HIV-infected patients (23% to 52%).[20][21] Possible diminished sweating and sebaceous gland secretion, and malabsorption of essential fatty acids, in those with wasting.[Figure caption and citation for the preceding image starts]: XerosisCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
Perioral dermatitis: more common in women. [Figure caption and citation for the preceding image starts]: Perioral dermatitisCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].

Acne vulgaris: flares are common in HIV-infected people, especially as antiretroviral therapy-treated patients become immune constituted. It is unusual to see acne vulgaris in patients with low CD4 counts.[22] [Figure caption and citation for the preceding image starts]: Acne vulgaris on faceCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].

Cutaneous manifestations of reactive arthritis (Reiter's syndrome): include hyperkeratotic skin and erythematous dermatitis. Occurs mainly in human leukocyte antigen-B27-positive men, and there may be a positive family history. Co-occurrence in HIV infection has also been noted. HIV-infection symptoms may appear simultaneously with symptoms of reactive arthritis, or onset of reactive arthritis may occur shortly after HIV infection becomes symptomatic.[15][23]
Molluscum contagiosum virus (MCV): severe MCV infection affected around 5% to 18% of people with HIV in the pre-antiretroviral therapy era.[24] Extensive disease usually occurs in individuals with CD4 counts significantly below 200 cells/microlitre.[24] Infection with Histoplasma, Cryptococcus, and Talaromyces marneffei (formerly Penicillium) should also be considered in the differential in the presence of significant immunocompromise. Talaromycosis (formerly penicilliosis) is more prevalent in Southeast Asia; cryptococcal infection has a worldwide distribution; histoplasmosis tends to appear around river valleys and has been reported in North and South America, Southeast Asia, and Central Africa.[Figure caption and citation for the preceding image starts]: Molluscum contagiosum on cheekCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].

Human papillomavirus (HPV): warts are common in HIV-infected people, and may be more difficult to treat as HIV advances; Bowen's disease, a form of squamous cell carcinoma in situ, has a variant known as bowenoid papulosis, involving flat, dark papules on the pelvic region; epidermodysplasia verruciformis is an unusual manifestation of HPV with extensive flat warts on the neck, dorsal hands, face, and extremities. [Figure caption and citation for the preceding image starts]: Human papillomavirus on soles of feetCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].

Herpes simplex virus: dissemination is rare even in severely immunocompromised patients. [Figure caption and citation for the preceding image starts]: Herpes simplex virus on buttocksCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Herpes simplex virus mimicking staphylococcal infectionCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Herpes simplex virus mimicking staphylococcal infectionCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
Varicella zoster virus: most HIV-infected patients have had varicella previously, manifesting as zoster at relatively normal CD4 counts. Incidence of herpes zoster has decreased among HIV-infected children.[25][Figure caption and citation for the preceding image starts]: Varicella zoster virus on the backFrom the collection of Tim Berger, MD, University of California San Francisco Department of Dermatology; used with permission [Citation ends].

Staphylococcal infection: may cause bullous impetigo, ecthyma, folliculitis, and botryomycosis. [Figure caption and citation for the preceding image starts]: Staphylococcal folliculitisCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Staphylococcal ulcersCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Staphylococcal ulcersCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Botryomycoses in axillaUniversity of California San Francisco Department of Dermatology; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Botryomycoses in axillaUniversity of California San Francisco Department of Dermatology; used with permission [Citation ends].
Bacillary angiomatosis: reported in South America, Europe, India, and Africa.[26][27][28][29][30] Should be considered in HIV-positive patients with fever of unknown origin; resembles Kaposi's sarcoma, cutaneous lymphoma, or pyogenic granulomata; may be associated with brain, liver, lymphatic, and pulmonary involvement.[Figure caption and citation for the preceding image starts]: Bacillary angiomatosisUniversity of California San Francisco Department of Dermatology; used with permission [Citation ends].

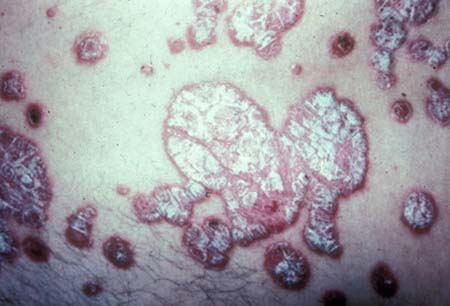
Syphilis: increased prevalence among HIV-infected populations, and worldwide increase in reported cases.[31][32][33][34] In urban settings, most cases are in men who have sex with men.[35][36] Methamphetamine use is implicated in some reports evaluating rising incidence in the US and Europe.[37][38] Among HIV-infected women, studies report that sex work, limited or no condom use, and substance use are risk factors.[31][39] Primary, secondary, and tertiary skin manifestations are similar in people with HIV and without HIV infection, although presentation may be atypical in HIV-infected individuals. It is important to exclude neurosyphilis.[Figure caption and citation for the preceding image starts]: Syphilis on sole of footCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Syphilis eruption on chestCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Syphilis eruption on chestCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
Gonorrhoea: increased prevalence among HIV-infected populations (mostly men who have sex with men). Asymptomatic infections are common in pharynx and anus. Antibiotic resistance is a rising challenge.[40]
Chlamydia/lymphogranuloma venereum (LGV): chlamydia causes trachoma (serovars A, B, Ba, or C), urethritis (serovars D-K), and lymphogranuloma venereum (LGV; serovars L1, 2, and 3). HIV-infected men who have sex with men are disproportionately affected by LGV. Clinical features of LGV have historically been divided into 3 stages: ulcer, local lymph node involvement and necrotic areas, and chronic oedema with sclerosing fibrosis. Anal infections present as ulcerative proctitis or proctocolitis. There is a high rate of concurrent STIs including hepatitis C.[41]
Chancroid: a sexually acquired disease caused by Haemophilus ducreyi. Soft and painful ulcers with regional lymphadenitis are typical manifestations. Treatment failure is more common in people with HIV infection.[42]
Scabies: in contrast to those without HIV infection, involvement above the neck is possible in people with HIV infection. [Figure caption and citation for the preceding image starts]: Scabetic burrowsCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Crusted scabiesCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Crusted scabiesCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
Leishmaniasis: occurs in patients who have history of travel to, or residence in, endemic areas with sand fly exposure. Visceral, mucocutaneous, and cutaneous coinfection with HIV has been noted.[43][44][45] Spain, around the Mediterranean basin, has been noted to be a high-prevalence area with regard to visceral leishmaniasis with HIV coinfection; areas where leishmaniasis has been reported include countries around the Mediterranean, Turkey, Iran, and Saudi Arabia.[46][47]
Dermatophytosis: prevalence is the same among people infected with HIV and people who are not, but there is increased variability of presentation and disease severity in HIV-infected individuals. Nail involvement is common in HIV-infected people, with reported prevalence as high as 41%.[48] If skin involvement is refractory to traditional treatments, other differential entities including psoriasis or seborrhoeic dermatitis must be considered.
Candida: oral and oesophageal candidiasis is also common in HIV.[49]
Basal cell carcinoma: presentation is the same as in patients not infected with HIV, although risk is increased in HIV-infected individuals compared with that of the general population.[50][51][Figure caption and citation for the preceding image starts]: Basal cell carcinomaCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].

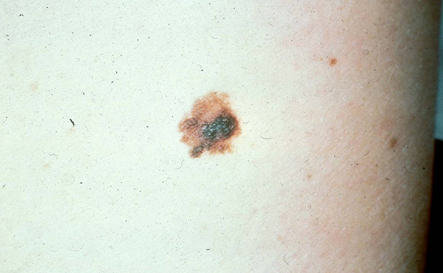
Melanoma: HIV-infected individuals may be at increased risk for melanoma, but this has not been consistently demonstrated.[50][52][53][54] Acral-lentiginous melanoma may present in Asian or dark-skinned populations.[Figure caption and citation for the preceding image starts]: MelanomaCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].
Squamous cell carcinoma: presentation is the same in HIV-infected patients as in people without HIV, although risk is increased in HIV-infected individuals compared with that of the general population.[50][51][Figure caption and citation for the preceding image starts]: Squamous cell carcinomaCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].

Merkel cell carcinoma (MCC): an aggressive non-melanoma skin tumour, the majority of MCC cases are associated with Merkel cell polyomavirus.[55][56] Immunocompromised individuals such as HIV-infected patients have an increased risk for MCC development.[55]
Leiomyosarcoma: has been reported in children with HIV; most neoplasms have been found in visceral organs, but leiomyosarcoma may occur cutaneously or subcutaneously.[57] The development is Epstein-Barr virus-associated.[58]
Stevens-Johnson syndrome/toxic epidermal necrolysis: much more prevalent per drug exposure in HIV-infected people than in the general population.[59][Figure caption and citation for the preceding image starts]: Toxic epidermal necrolysisCommon skin diseases in HIV-infected patients in the antiretroviral era. IAS-USA 2007; used with permission [Citation ends].

Mpox: it is currently unknown whether HIV status increases the risk of infection.[60] However, individuals with HIV-associated immunosuppression (CD4 cell count <200 cells/mm³ and especially <50 cells/mm³), or using immunosuppressants, may be at risk of developing protracted or life-threatening symptoms, regardless of disease severity at presentation.[60]
Use of this content is subject to our disclaimer