Approach
The diagnosis of LQTS is not straightforward, as nearly 2.5% of the normal population may have a mildly prolonged QT interval, and nearly 25% of patients genotypically positive for LQTS may have normal-appearing QT intervals.[31] The QT interval is affected by heart rate (the slower the heart rate the longer the QT interval); therefore, rate-corrected QT interval (QTc) is used. Patients with LQTS may be risk-stratified for the probability of a future cardiac event (syncope, cardiac arrest, or sudden death) according to genotype, sex, age, and length of the QTc. It is also important to take into consideration any history of past symptoms when assessing the patient's risk of a future cardiac event. A careful history can help to elucidate the presence of LQTS and identify its genetic subtype in the congenital form of the condition, or highlight the cause of QT interval prolongation in acquired LQTS. An ECG should be undertaken in all suspected cases.
The Schwartz criteria, based on ECG findings (length of corrected QT interval [QTc], presence of torsades de pointes, visible T-wave alternans, presence of notched T waves, low heart rate for age in children), clinical history (presence of syncope, congenital deafness), and family history (of LQTS or sudden death) can be used to aid the diagnosis of LQTS.[32][33]
Presenting features
LQTS commonly presents in young people with cardiac arrest or unexplained syncope and is frequently misdiagnosed as epilepsy. It should therefore be considered in all such presentations, and a thorough history, including a review of premonitory symptoms and a corroborative history, is essential as it can help to differentiate between cardiac syncope, epilepsy, and other causes of syncope, some of which may be benign conditions.
Cardiac syncope is characterised by premonitory symptoms such as palpitations, chest pain, and dyspnoea. During the syncopal episode, pallor and cyanosis are common features, and the recovery period is brief and characterised by flushing.
In a patient with documented LQTS and syncope, it is important to try to identify triggers for syncope, as this may suggest a certain subtype of the syndrome.
Patients with LQT1 typically have events (i.e., syncope or sudden death) during heightened adrenergic tone such as in exercise, particularly swimming.[34]
Patients with LQT2 commonly have events during arousal or when startled, as by a telephone or alarm clock.[34]
Female patients with LQTS are more prone to developing arrhythmic symptoms during the first 9 postnatal months, particularly patients with LQT2.[35]
Patients with LQT3 commonly have events at rest and during bradycardia.[34]
Both congenital and acquired LQTS may present with palpitations secondary to premature ventricular complex and tachyarrhythmias including torsades de pointes, although the more common symptom is syncope (or cardiac arrest).
Acquired LQTS secondary to electrolyte imbalance may present with associated symptoms of hypokalaemia, hypomagnesaemia, and/or hypocalcaemia.
Hypokalaemia is normally asymptomatic but it may cause muscle weakness if severe.
Hypomagnesaemia may present with muscle weakness secondary to associated hypokalaemia, as well as tetany (manifested as carpopedal spasm) and numbness (periorally and in the extremities) secondary to associated hypocalcaemia.
Complete atrioventricular (AV) block may present with palpitations, syncope or presyncope, angina, and symptoms of reduced cardiac output (cold and clammy extremities, fatigue, listlessness, poor effort tolerance, dizziness, oliguria).
LQTS may also be discovered as an incidental ECG finding during the routine investigation of an unrelated presenting complaint such as a cardiac murmur, or during genetic diagnostic testing for another condition.[36]
Medication history
Drugs known to prolong the QT interval or cause depletion of potassium and/or magnesium may precipitate symptoms in patients with congenital LQTS or be the primary cause of acquired LQTS:
Quinidine, procainamide, sotalol, amiodarone, disopyramide, dofetilide, phenothiazines, tricyclic antidepressants, and methadone.[21][22] Credible Meds (Arizona CERT): drugs that prolong the QT interval Opens in new window
Certain cancer treatments are also known to cause QT prolongation, e.g., kinase inhibitors, growth factor inhibitors, androgen-deprivation therapies, and chimeric antigen receptor T-cell therapies.[23][24]
Medical history
Some medical conditions are known to cause acquired LQTS:
Any sudden bradycardia or AV nodal block may result in QT prolongation or pause-dependent QT prolongation.
Central nervous system lesions, such as intracranial haemorrhage (especially subarachnoid haemorrhage) and ischaemic strokes.
Knowledge of the patient's medical history may also be helpful in identifying possible therapeutic drugs known to prolong the QT interval that the patient may be taking.
Family history
Review of the family history is extremely important to assist in making the diagnosis when it is in doubt, understand the penetrance of the condition, and screen, treat, and potentially avert cardiac arrest in family members.
If possible, the ECGs and medical records of all family members should be reviewed.
On occasion, a family member may have more pathological findings than the affected proband; more commonly, the proband is the most severely involved.
Developing a family pedigree may help in discovering other affected but undiagnosed family members.
There may be a family history of complete AV block, which may indicate a diagnosis of acquired LQTS secondary to this condition.
Physical examination
Patients with Jervell and Lange-Nielsen syndrome have a very severe form of LQTS associated with sensorineural deafness.[9]
Patients with Andersen-Tawil syndrome have periodic paralysis (transient paralysis involving any part of the body and lasting seconds to hours, typically resolving spontaneously and sometimes associated with confusion and altered mental status) and ventricular tachyarrhythmias, and have a variety of dysmorphic features including micrognathia, low-set ears, widely spaced eyes, clinodactyly, syndactyly, and scoliosis.[10]
Severe hypokalaemia may cause muscle weakness.
Patients with hypocalcaemia may have positive Chvostek's sign (twitching of facial muscles in response to tapping the facial nerve in the area of the parotid gland) and Trousseau's sign (carpopedal spasm in response to inflation of a blood pressure (BP) cuff creating pressure in the upper limb greater than systolic BP).
Signs of reduced cardiac output (cold, clammy, pale, or cyanosed extremities; hypotension; confusion) may be present in complete AV block.
Schwartz criteria
The Schwartz criteria are diagnostic criteria for LQTS and are distinct from the criteria used to risk-stratify patients with known LQTS. Points are assigned to ECG, clinical, and familial findings. Patients with 3.5 or more points have a high probability of having LQTS, those with 1.5 to 3 points have an intermediate probability, and those with 1 or no points have a low probability of having LQTS.[32][33]
ECG findings (in the absence of medications or disorders known to affect these features)
Corrected QT interval (QTc), defined as QT interval (in seconds) divided by the square root of the RR interval (in seconds):
≥480 ms = 3 points
460-479 ms = 2 points
450-459 ms (in males) = 1 point.
QTc 4th minute of recovery from exercise stress test ≥480 ms = 1 point
Torsades de pointes = 2 points
Visible T-wave alternans = 1 point
Notched T wave in 3 leads = 1 point
Low heart rate for age (resting heart rate below the 2nd percentile for age) = 0.5 points.
Clinical history
Syncope (cannot receive points for both syncope and torsades de pointes)
With stress = 2 points
Without stress = 1 point.
Congenital deafness = 0.5 points.
Family history (the same family member cannot be counted for LQTS and sudden death)
Family members with definite LQTS = 1 point
Unexplained sudden cardiac death under age 30 years among immediate family = 0.5 points.
Resting ECG
A resting ECG is crucial in the diagnosis of LQTS and should be undertaken in all suspected cases in order to confirm QT interval prolongation, help identify the LQTS subtype, and uncover any causative or contributory reversible factors. When measuring the QT interval, it may be helpful for the patient to move rapidly from lying to standing.[2]
In a patient with documented LQTS, it is very important to obtain ECGs from parents, siblings, and especially any family member with presyncope or syncope.
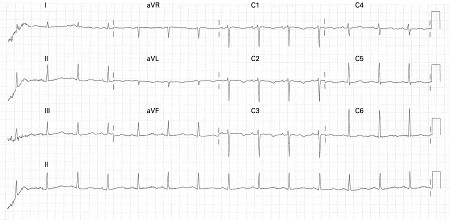
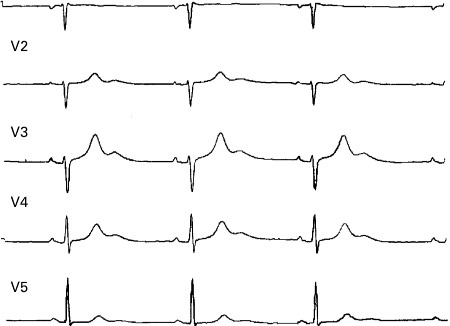
Careful attention must be given to the QT interval and the corrected QT interval (QTc). ECG findings associated with a high risk of life-threatening arrhythmias include T-wave alternans and functional 2:1 block.[5][Figure caption and citation for the preceding image starts]: ECG showing QT prolongation (QTc = 519 ms)Chong DW, Ankolekar SJ, McDonald J. BMJ Case Reports. 2009; doi:10.1136/bcr.01.2009.1426 [Citation ends].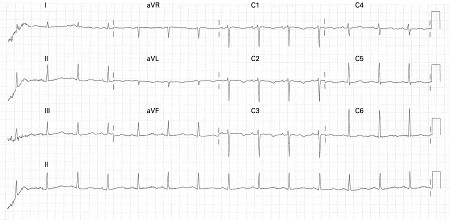 [Figure caption and citation for the preceding image starts]: ECG showing a corrected QTc interval of 760 msIniesta I, Yotti R, Garcia-Pastor A. BMJ Case Reports. 2009; doi:10.1136/bcr.06.2008.0285 [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing a corrected QTc interval of 760 msIniesta I, Yotti R, Garcia-Pastor A. BMJ Case Reports. 2009; doi:10.1136/bcr.06.2008.0285 [Citation ends].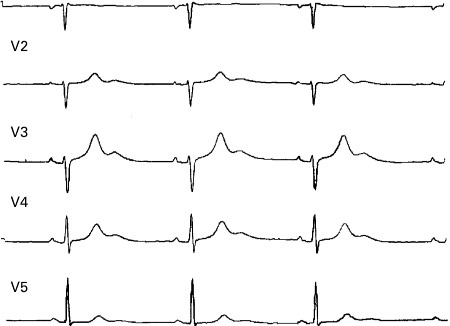 Inspection and appreciation of the T wave and whether it is monophasic or multiphasic may also be helpful.
Inspection and appreciation of the T wave and whether it is monophasic or multiphasic may also be helpful.
The QT interval is the ECG representation of ventricular depolarisation and subsequent repolarisation and may be measured in any lead in which it looks prolonged.[Figure caption and citation for the preceding image starts]: ECG showing QT prolongation (QTc = 519 ms)Chong DW, Ankolekar SJ, McDonald J. BMJ Case Reports. 2009; doi:10.1136/bcr.01.2009.1426 [Citation ends].
QT interval is measured using either tangent or threshold methods.The threshold method, measured from the onset of the initial wave of the QRS complex to where the T wave returns to the isoelectric baseline, has probably been the most commonly used.[1][37] In the tangent method, the downslope of the T wave is extrapolated to the isoelectric baseline and this intersection is used for the end of the T wave. One study comparing the two methods found that the tangent method resulted in shorter QT intervals than the threshold method, and both methods were found to have high validity and diagnostic accuracy; however, the two methods need different cut-off values for use in practice.[38]
The QT interval can also be measured with digital recordings using on screen calipers. Automated QT intervals are typically longer than manual measurements in lead II or V5 since they use the earliest lead for QRS onset and the latest lead for T-wave offset.[1] Some computerised ECG systems allow visualisation of the automated QT interval (and other interval) measurements so they can be verified.
The most commonly used formula to calculate the QTc is Bazett's formula: QT divided by the square root of the RR interval, where all intervals must be in seconds. The RR interval is the interval between each QRS complex, and should ideally be that immediately preceding the QT interval and averaged for 3 to 5 complexes. Sinus arrhythmia may lead to overestimation (or underestimation) of the QTc with 3 or even 5 complexes, so a broader average RR interval may be used in such cases.[Figure caption and citation for the preceding image starts]: ECG showing a corrected QTc interval of 760 msIniesta I, Yotti R, Garcia-Pastor A. BMJ Case Reports. 2009; doi:10.1136/bcr.06.2008.0285 [Citation ends].
Attention must be given to convert all measurements to seconds, otherwise the QTc measurement will be erroneous and meaningless. Online calculators are now available. [ QT Interval Correction Opens in new window ]
Each subtype of LQTS shows different characteristic ECG changes, although these are not universally present.
LQT1 is characterised by prolonged QT intervals associated with a broad-based T wave.[16][Figure caption and citation for the preceding image starts]: ECG findings in type 1 long QT syndromeFrom the collection of Dr James P. Daubert [Citation ends].
LQT2 is characterised by low-amplitude and notched T waves.[16][Figure caption and citation for the preceding image starts]: ECG findings in type 2 long QT syndromeFrom the collection of Dr James P. Daubert [Citation ends].
LQT3 is characterised by long ST segments with a late-appearing T wave resulting in a long QT interval.[16][Figure caption and citation for the preceding image starts]: ECG findings in type 3 long QT syndromeFrom the collection of Dr James P. Daubert [Citation ends].
Complete AV block, which can result in prolongation of the QT interval, or pause-dependent QT prolongation, resulting in acquired LQTS, shows characteristic ECG changes:
Sinus rhythm with normal atrial rate (represented by P-wave rate)
No relationship between P waves and QRS complexes
Widening of the QRS complex
Ventricular rate (represented by QRS complex rate) <50 bpm.
Electrolyte abnormalities associated with acquired LQTS show characteristic ECG changes.
Hypokalaemia is characterised by ST depression, flattened T waves, prominent U waves, and a prolonged QT interval.
Hypomagnesaemia in itself does not have well-defined ECG abnormalities but, as it is often associated with hypokalaemia and hypocalcaemia, ECG changes associated with these may be present.
Hypocalcaemia causes isolated prolongation of the QT interval.
Serum electrolyte measurement
Hypokalaemia, hypomagnesaemia, and hypocalcaemia may precipitate symptoms in patients with unrecognised congenital LQTS or be the primary cause of acquired LQTS. Serum electrolytes should therefore be measured in all patients found to have a prolonged QT interval on ECG.
Holter monitor
All patients with suspected or confirmed congenital LQTS should undergo Holter monitoring, the main purpose of which is to evaluate the behaviour of the QT interval during:
Bradycardia (at night)
Tachycardia
Sudden pauses (e.g., post-extrasystolic).
Marked changes in QT morphology during the above changes in heart rate aid diagnosis.[39]
Holter monitoring may also allow the clinician to identify non-sustained ventricular arrhythmias in patients with LQTS who are asymptomatic, thereby assisting the decision-making process as to whether medical and/or device therapy should be initiated. A Holter monitor-derived 'QT clock' may be used to improve detection of QT prolongation.[39]
Exercise tolerance testing
All patients with suspected or confirmed congenital LQTS should undergo an exercise tolerance test to identify abnormal QT interval prolongation during exercise and recovery, which is helpful in:
Diagnosing LQTS, especially LQT1, in which the QT interval and QTc increase more than those of the controls or LQT2 and LQT3 patients
Diagnosing LQTS when the QT interval is borderline prolonged
Assisting in the prescription of a maximum exercise level for patients presenting with exercise-induced symptoms of presyncope or syncope by simulating similar circumstances in a controlled environment.
Echocardiography
Echocardiography is helpful to assess for and rule out regional wall motion abnormalities suggestive of myocardial scarring or infarction. It is also helpful in ruling out and characterising valvular stenotic or regurgitant lesions.
This investigation should be carried out in patients with suspected structural heart disease as suggested by a history of coronary artery disease, myocardial infarction, or valvular heart disease requiring surgical correction. SCN5A mutations in LQT3 may also exhibit cardiomyopathy.[40]
Genetic testing
Determination of the patient's genotype is recommended for all patients with a high probability of congenital LQTS (Schwartz score ≥3.5).[5][41] For patients with an intermediate probability of congenital LQTS (Schwartz score 1.5 to 3), testing of established genes may be considered, mainly to help rule out a diagnosis.[5] Definitive disease-associated genes are currently KCNQ1, KCNH2, SCN5A, and CALM 1, 2, and 3; in patients with a high probability of congenital LQTS, CACNA1C and KCNE1 may also be considered.[5] For patients with defined syndromes, specific genes should be tested, for example KCNQ1 and KCNE1 in Jervell and Lange-Nielsen syndrome, or CACNA1C in Timothy syndrome.[5]
The identification of specific gene mutations enables:[5]
Pinpointing of the exact channelopathy responsible for the LQTS, thus identifying the subtype
Risk stratification of patients with congenital LQTS
Mapping of the mutation's inheritance so that family members can be screened
Initiation of gene-specific prophylactic treatment.
Genetic testing has a sensitivity of approximately 70% to 85% in index cases.[2][5] It requires expert interpretation, and can be costly.[5][42] In the absence of a family history of LQTS, it is not indicated for asymptomatic individuals with borderline QTc intervals (<480 ms). However, genetic testing is indicated when there is a very strong clinical diagnosis or when the QTc exceeds 500 ms on serial ECGs and a reversible cause is absent.[5][42]
Certain genetic subtypes are associated with particularly severe phenotypes that have a higher incidence of sudden cardiac death (such as KCNQ1-A341V or SCN5A-G1631D), whereas others are associated with milder disease.[5] Patients with multiple LQTS gene mutations are at higher risk for breakthrough cardiac events during follow-up.[43] Family members should have variant-specific genetic testing once a disease-causing variant has been identified in an index case. Early identification of affected family members is important, even in those with a normal baseline QTc, and genetic testing can be carried out in children from birth.[2][5]
In patients with acquired LQTS, genetic testing for defined disease-associated genes should be offered to those who experienced drug-induced torsades de pointes, are aged <40 years, and have a QTc interval >440 ms (males) and >450 ms (females) in the absence of the likely causative drug.[5] In these patients, a variant can be identified in >60% of cases.[5] Family screening is recommended for patients where a QT-prolonging drug is prescribed or being considered.[5]
European Society of Cardiology guidelines recommend that a diagnosis of LQTS is made in the presence of a pathogenic mutation, regardless of QT interval.[2]
Adrenaline (epinephrine) test
This test involves a catecholamine challenge with a brief infusion of adrenaline (epinephrine) and must be performed with immediate access to advanced life support and external defibrillation. It is not recommended by European guidelines due to low reproducibility.[2] However, it may be helpful in the diagnosis of LQT1 in which the QT interval and QTc increase more than those of the controls or LQT2 and LQT3 patients.[44]
Electrophysiology study
Investigating for inducible ventricular arrhythmias using electrophysiology studies has not been shown to have significant value in the diagnosis, treatment, or risk stratification of patients with LQTS.[2]
Use of this content is subject to our disclaimer