Tests
1st tests to order
skin test for Aspergillus fumigatus sensitivity
Test
Initial skin testing for Aspergillus sensitization is performed via a skin prick test; a positive result is indicated by an immediate cutaneous wheal-and-flare reaction relative to a positive control (e.g., a histamine) and negative control (e.g., saline), indicative of type I hypersensitivity to Aspergillus antigens.
The sensitivity of Aspergillus skin testing for allergic bronchopulmonary aspergillosis is very high (>95% in prior studies), but the specificity is relatively low.
Result
positive wheal and flare reaction
serum total IgE
Test
In practice, serologic markers of allergic hypersensitivity to Aspergillus, including total serum IgE and Aspergillus-specific IgE, are typically sent concurrently or in lieu of Aspergillus skin testing.
IgE levels are significantly higher in patients with allergic bronchopulmonary aspergillosis than in those with asthma, who have only a positive skin test to A fumigatus, and in normal controls.[24] If serum total IgE is between 200 and 500 kilounits/L for a patient with CF, the serum IgE test is repeated. If suspicion is high, then other diagnostic tests, such as Aspergillus-specific IgE and serum precipitating antibodies (serum precipitins) to A fumigatus, should be considered.[34] In practice, patients with ABPA almost always have IgE levels greater than 500, with few caveats.
Result
elevated
CBC with peripheral blood eosinophil count
Test
A complete blood count is also indicated to assess the peripheral blood eosinophil count. In the absence of oral corticosteroid use (which can lower eosinophil counts), peripheral eosinophilia has been reported in 43% to 100% of cases, a total eosinophil count of over 500 is one of the criteria for diagnosis of allergic bronchopulmonary aspergillosis in patients with asthma.[28][29]
Result
elevated
chest x-ray
Test
Chest x-ray is usually undertaken early in the workup of chest symptoms. Although this is not essential for the diagnosis of allergic bronchopulmonary aspergillosis, when a chest x-ray is obtained as part of an evaluation infiltrates may be visible, commonly involving the upper or middle lobe.[1] These findings may be transient or permanent. If serum eosinophilia is present at the same time, the lung infiltrates may be termed pulmonary eosinophilia. Mucus plugging and signs of bronchiectasis may also be noted.[1][Figure caption and citation for the preceding image starts]: Chest x-ray in a patient with ABPA: ring shadows (long arrows) represent bronchiectatic airways seen in cross-section; tram lines (short arrow) seen longitudinallyFrom American College of Chest Physicians. PCCU Volume 17, Lesson 17: Allergic bronchopulmonary aspergillosis. Used with permission [Citation ends].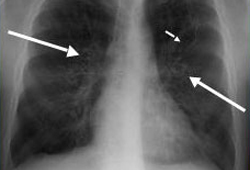 [Figure caption and citation for the preceding image starts]: Chest x-ray in a patient with ABPA: classic glove-finger pattern represents central bronchiectatic airways impacted with mucusFrom American College of Chest Physicians. PCCU Volume 17, Lesson 17: Allergic bronchopulmonary aspergillosis. Used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Chest x-ray in a patient with ABPA: classic glove-finger pattern represents central bronchiectatic airways impacted with mucusFrom American College of Chest Physicians. PCCU Volume 17, Lesson 17: Allergic bronchopulmonary aspergillosis. Used with permission [Citation ends].
Result
patchy consolidation; upper lobe/perihilar infiltrates; “toothpaste shadows”; “gloved finger shadows”; segmental or lobar atelectasis; bronchial wall thickening “tramline shadows
high-resolution CT chest
Test
High-resolution CT of the chest detects whether central bronchiectasis (i.e., occurring within the inner two-thirds of the lungs) is present.[1] Additional findings that may be noted on chest CT include mucus plugging of the bronchi (finger-in-glove appearance) or bronchiolar mucus impaction (tree-in-bud shadow), pulmonary infiltrates, and peribronchial thickening.[1] High-attenuation mucus, that is mucus which is visually denser than paraspinal skeletal muscle, or measuring >70 Hounsfield units, is considered the closest thing to a pathognomonic sign for allergic bronchopulmonary aspergillosis, and has 100% specificity. When present at the time of diagnosis it also predicts poor outcomes.[31][32] [Figure caption and citation for the preceding image starts]: CT chest in a patient with ABPA: dilated, mucoid-impacted bronchiectatic airwaysFrom American College of Chest Physicians. PCCU Volume 17, Lesson 17: Allergic bronchopulmonary aspergillosis. Used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: CT chest in a patient with ABPA: glove-finger shadow due to mucoid impaction in central bronchiectasis in a patient with asthmaFrom The Radiology Assistant: Chest - HRCT Part 1. Used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: CT chest in a patient with ABPA: glove-finger shadow due to mucoid impaction in central bronchiectasis in a patient with asthmaFrom The Radiology Assistant: Chest - HRCT Part 1. Used with permission [Citation ends].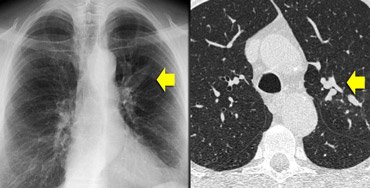
Result
central bronchiectasis; mucus plugging “finger in glove”; centrilobular nodules with tree-in-bud opacities; bronchial wall thickening; mosaic attenuation with air trapping; high-attenuation mucus
Aspergillus-specific IgE
Test
In practice Aspergillus-specific IgE ( >0.35 kilounit/L) is generally required for the diagnosis of allergic bronchopulmonary aspergillosis (ABPA). However, there is no specifically recommended cutoff to diagnose ABPA, except that the Aspergillus-specific IgE should be positive.
Result
elevated
Tests to consider
sputum culture and microscopy
Test
Test is not required to meet criteria for diagnosis, and these findings are not specific for allergic bronchopulmonary aspergillosis (ABPA) but are commonly found in patients with ABPA.[25]
Result
mucus plugs on gross exam; evidence of Aspergillus fumigatus fungal elements and eosinophils
Use of this content is subject to our disclaimer