Tests
1st tests to order
CT angiogram
Test
CT angiogram (CTA) is the first-line investigation of choice when acute mesenteric ischemia is suspected and should be obtained early.[17][31][36]
CTA should be performed in the noncontrast, arterial, and portal venous phases (known as a "triple phase" scan).[17]
CTA provides evidence for the extent of bowel compromise from ischemia.[44][45] It also enables stratification of patients to identify those who would benefit from mesenteric angiography from those who require primary surgery.
It can also identify the underlying cause of ischemia, bowel complications, and other causes of acute abdominal pain.[17]
Presence of the thumbprinting sign, indicative of mucosal edema, suggests a worse prognosis.
CTA has replaced conventional angiography as standard practice for diagnosis of acute mesenteric ischemia.[31]
[Figure caption and citation for the preceding image starts]: CT scan: colonic thickening with pneumatosis intestinalisFrom the collection of Dr Jennifer Holder-Murray; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: 84-year-old man presenting with symptoms suggestive of ischemic bowel disease: (A) Abdominal CT revealing a massive circumferential and band-like air formation as intestinal pneumatosis (arrows) and pronounced edema of mesenteric fat (arrowhead) around necrotic bowel loops; (B) Another slice of abdominal CT showing long segmental pneumatosis of the small bowelLin I, Chang W, Shih S, et al. Bedside echogram in ischaemic bowel. BMJ Case Reports. 2009:bcr.2007.053462 [Citation ends].
[Figure caption and citation for the preceding image starts]: 84-year-old man presenting with symptoms suggestive of ischemic bowel disease: (A) Abdominal CT revealing a massive circumferential and band-like air formation as intestinal pneumatosis (arrows) and pronounced edema of mesenteric fat (arrowhead) around necrotic bowel loops; (B) Another slice of abdominal CT showing long segmental pneumatosis of the small bowelLin I, Chang W, Shih S, et al. Bedside echogram in ischaemic bowel. BMJ Case Reports. 2009:bcr.2007.053462 [Citation ends].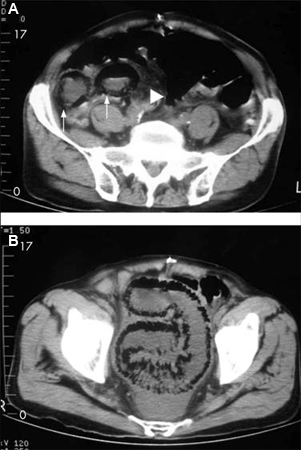 [Figure caption and citation for the preceding image starts]: CT scan: circumferential wall thickening of the transverse colon; white arrow shows thumbprintingFrom the collection of Dr Amir Bastawrous; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: CT scan: circumferential wall thickening of the transverse colon; white arrow shows thumbprintingFrom the collection of Dr Amir Bastawrous; used with permission [Citation ends].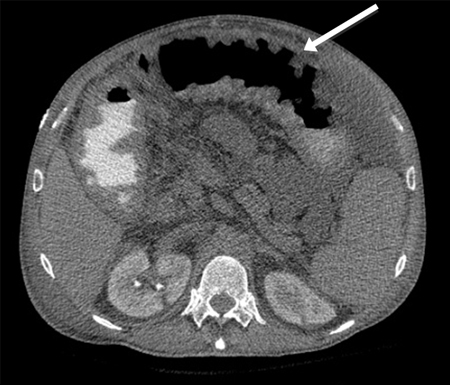 [Figure caption and citation for the preceding image starts]: CT angiogram: acute superior mesenteric artery thrombusFrom the collection of Dr Jennifer Holder-Murray; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: CT angiogram: acute superior mesenteric artery thrombusFrom the collection of Dr Jennifer Holder-Murray; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: CT angiography: 3-dimensional reconstruction with superior mesenteric artery stenosis from severe atherosclerotic plaque in a patient on follow-up imaging for endovascular aneurysm repairFrom the collection of Dr Jennifer Holder-Murray; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: CT angiography: 3-dimensional reconstruction with superior mesenteric artery stenosis from severe atherosclerotic plaque in a patient on follow-up imaging for endovascular aneurysm repairFrom the collection of Dr Jennifer Holder-Murray; used with permission [Citation ends].
Result
bowel wall thickening, bowel dilation, pneumatosis intestinalis, portal venous gas, occlusion of the mesenteric vasculature, bowel wall thickening with thumbprinting sign suggestive of submucosal edema or hemorrhage; may show the underlying cause of ischemia
CBC
Test
More than 90% of patients with acute mesenteric ischemia will have an abnormally elevated leukocyte count.[11]
May reveal anemia (often as a result of repeated episodes of melena) that exacerbates ischemia.
Result
leukocytosis, anemia, evidence of hemoconcentration
chemistry panel including CRP
coagulation panel, type and screen, cross match
Test
Sending a coagulation panel before treatment will aid in the diagnosis of any underlying coagulopathy as a risk factor for further thrombosis.[35] Allows correction of any clotting dyscrasia as part of treatment. Type and screen in preparation for the possibility of transfusion.
Result
underlying prothrombotic disorder
arterial blood gas/lactate level
Test
Metabolic acidosis is a common finding in patients with acute mesenteric ischemia.[11] Elevated serum lactate does not determine the presence or absence of ischemic or necrotic bowel; however, it can be used to assist with making the diagnosis and determining the severity.[11]
Result
acidosis, elevated lactate
ECG
Test
May demonstrate arrhythmias that predispose to cardioembolic complications, such as atrial fibrillation or atrial flutter, or acute infarction that may be the etiology of intestinal ischemia.
Result
atrial fibrillation, atrial flutter, acute myocardial infarction
erect CXR
Test
If perforation has occurred due to bowel necrosis, erect CXR may show subdiaphragmatic air. Immediate perioperative resuscitation, empiric intravenous antibiotics, and surgery are indicated if free air is identified.
Result
free air if perforation present
abdominal x-rays
Test
Abdominal x-ray has a limited role in the diagnosis and evaluation of acute mesenteric ischemia.[11][24] A negative radiograph does not exclude the diagnosis.[11] Plain x-rays are often normal early in the course of ischemia or when ischemia is mild. Abdominal x-ray is therefore not recommended in the diagnosis of intestinal ischemia.[11]
With worsening ischemia, plain x-rays may show formless loops of bowel, ileus, or thickening of the bowel wall with thumbprinting sign suggestive of submucosal edema or hemorrhage. [Figure caption and citation for the preceding image starts]: Plain abdominal x-ray: shows marked wall thickening of the transverse colon compatible with the finding of thumbprinting (white arrows)From the collection of Dr Amir Bastawrous; used with permission [Citation ends].
Result
formless loops of bowel, ileus, bowel wall thickening with thumbprinting sign suggestive of submucosal edema or hemorrhage
sigmoidoscopy or colonoscopy
Test
Sigmoidoscopy or colonoscopy with biopsy should be done within 48 hours to confirm the diagnosis of ischemic colitis.
In nongangrenous ischemic colitis, colonoscopy may show a highly specific sign - a single linear ulcer running longitudinally along the antimesenteric colon wall (colon single-strap sign). Nonspecific signs include erythema, fragility, edema of colon mucosa, scattered hemorrhagic erosions, scattered petechial hemorrhages with pale areas, bluish hemorrhagic nodule due to submucosal hemorrhages, and rarely mass-like lesion mimicking malignancy.
If urgent surgical intervention is required due to the condition of the patient, surgery should not be delayed to carry out sigmoidoscopy or colonoscopy.
[Figure caption and citation for the preceding image starts]: Colonoscopy: mucosal sloughing and likely nonviable colonFrom the collection of Dr Jennifer Holder-Murray; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Colonoscopy: denudation of colonic mucosaFrom the collection of Dr Jennifer Holder-Murray; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Colonoscopy: denudation of colonic mucosaFrom the collection of Dr Jennifer Holder-Murray; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Colonoscopy: demarcation between ischemic and normal colonFrom the collection of Dr Jennifer Holder-Murray; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Colonoscopy: demarcation between ischemic and normal colonFrom the collection of Dr Jennifer Holder-Murray; used with permission [Citation ends].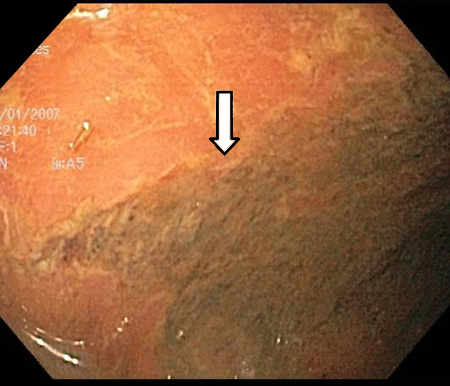
Result
mucosal sloughing or friability; mucosal petechiae; submucosal hemorrhagic nodules, erosions or ulcerations; submucosal edema; luminal narrowing; necrosis; gangrene
upper gastrointestinal endoscopy
Test
Can be used in patients with suspected chronic mesenteric ischemia to rule out alternative diagnoses involving the upper gastrointestinal tract, such as refractory ischemic gastric or duodenal ulcers.
Result
normal in patients with chronic mesenteric ischemia
Tests to consider
magnetic resonance angiography
Test
Magnetic resonance angiography (MRA) may have a role in making the diagnosis of chronic mesenteric ischemia.[31] However, CT angiography (CTA) is likely a better exam than MRA for the diagnosis of chronic mesenteric ischemia because of its capacity for higher resolution in combination with faster scans.
MRA may be considered with and without contrast if acute mesenteric ischemia is suspected.[17] However, compared with CTA, MRA is less likely to identify signs of ischemia such as pneumatosis or portal venous gas; the time required to perform an MRA exam, and the possible need for bowel stimulation with a meal, limit the usefulness of MRA in the diagnosis of acute mesenteric ischemia.[17]
Result
narrowing or obstruction of mesenteric vasculature; decreased bowel wall enhancement
mesenteric angiography
Test
Historically this has been the definitive test for diagnosing mesenteric ischemia. In current practice it is usually preceded by positive CT angiography in the acute setting. Sensitivity is 74% to 100%, specificity 100%.[32]
Occlusive ischemia demonstrates a proximal defect in the angiogram without distal filling of the mesenteric arcades.
Nonocclusive ischemia may cause vasoconstriction of all mesenteric arcades; mesenteric angiography can therefore diagnose nonocclusive mesenteric ischemia (NOMI) before infarction occurs. Four criteria are used for this purpose: narrowing of the origins of the superior mesenteric artery (SMA) branches, irregularities in these branches, spasm of the mesenteric arcades, impaired filling of the intramural vessels.
Mesenteric angiography enables treatment by infusion of vasodilators or thrombolytic agents (which have been shown to improve outcome). Often performed with the intention of proceeding to intervention.
For the diagnosis of chronic mesenteric ischemia due to atherosclerotic disease, angiography needs to demonstrate severe occlusion of at least 2 of the 3 splanchnic vessels, although in the absence of symptoms an abnormal angiography result alone is not sufficient for diagnosis.[36]
Result
proximal defect of a mesenteric vessel or vasoconstriction of all mesenteric arcades
mesenteric duplex ultrasound
Test
Particularly useful if obstruction is proximal in the mesenteric vessels, but ultrasound cannot assess distal mesenteric blood vessel flow and nonocclusive etiology of ischemia.[12] This is mostly used in vascular units for the assessment of chronic mesenteric ischemia, and is the first-line investigation of choice.[40]
Ultrasound of the bowel can be used to diagnose ischemic colitis (providing the user has adequate expertise) and differentiate between left- and right-sided disease.[41] It is an alternative for patients unable to tolerate contrast media.[35] However, it is not considered a routine investigation and should only be performed by a radiologist with sufficient ultrasound expertise.
Result
reduced or lack of blood flow through proximal mesenteric vessels
Emerging tests
abdominal near-infrared spectroscopy
Test
One meta-analysis of studies in newborns, which assessed the use of abdominal near-infrared spectroscopy (NIRS) as a marker of bowel ischemia in newborns, showed that NIRS accurately detects local tissue oxygenation mismatch, and can be used to monitor gastrointestinal oxygenation and detect bowel ischemia in this patient group.[43] Low gastrointestinal regional blood flow was consistently associated with bowel ischemia.[43] Further investigation is needed to confirm the utility of NIRS as a biomarker for bowel ischemia in adults.
Result
local tissue oxygenation mismatch, low gastrointestinal blood flow
Use of this content is subject to our disclaimer